The goals of palliative care are relief of suffering and improvement in quality of life for patients facing life-threatening illness. Such improvements are made through prevention, assessment, and treatment of pain and other symptoms and the provision of psychological, emotional, and spiritual support (
1 ). Palliative care is patient and family centered and emphasizes patient autonomy and advance planning for care. By 2003, 25% of U.S. hospitals sponsored a palliative care program (
2 ).
Patients become eligible for palliative care delivered by a hospice organization at the point they are expected to have less than six months of remaining life. The primary goals of hospice care are comfort and preservation of quality of life; cure of the terminal illness is no longer being pursued. Hospice care is delivered by an interdisciplinary cadre of physicians, nurses, social workers, and chaplains. Most often care is in patients' homes, but it also occurs in long-term care settings and, rarely, in inpatient hospice units. Although originally developed as an approach for patients with advanced cancer, currently over half of hospice enrollees in the United States have noncancer diagnoses. In 2007, 39% of all decedents in the United States were hospice enrolled before death (
3 ).
Hospice and palliative care are intuitively appealing for patients with both advanced cancer and chronic mental illnesses, such as schizophrenia. Little is known, however, about access, special needs, and barriers to palliative care for persons with chronic mental illness. End-of-life care is optimized when patients and their families participate in determining goals of care, yet half of patients with schizophrenia have impairments in decision-making capacity and when incapacitated, frequently lack surrogate decision makers (
4,
5 ). Home hospice requires the presence of a caregiver, most often a family member (
3 ).
Provision of palliative and hospice care can also be impeded by symptoms of schizophrenia, which impair development of a therapeutic alliance with medical providers, undermine motivation for advance care planning, and hinder communication about symptoms, including pain. Case reports document that some patients with schizophrenia do not acknowledge their cancer even when the malignancy reaches an advanced stage (
4,
6 ). If palliative goals of care are not explicitly communicated, patients may follow an antipalliative course, including terminal hospitalization and aggressive life-sustaining treatments, such as cardiopulmonary resuscitation (CPR).
We theorized that patients with schizophrenia and cancer may suffer disparities in end-of-life care because, in addition to the aforementioned potential barriers, there are disparities in their care at other stages of cancer treatment. For example, they are less likely to undergo preventive screenings for cervical, breast, prostate, and colorectal cancer, and several studies point to higher case fatality rates among patients with schizophrenia when cancer develops (
7,
8 ). The goal of this study was to compare measures of quality of end-of-life care among veterans with and without schizophrenia who died of cancer. We hypothesized that veterans with schizophrenia and advanced cancer, compared with those without major mental illness, would be less likely to complete advance directives, less likely to be enrolled in hospice, less likely to receive opioid medications before hospice enrollment, and more likely to die in the hospital without an order limiting CPR.
Methods
We used data from the data management system (DMS) of the U.S. Department of Veterans Affairs (VA) Northwest Health Network-Veterans Integrated Service Network (VISN) 20 (Oregon, Washington, and Alaska) to examine how cancer patients with schizophrenia are treated compared with cancer patients with no major mental illness. The DMS is a VISN-wide data repository that contains clinical information from each VA medical center (VAMC) in the northwestern United States, including demographic information, date of death, treatment dates, ICD-9 diagnoses, clinic appointments, and medications. We included veterans who died of cancer between January 1, 2003 (the date by which all VAMCs were required to have developed a palliative care team and to pay for hospice care for all veterans), and December 31, 2008. The study was approved as exempt from the need for written informed consent by the Portland VAMC Institutional Review Board.
Veterans were classified as eligible cases for study inclusion if they had an ICD-9 diagnosis of schizophrenia or schizoaffective disorder, had attended at least one mental health clinic outpatient appointment, and were prescribed an antipsychotic. A research psychologist (RS), manually reviewed the medical records to confirm the accuracy of the psychiatric diagnosis and cancer as a cause of death. The comparison group was randomly selected from approximately 14,000 veterans who died with cancer in VISN 20 during the same period but who had not been diagnosed as having a major mental illness (any psychotic disorder or bipolar disorder).
Information obtained from the DMS and from medical record review included demographic characteristics (age, sex, sites of care and death, and date of death), enrollment in and length of hospice care, prescription of any opioids in the last six months of life but before hospice enrollment, and presence of an advance directive or physician orders for life-sustaining treatment (POLST). The POLST is a set of regionally developed, portable, medical orders based on a patient's values for life-sustaining treatment (
9 ). The orders stay with the patient regardless of care setting and are most often used to limit life-sustaining treatments, artificially delivered nutrition, and even transport to the hospital. We also determined whether the patient's cancer was biopsy proven and whether the patient's cancer was treated with surgery or chemotherapy.
The groups were compared by Student's t test for continuous variables and chi square test for categorical variables with SPSS, version 17.0. All tests were two-tailed, and alpha was set at .05.
Results
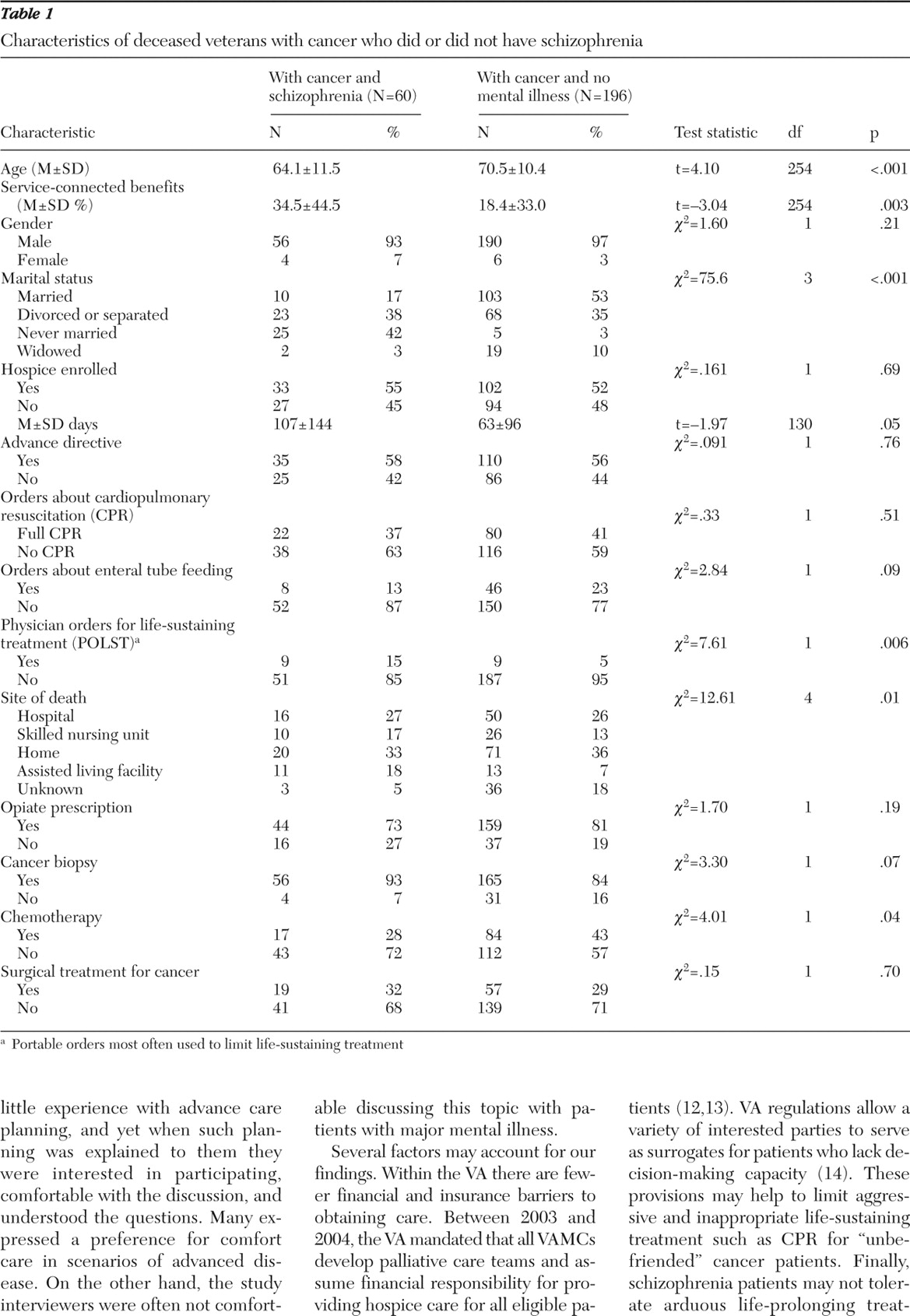
Sixty patients with schizophrenia or schizoaffective disorder who died of cancer were identified and compared with 196 cancer decedents without major mental illness. As expected with an older veteran population, the cohort was overwhelmingly male (
Table 11 ). Patients with schizophrenia who died of cancer were, on average, six years younger than patients in the control group and were significantly less likely to have ever been married. Race and ethnicity data are often missing in this database, and therefore this information was not collected.
None of our hypotheses predicting poorer-quality end-of-life care for patients with schizophrenia were substantiated. Fifty-eight percent of patients with schizophrenia had an advance directive, 73% were prescribed an opioid before hospice enrollment, and 63% had a physician order to forgo CPR. Only 27% of patients with schizophrenia died in the hospital, and over half (55%) were hospice enrolled. There were no differences between patients with schizophrenia and the comparison group on any of these measures. Some measures suggested that patients with schizophrenia had better end-of-life care than those without mental illness. They had longer hospice stays and were more likely to have a POLST documented. Patients with schizophrenia did not differ from the comparison group in the percentage who had biopsies or surgery for cancer, but they were significantly less likely to initiate chemotherapy (28% versus 43%, p=.04).
Discussion
We conducted a six-year, retrospective review of end-of-life care among veterans with cancer in the Northwest region of the United States. The main finding was that patients with schizophrenia received comparable or, on some measures, better end-of-life care than cancer patients without mental illness. In contrast, most studies indicate that patients with serious mental illness experience disparities in levels of cancer prevention and treatment.
A strength of our study is its breadth—it captured data from seven medical centers, including data for all veterans receiving active care in Oregon, Washington, and Alaska. A weakness is that we may not have had access to records from civilian hospitals, particularly for veterans without mental illness. We also may have excluded patients with schizophrenia who were transient, not adherent to their treatment, or not well integrated into the care system. Patients with schizophrenia were significantly younger than patients without mental illness. Finally, we might have demonstrated statistically significant differences with a larger sample.
Many case reports and commentaries outline the difficulties in caring for patients with schizophrenia and cancer, including patients' denial of having either disease, failure to seek care until cancer is advanced, uncooperativeness with and intolerance of cancer treatment, homelessness, and lack of family support (
4,
6 ). Foti and colleagues (
10,
11 ), in a study of 150 patients with serious mental illness, reported that most patients reported little experience with advance care planning, and yet when such planning was explained to them they were interested in participating, comfortable with the discussion, and understood the questions. Many expressed a preference for comfort care in scenarios of advanced disease. On the other hand, the study interviewers were often not comfortable discussing this topic with patients with major mental illness.
Several factors may account for our findings. Within the VA there are fewer financial and insurance barriers to obtaining care. Between 2003 and 2004, the VA mandated that all VAMCs develop palliative care teams and assume financial responsibility for providing hospice care for all eligible patients (
12,
13 ). VA regulations allow a variety of interested parties to serve as surrogates for patients who lack decision-making capacity (
14 ). These provisions may help to limit aggressive and inappropriate life-sustaining treatment such as CPR for "unbefriended" cancer patients. Finally, schizophrenia patients may not tolerate arduous life-prolonging treatments, such as chemotherapy, and may lack family support necessary for some cancer treatments. These patients may default earlier to less demanding comfort care, thus allowing longer hospice stays.
Conclusions
Our data indicate that characteristics of schizophrenia patients that might predict poor end-of-life care—impaired decision-making capacity, homelessness, poor social support, noncompliance with treatments, difficulty communicating symptoms, and more frequent denial of illness—do not undermine appropriate care in the context of institutional processes that support hospice and palliative care.
Acknowledgments and disclosures
This study was supported in part by the VA Health Services Research and Development Research Enhancement Award Program, Portland, Oregon. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the U.S. government.
The authors report no competing interests.