The University of Pennsylvania Institutional Review Board approved this study.
Conceptual model and rationale for included variables
Medicaid is the primary source of health care insurance for one in four children in the United States—approximately 26 million children were enrolled in each year of the study period (2002–2004). Although Medicaid is a federal program, states have considerable flexibility in whom they insure and what services they cover. Most Medicaid-enrolled children are eligible because their families' income is less than federally specified poverty levels. Children in foster care are automatically eligible for Medicaid. Most states have expanded Medicaid eligibility to include children of families with income as high as 300% of the poverty level. States also may cover children with disabilities that impair functioning; different states have different criteria for determining eligibility through this category, although the minimum standard is set by the federal Social Security Administration. Finally, states may determine that there is a group of children who frequently aren't covered by Medicaid or who require services traditionally not covered by Medicaid (for example, those with a specific diagnosis). The state can create a waiver to include these children and provide services that are traditionally not covered, using the argument that without these services, this group is at high risk of institutionalization. Forty-nine of 50 states use this mechanism to cover services for at least some children with disabilities; during the study period, five states had or were seeking a waiver specifically for children with autism (
12,
13 ).
It might be expected that this state-level variation in how Medicaid is used to cover services for children with disabilities would lead to variation in the quality of care they receive, including timely diagnosis. It is also possible that state-level variation is mediated by local health care resources. Other studies have found that local health care resources affect the identification of and delivery of care to children with autism (
14,
15,
16 ).
Local early intervention resources, generally paid for through the education system, also may affect timely identification of children with autism (
16 ). The needs of children with autism straddle the education and health care systems. Different jurisdictions have made different choices regarding how education and health care resources will substitute for or complement each other with regard to the identification and care of children with autism.
Age of diagnosis also may be consumer driven. Wealthier families or those with more information about child development may be more likely to notice deviations from usual behaviors and advocate for more timely evaluation (
9 ). Finally, children who are more severely affected may be noticed and diagnosed earlier.
Sample
The sample included all children meeting the following algorithm. First, only children younger than ten years were included (N=101,281) so that the results could be more readily compared with the ADDM Network study (
10 ). Second, children had to be Medicaid eligible for at least nine out of the 12 months preceding their first Medicaid claim associated with autistic disorder (
ICD-9 code 299 or 299.0x) or Asperger's disorder or pervasive developmental disorder not otherwise specified (
ICD-9 code 299.8x) (N=48,367). Nine of 12 months were required because of "administrative churning," in which families may lose benefits for as much as three months in a row because of administrative sanctions (
18 ). Because data were available starting January 1, 2001, the earliest diagnosis in the sample could occur on January 1, 2002. Third, children in the waiver program category were excluded, because of the high probability that these children were eligible because of their autism diagnosis and therefore had received the diagnosis before Medicaid enrollment (47,823 children not in the waiver category). Finally, within three months (one billing period) of the initial claims associated with an autism diagnosis, the child had to have a claim associated with both an autism diagnosis and a procedure code with a high probability of representing a diagnostic procedure. To identify these procedure codes, a complete list of procedure codes associated with a claim for autism services was created. All procedure codes associated with therapies, laboratory tests or X-rays, durable goods, or transportation or with missing definitions were removed from the list. By using this algorithm, a sample of 28,722 children with a first diagnosis of autism during the study period was identified. [A figure showing a graphical representation of the sample selection is available as an online supplement at
ps.psychiatryonline.org .] As a sensitivity analysis, a more restrictive sample of 14,876 children was identified where the first diagnosis of autism was associated with a procedure code in which the word "assessment," "evaluation," or "diagnosis" occurred. There was less than .2 months difference in observed age of diagnosis between these groups. Therefore, the larger sample was used.
Variables
Age of diagnosis was calculated as the difference between the date of the first claim associated with an autism diagnosis and the child's date of birth.
Children's demographic and clinical characteristics were abstracted from the Medicaid claims data and included sex, race and ethnicity (African American, Asian, Latino, white, or other race or ethnicity), diagnosis (autistic disorder versus other pervasive developmental disorder), and reason for Medicaid eligibility (disability, foster care, poverty, or other reason).
Education characteristics included county-level education expenditures (calculated as [total expenditures - total capital outlay)] ÷ total number of students) and pupil-teacher ratio. The number of children served in the early intervention system was included as a state-level variable because that information is not available at the county level. It was hypothesized that counties that invest more resources (that is, money or staff) into the education system would also conduct most of their identification of autism through this system. This may ultimately increase the treated prevalence of autism within that county; however, children identified through the Medicaid system may therefore be identified later than in other counties because they may represent children who are missed by the education system. On the other hand, greater educational resources may increase the incentive for earlier identification of children with disabilities so that they can benefit from these services.
Health care resources included the per capita number of pediatricians and pediatric specialists (child psychiatrists, neurologists, occupational therapists, audiologists, physical therapists, speech-language pathologists, speech therapists, and psychologists). These data were based on work addresses captured by the relevant professional organizations and included in the ARF. It was hypothesized that greater pediatric health care capacity would result in earlier diagnosis.
Demographic characteristics of county residents included the median income, percentage of white residents, percentage of residents aged from birth through less than ten years of age, and urbanicity. Urbanicity was initially coded on the basis of nine categories available in the ARF: The first category was counties of metropolitan areas of one million population or more. The second was counties in metropolitan areas of250,000 to one million population. The third was counties in metropolitan areas of fewer than 250,000 population. The fourth was urban population of 20,000 or more, adjacent to a metropolitan area. The fifth was urban population of 20,000 or more, not adjacent to a metropolitan area. The sixth was urban population of 2,500–19,999, adjacent to a metropolitan area. The seventh was urban population of 2,500–19,999, not adjacent to a metropolitan area. The eighth was completely rural or less than 2,500 urban population, adjacent to a metropolitan area. The ninth was completely rural or less than 2,500 urban population, not adjacent to a metropolitan area. To facilitate comparisons, these nine categories were recoded into four categories: counties of metropolitan areas of one million or more (code 1), counties in metropolitan areas of fewer than one million (codes 2 and 3; referred to as "suburban"), urban areas (codes 4, 5, 6, and 7), and rural areas or areas less than 2,500 urban population (codes 8 and 9).
The percentage of white residents has been associated with autism treatment decisions (
15 ) and may affect age of diagnosis because it could act as a proxy for greater resources or health care provider bias, in that clinicians may be more likely to screen for autism in a predominantly white population (
19 ). Urbanicity also has been associated with autism identification (
16 ). Larger population is associated with proximity to tertiary care medical centers and greater absolute number of cases of autism, which may increase familiarity with the presentation of the disorder.
Statistical analysis
The purpose of the analysis was to examine the age of diagnosis of autism and its association with various child and county characteristics and to examine trends in age of diagnosis during the study period. To facilitate comparisons among strata of each variable and to avoid the assumption of linear relationships between variables, county characteristics were categorized by quartile. The exceptions were the number of pediatricians, which was categorized as none and then as a median split of the remaining counties (low versus high), and the number of pediatric specialists, which was categorized as any versus none.
Age of diagnosis was modeled using linear regression models with random effects for county and state. Trends in age of diagnosis were examined by adding year of diagnosis to the statistical model. We tested for interactions, without adjustment for multiple comparisons, among all child-level variables to determine whether the annual trends varied among levels of different child characteristics. Significant interactions were included in the final model. Covariate effects were reported in terms of the predicted mean age of diagnosis, associated standard error, and p values from the omnibus test across categories. Adjusted estimates were computed from the final model with other covariates centered at their mean value.
To estimate the total explainable variance at each level of this multilevel analysis (individual, county, and state), we estimated a pseudo-R
2 from the variance components and the intraclass correlation at each level in the null model (with no fixed effects added). To estimate the amount of explainable variance accounted for at each level by the variables at that level, we ran three regressions; in each regression, we entered sets of variables only at one level (that is, one model for child characteristics, one model for county characteristics, and so on) and calculated the percentage change in the pseudo-R
2 from the pseudo-R
2 in the null model. This percentage change quantifies the proportion of outcome variation explained by observed covariates (
20 ).
Results
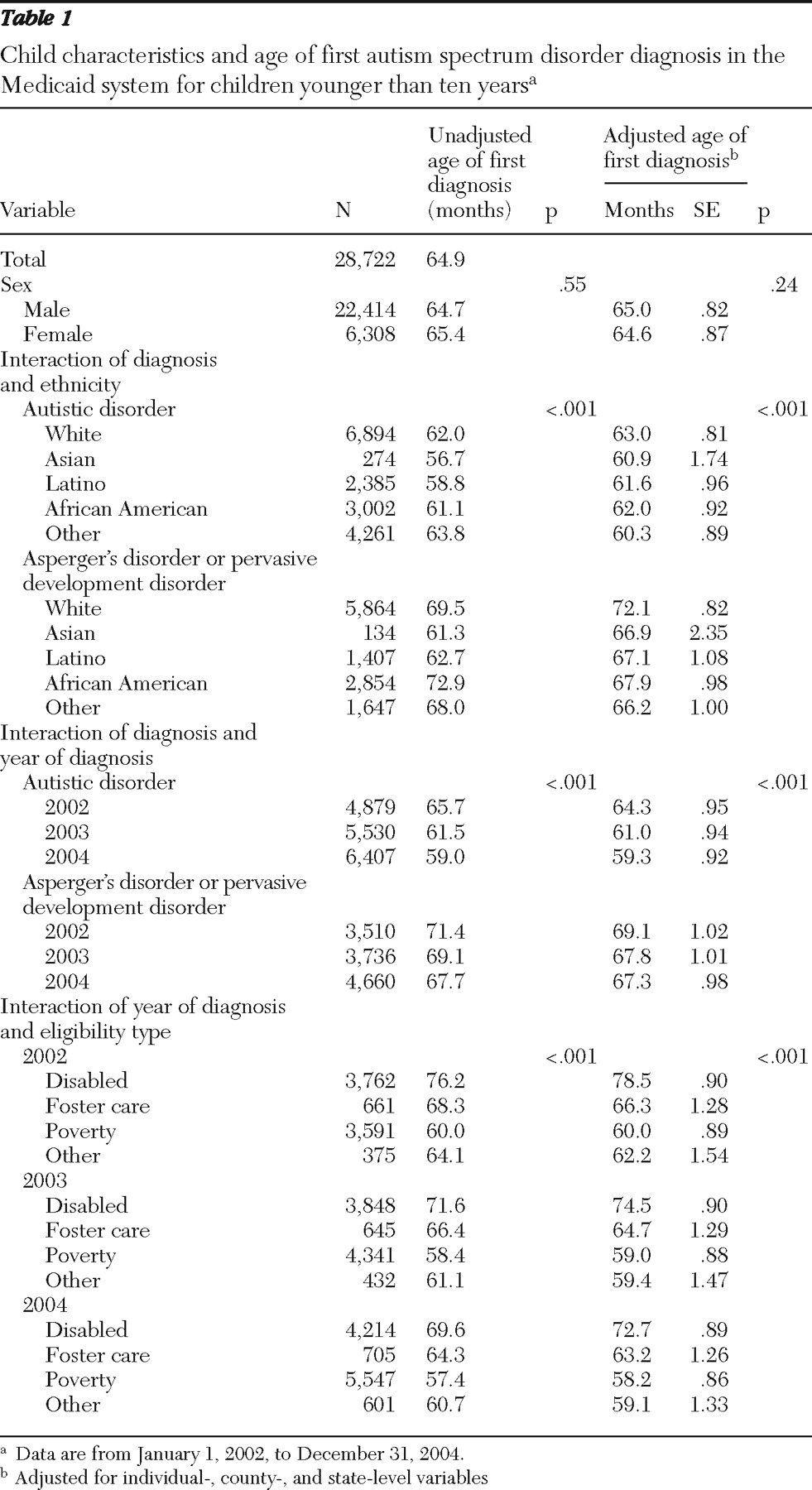
We identified 28,722 children with newly diagnosed autism in the Medicaid rolls from January 1, 2002, to December 31, 2004. Their average age of diagnosis was 64.9 months.
Table 1 presents the bivariate and adjusted associations between each child-level variable and age of diagnosis. In the adjusted analysis, the average age of diagnosis during the study period dropped 5.0 months for autistic disorder and 1.8 months for other spectrum disorders. Compared with other racial and ethnic groups, Asian children were diagnosed as having autistic disorder at a younger age (60.9 months) and white children were diagnosed at an older age (63.0 months). The difference across ethnic groups was more pronounced for other spectrum disorder diagnoses, with Asian children diagnosed at an average of 66.9 months and white children diagnosed at an average of 72.1 months. In 2002 (the first year of the study), children who were Medicaid eligible through the disability program category were diagnosed 18.5 months older, on average, than children eligible through the poverty category. This difference decreased to 14.5 months in 2004.
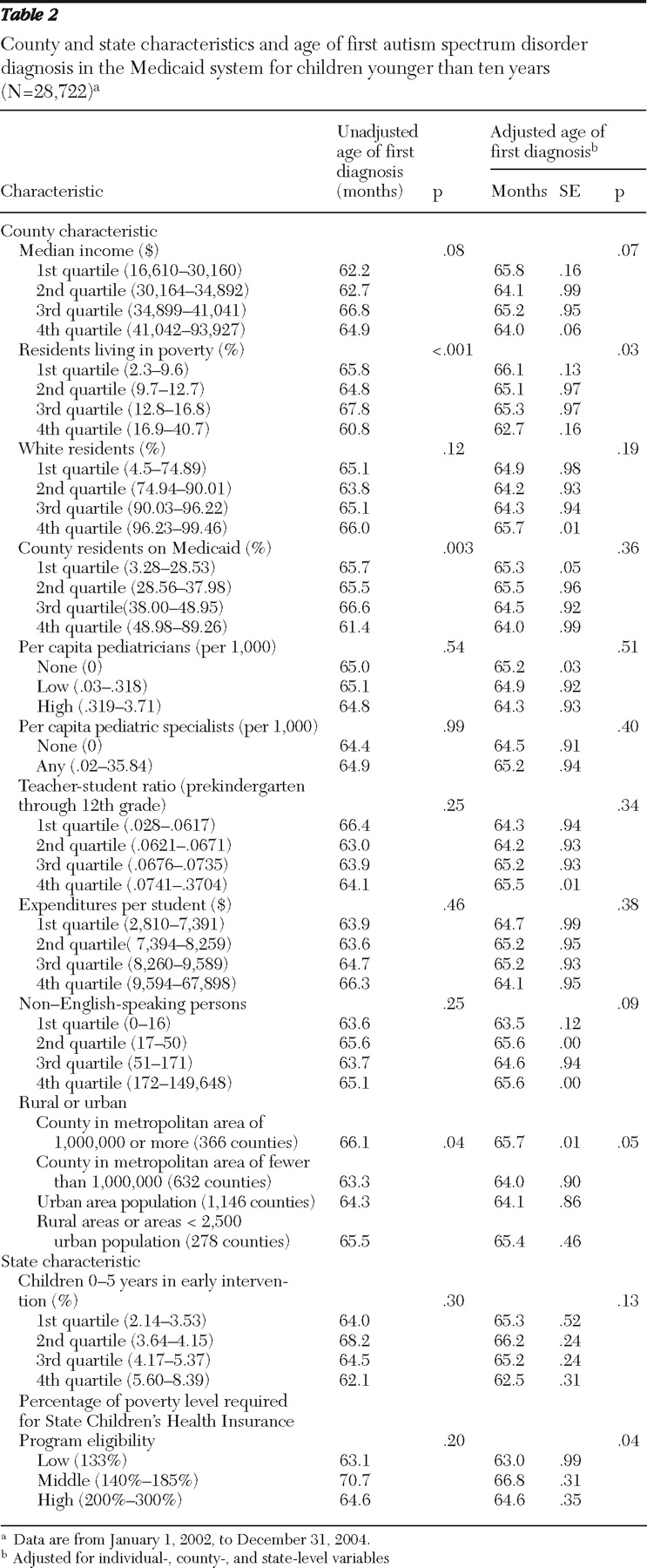
Table 2 presents the bivariate and adjusted associations between county- and state-level variables and age of diagnosis. At the county level, increased proportion of impoverished county residents and living in a suburban county (as opposed to an urban or rural county) were associated with earlier age of diagnosis. States with the most stringent criterion for the State Children's Health Insurance Program, insuring children only up to 133% of the poverty level, had the lowest age of diagnosis, on average, whereas states in the middle range (insuring children between 140% and 185% of the poverty level) had the highest age of diagnosis.
The variance calculations estimated that 96% of the explainable variation in age of diagnosis is at the child level; adding the county level accounted for an additional 3%, and adding the state level accounted for another 1%. The child-level variables included in the model explained 9% of explainable variation at the child level in age of diagnosis. The county-level variables explained 16% of the variation across counties. The state-level variables explained 23% of the variation across states.
Discussion
Our study found that among Medicaid-enrolled children in the United States from 2002 to 2004, the average age of diagnosis of autism was 64.9 months, remarkably similar to the 68.4 months that Shattuck and colleagues (
10 ) reported from using 2002 data from the ADDM Network, although the Shattuck study included children who met case criteria but did not have a diagnosis of autism in their records, which may have inflated their estimate of age of diagnosis. Even among children with autistic disorder, our study found that the average age of diagnosis was 59.3 months in 2004, confirming that for most children with autism in the United States, diagnosis occurs years later than it should (
6 ). The average age of diagnosis differed by important sample characteristics and changed differentially by these characteristics over time.
The five-month drop in the average age of autistic disorder diagnosis over the three-year study period is encouraging and suggests greater awareness, perhaps fueled by campaigns conducted by the CDC and other organizations during the study period (for example,
www.cdc.gov/ncbddd/actearly/index.html ). Small differences in age of treatment entry may be important, because observational studies point to improved outcomes for children who, for example, enter treatment at three years of age instead of four years (
21,
22 ).
The decrease in age of diagnosis over time was significant only among children with autistic disorder. Other spectrum disorders comprise both Asperger's disorder and pervasive developmental disorder not otherwise specified; previous research showed that although the age of diagnosis of pervasive developmental disorder not otherwise specified is decreasing, older children increasingly are diagnosed as having Asperger's disorder (
9 ). The smaller change over time for other spectrum disorders may therefore result from two countervailing trends: one for a decreasing age of diagnosis for pervasive developmental disorder not otherwise specified and the other for increased average age of diagnosis for Asperger's disorder. A second interpretation is that awareness of the symptoms of autistic disorder is increasing, but much work is left to do regarding the more subtle indications for other spectrum disorders.
The differences in age of diagnosis among ethnic groups are difficult to interpret in light of previous research on health disparities. For example, other studies have suggested late or underdiagnosis among Latino children (
16,
19,
23 ), whereas we found that Latino and Asian children were diagnosed earlier than children in other racial or ethnic groups. Similarly, our study found that children in poorer counties were diagnosed earlier, on average. It may be that in an impoverished sample such as this one, racial- and ethnic-related health disparities are ameliorated. It may also be that only the most severely impaired children within some racial or ethnic groups or in poor counties are identified, with other children missed altogether, decreasing the observed age of diagnosis for that group. This hypothesis is supported by a study that used the same data as Shattuck and colleagues (
10 ) and found that children with autism from racial or ethnic minority groups were less likely than white children to be diagnosed (
19 ). Further support comes from the finding in the study presented here that the racial and ethnic difference in age of diagnosis was much less for children with autistic disorder (most likely more severely affected) than for children with other spectrum disorders, for which more variability in presentation may be observed.
Children who were eligible for Medicaid through the disability category were diagnosed much later than other children. Many states have expanded Medicaid eligibility to include children with autism, regardless of family income. The age of diagnosis in the disability category may represent age of Medicaid-reimbursed treatment entry, with diagnosis occurring earlier in another system. A second hypothesis is that children in the disability category are multiply impaired. The amelioration of the difference over time in age of diagnosis between children in different eligibility categories may again relate to clinicians' more sophisticated understanding of the presentation of autism and associated comorbidities.
Contrary to studies examining factors associated with autism treatment (
15 ), few county- or state-level variables were significantly associated with age of diagnosis. In fact, the multilevel analysis of variance suggested that most of the variation in age of diagnosis was associated with child-level differences. This finding may have important implications for designing interventions to reduce age of diagnosis, which perhaps should focus more on increasing parental and clinician awareness, rather than changing policy. Two caveats to this interpretation should be considered: first, although Medicaid eligibility was entered into the model as a child-level variable, program eligibility is determined by both child characteristics and state practice. Therefore, there may be cross-level interactions (that is, child characteristics and state policies) that could not be tested in this model. Second, one should use caution in placing emphasis on the estimates of proportion of variance explained. There is still debate in the literature on the most appropriate statistic for linear mixed models (
20 ). Replication and careful study in other data sets are warranted before this hypothesis is accepted.
At least four study limitations should be mentioned; first among them is that the autism diagnosis in the Medicaid claims has not been validated. Although its accuracy has not been examined specifically, Fombonne and colleagues (
24 ) found 97% positive predictive value for chart diagnoses and a diagnosis of autism administered by a trained research team, and Yeargin-Allsopp and colleagues (
25 ) found that 98% of children with a chart diagnosis met research criteria for autism. Other studies have found good correspondence between psychiatric diagnoses in the claims and those in the charts (
26 ). Taken together, these findings suggest acceptable validity of the diagnosis of autism in the Medicaid claims. A second limitation is that, as with any study relying on a diagnosed group, this study did not include those who were diagnosed very late or not at all. Previous CDC findings suggest that the age group we selected represents the overwhelming majority of individuals who ever will receive the diagnosis (
25 ). With our new sample selection strategy, we also missed most individuals who were diagnosed in inpatient or residential settings (these providers rarely submit procedure codes) and those diagnosed in health care markets in which specific procedure codes may not be required. A third limitation is that children may have received a diagnosis of autism outside the Medicaid system before initiating Medicaid-reimbursed treatment. Other studies have found that many children receive their first autism diagnosis in the education system (
10 ). We attempted to capture this by identifying children eligible through the disability category of Medicaid, which may indicate that they were Medicaid eligible because of their autism or a related impairment; overall this limitation may have artificially inflated the observed age of diagnosis. Finally, the analysis did not include other county variables (for example, autism-specific diagnostic resources or information about other systems that provide diagnostic services) that may be related to age of identification in the Medicaid system. On a related note, the geographic unit of analysis more relevant than county may be school district, because even within a given county, there may be substantial differences in resources and practices among the districts.