Between 7% and 13% of Medicaid beneficiaries use mental health or substance abuse services in any year (
1,
2 ). This use is concentrated among individuals who qualify for Medicaid on the basis of disability, about one-third of whom have psychiatric conditions (
3,
4 ). Because Medicaid plays a critical role in financing mental health and substance abuse services, especially for beneficiaries with disabilities, knowing the characteristics and service use patterns of beneficiaries who use these services is useful for establishing policy priorities, designing new programs, and tracking their effects (
5 ).
Using data that are more recent and from more states than in previous reports (
3,
4,
6 ), we describe characteristics of Medicaid beneficiaries who use mental health or substance abuse services, identify their use of selected health services, and compare it with that of other beneficiaries. The study addresses two specific questions: What are the demographic and diagnostic characteristics of Medicaid beneficiaries who use mental health or substance abuse services? And how does their use of psychotropic medications, inpatient care, and emergency services compare with that of other beneficiaries?
Methods
Overview of data
This study was based on data from the 2003 Medicaid Analytic eXtract (MAX) files, a system that contains data on beneficiaries, service use, prescription drugs, and expenditures in state Medicaid programs. Except for claims involving prescription drugs, each claim contains codes indicating a primary diagnosis from the
ICD-9-CM and the type of service that generated the claim. We used these codes to identify treatment settings (such as emergency rooms) and to distinguish psychiatric from general hospitals. Data entered into the MAX files undergo extensive quality reviews (
7,
8 ). Data from 2003 were the most recent MAX data available at the start of the study.
We used fee-for-service Medicaid claims because such claims yield more detailed and complete information about service use than encounter data submitted by managed care organizations. Because of potential problems with data from managed care plans, we excluded states where more than 33% of the state's Medicaid beneficiaries were enrolled in such plans. With respect to states where capitated managed care penetration was 33% or less, we excluded those that failed to meet specific data quality standards, such as by having unacceptable rates of missing data (
9 ).
Thirteen states met all data standards for variables pertinent to this study. For these 13 states, we excluded beneficiaries who were enrolled in any capitated comprehensive or behavioral managed care plan for the entire year. For beneficiaries enrolled in both fee-for-service and managed care systems during 2003, we excluded data for months of managed care enrollment. Overall, in the 13 study states, 86.6% of data for all eligible months were from fee-for-service systems, compared with 50.9% of data in other states.
The 13 states that met study criteria were Arkansas, Georgia, Idaho, Illinois, Indiana, Kansas, Maine, Montana, North Carolina, South Carolina, Texas, Vermont, and Wyoming. These states include 12.9 million beneficiaries (23% of all 55.8 million beneficiaries enrolled in Medicaid for any time in 2003). The percentage of the fee-for-service Medicaid population using mental health or substance abuse services in 2003 varied slightly between the 13 states and all other states (11.7% compared with 11.1%). Gender, racial, and eligibility group distributions in the 13 study states were similar to those in all states. However, beneficiaries residing in the 13 states were more likely to be under 22 years old (62%, compared with 54% for all states). Extensive data on state variation with respect to beneficiary characteristics and coverage of mental health services and substance abuse treatment are available elsewhere (
9 ). Researchers may wish to use this information to examine the implications of state variation for service use.
Study population
The study included all Medicaid beneficiaries enrolled in fee-for-service Medicaid in the selected states for at least one month in 2003, including those eligible for limited or restricted benefits. We identified the group of beneficiaries using mental health or substance abuse services in two ways. First, we selected beneficiaries with any claim for inpatient psychiatric care in a psychiatric hospital, an institution for mental disease (IMD), or a psychiatric residential treatment facility. Second, we selected individuals who had any Medicaid claim with a primary ICD-9-CM diagnosis code for a mental or substance use disorder, including schizophrenia (295.x), major depression and affective disorders (296.x), other psychoses (297.x or 298.x), childhood psychoses (299.x), neurotic and other depressive disorders (300.x or 311.x), personality disorders (301.x), other mental disorders (302.x, 306.x, or 310.x), special symptoms and syndromes (307.x), stress and adjustment reactions (308.x, 309.x), conduct disorders (312.x), emotional disturbances (313.x), attention-deficit hyperactivity disorder (ADHD or hyperkinetic syndrome, 314.x), and mental disorders associated with childbirth (248.4).
ICD-9 codes used to identify beneficiaries who had substance use disorders were alcoholic psychoses (291.x), alcohol dependence or nondependent abuse (303.x or 305.x), drug psychoses (292.x), drug dependence or nondependent abuse (304, 305.2–305.9, or 965.0), and substance abuse associated with childbirth (648.3, 760.71, or 779.5).
Although mental and substance use disorders often co-occur, we identified beneficiaries as having used either mental health services or substance abuse treatment on the basis of the most frequently occurring condition. This approach prevented double-counting of service use by individuals with both conditions but may have underidentified the number of beneficiaries using substance abuse treatment (
4 ). Beneficiaries were identified on the basis of claims from traditional behavioral health providers (for example, community mental health centers) as well as other providers (for example, internists).
Procedures and variable definitions
After obtaining a data usage agreement from the Centers for Medicare and Medicaid Services (CMS), we created a new person-level file for beneficiaries meeting inclusion criteria. Summary variables showing each beneficiary's service use during eligible months were constructed by repeated runs through the MAX files to find all claims associated with the beneficiary. Each claim was classified as being for mental health treatment, substance abuse treatment, or other treatment, as indicated by the claim's type of service or primary diagnostic code. We used CMS mainframe computers to conduct the analyses and adhered to all confidentiality and security provisions specified in the agreement.
Beneficiary age was defined as the age of the beneficiary on December 31, 2003. Individuals whose ages are unknown accounted for .004% of beneficiaries in the study states and were excluded from tables that include this variable. Gender was not reported for about .02% of beneficiaries in the study states; 3.7% of records lacked race or ethnicity data.
Four mutually exclusive Medicaid eligibility groups (disabled, aged, adults, and children) were identified on the basis of how individuals qualified for Medicaid according to state records. The disabled category included beneficiaries of all ages who met federal or state definitions of disabled, blind, or chronically ill. The aged category included beneficiaries aged 65 and over, some of whom may have been disabled but did not qualify for Medicaid on the basis of disability (and hence are not in the disabled category). A few individuals in this category may be dependent spouses under age 65. Adults included all nondisabled beneficiaries aged 22 to 64 and beneficiaries under 18 if determined to be head of household. Children included State Child Health Insurance Program beneficiaries in ten of the 13 states covered in this study (excepting Kansas, Texas, and Wyoming). Some children in the child category may have been disabled but did not qualify for Medicaid on that basis.
Each claim for a prescription psychotropic drug was placed into one of four therapeutic classes (antidepressants, antipsychotics, anxiolytic agents, and stimulants) using drug classification software from the Master Drug Data Base (Medi-Span, v2.0).
Results
Characteristics of the study population
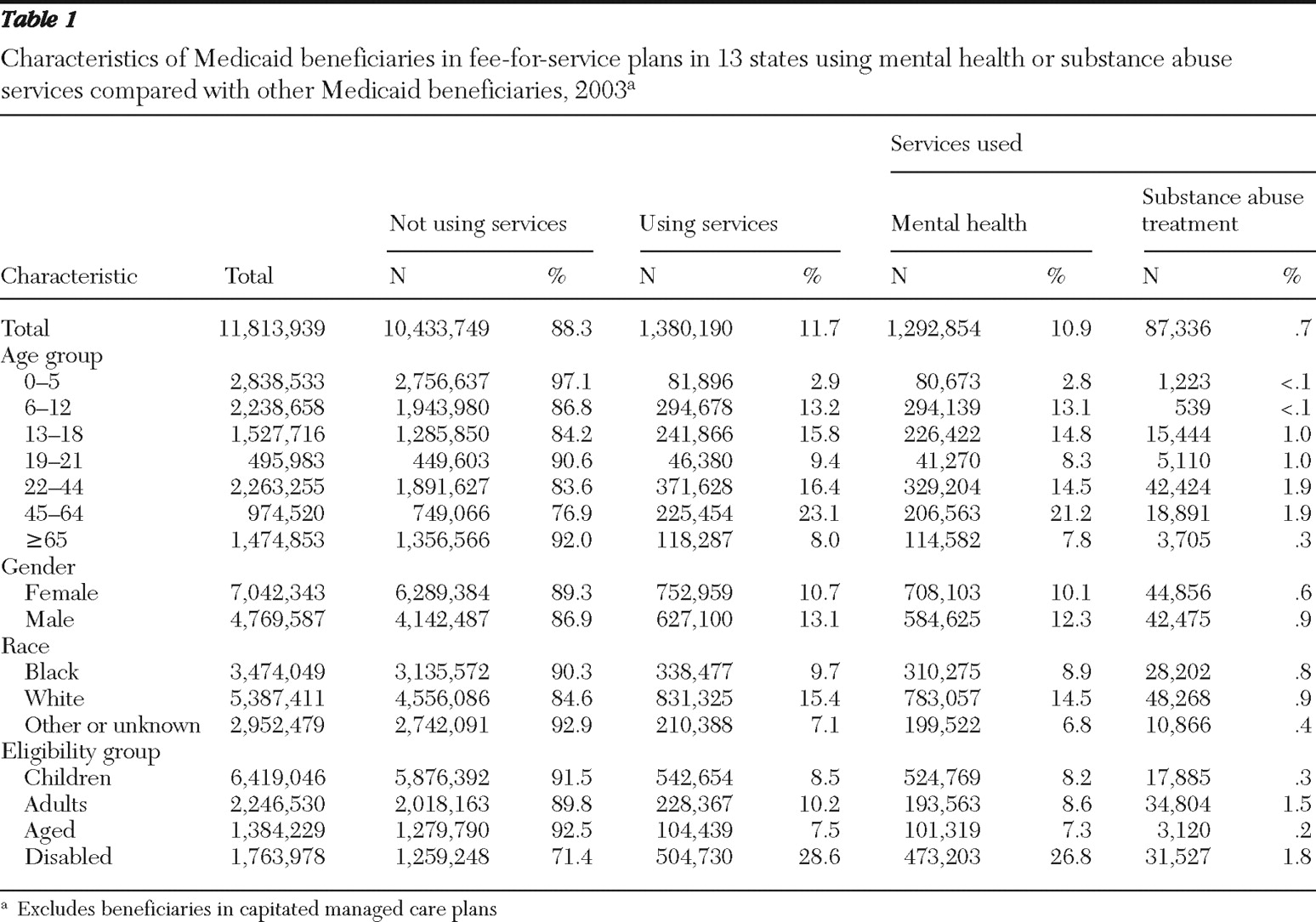
In the 13 study states in 2003, 10.9% of fee-for-service Medicaid beneficiaries were identified as using mental health services and .7% as using substance abuse treatment (
Table 1 ). The proportion of beneficiaries so identified varied by age, race, and eligibility group. Overall, of beneficiaries who were eligible for Medicaid on the basis of disability, 26.8% and 1.8% used mental health or substance abuse services, respectively. The proportion of beneficiaries who used these services was largest in the 45–64 age group.
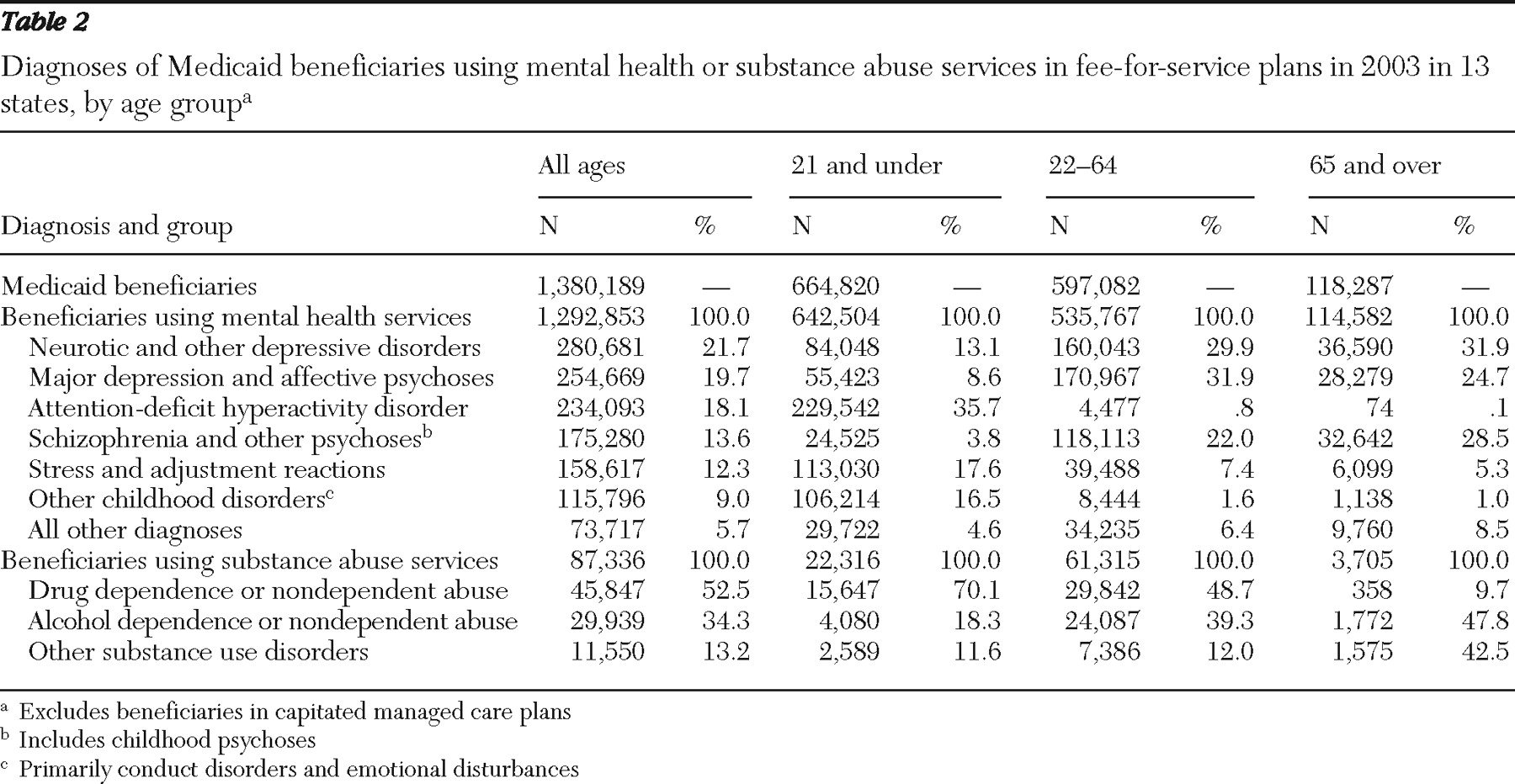
The most frequently occurring diagnosis varied across age categories (
Table 2 ). ADHD was the most common mental disorder among beneficiaries under 22 (diagnosed in 35.7% of this age group). Major depression and affective psychoses (31.9%), neurotic and other depressive disorders (29.9%), and psychotic disorders including schizophrenia (22.0%) were common mental disorders among beneficiaries aged 22–64 years. In the 65-and-older age group, neurotic and other depressive disorders were the most common mental disorders (31.9%), followed by schizophrenia and other psychoses (28.5%), and major depression and affective disorders (24.7%). Of beneficiaries using substance abuse services, about half (52.5%) were diagnosed as having drug dependence or nondependent drug abuse; again, diagnoses varied by age group.
Use of psychotropic medications
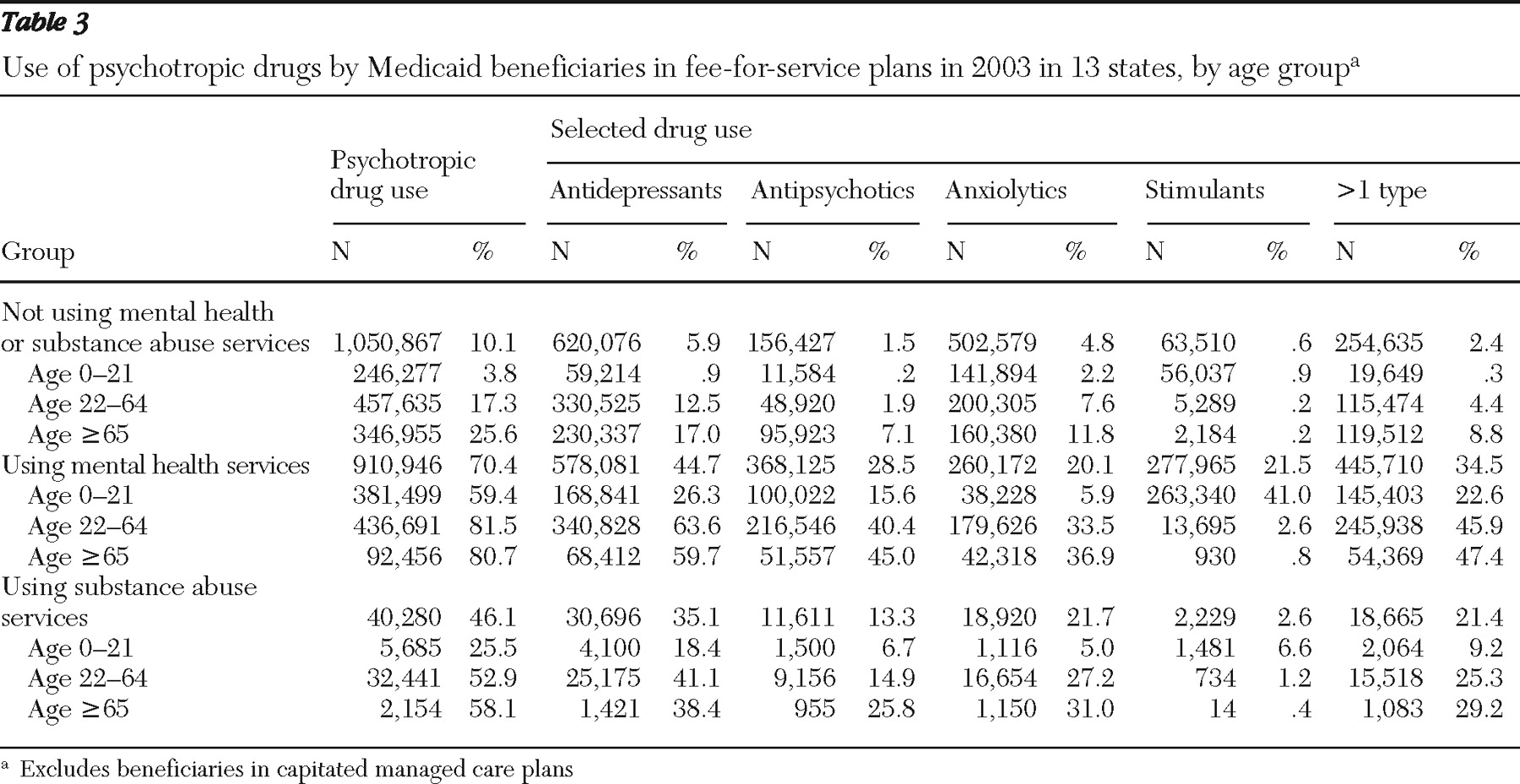
Among beneficiaries using mental health services, 70.4% were prescribed psychotropic drugs and 34.5% were prescribed more than one class of drug during the year (
Table 3 ).
Prescription patterns varied markedly according to diagnosis and age category. Of beneficiaries using mental health services who were aged 21 and under, 59.4% received prescriptions for psychotropic medication, and 22.6% used more than one class. The most common drugs for beneficiaries under age 22 were stimulants (prescribed for 41.0% of beneficiaries in this age group) and antidepressants (prescribed for 26.3%). More than 80% of beneficiaries in the other two age groups who used mental health services received a prescription for a psychotropic drug during 2003, and nearly half used more than one class.
Among beneficiaries using substance abuse services, 46.1% were prescribed psychotropic drugs and 21.4% were prescribed multiple classes of these drugs. About one-quarter (25.5%) of beneficiaries 21 years and under, and slightly more than half (52.9%) of those 22–64 used these drugs.
Within the group of beneficiaries who did not use mental health or substance abuse services in 2003, 10.1% filled a prescription for some type of psychotropic drug (data not shown). Use of psychotropic drugs in the absence of a qualifying diagnosis was most common among those aged 65 years and older (25.6%). Antidepressants were prescribed for 17.0% of beneficiaries in this group, antianxiety drugs for 11.8%, and antipsychotics for 7.1%.
Inpatient treatment for mental illness or substance use disorders
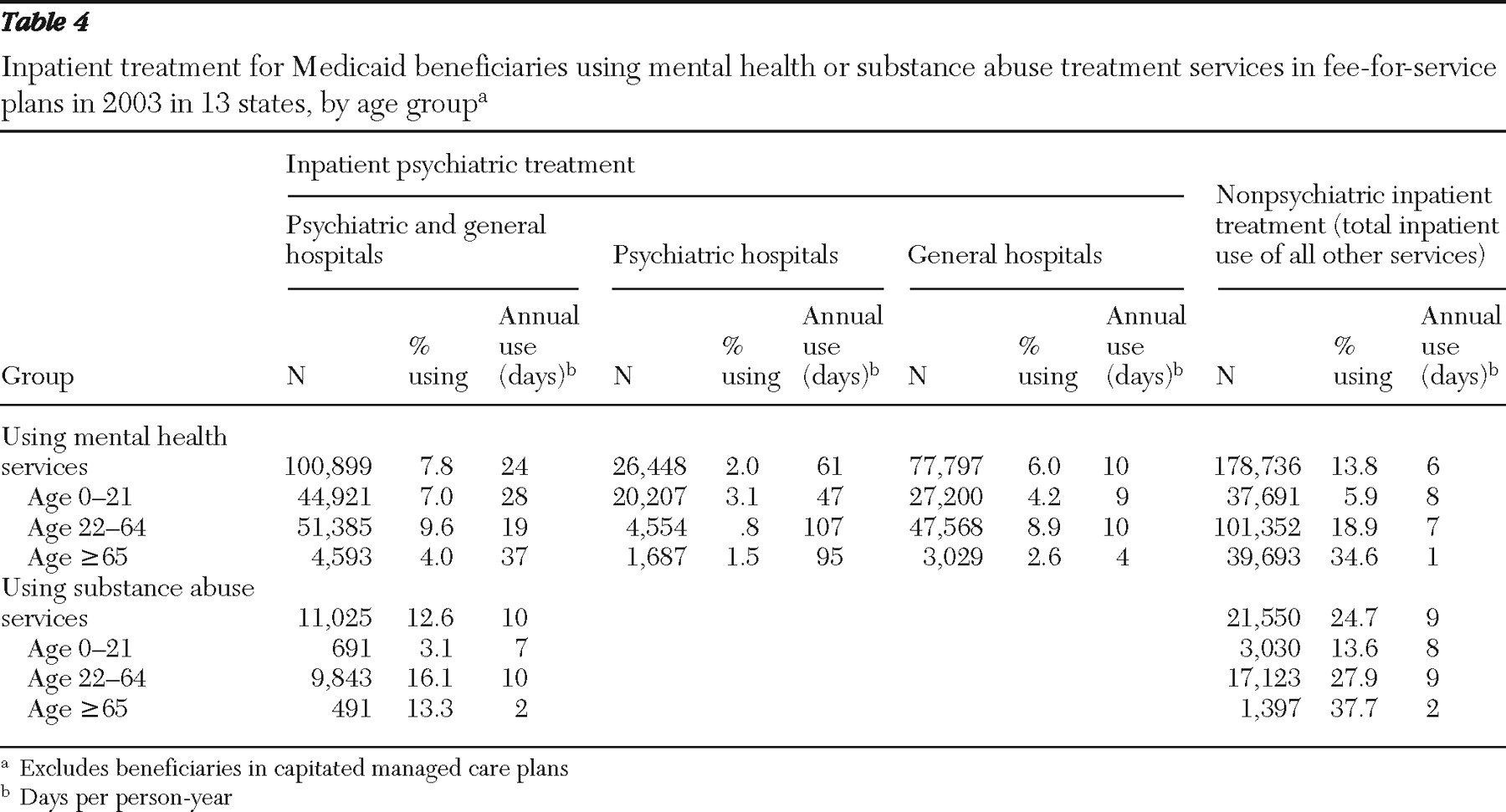
Of beneficiaries using mental health services in the 13 study states in 2003, 7.8% received inpatient treatment in psychiatric or general hospitals (
Table 4 ): 2.0% received treatment in psychiatric hospitals and 6.0% in general hospitals. On average, these beneficiaries stayed far longer in psychiatric hospitals (61 days) than they did in general hospitals (ten days).
Despite federal exclusion of IMD costs (
10 ), a small percentage of Medicaid beneficiaries aged 22 to 64 (.8%) had stays in psychiatric hospitals (possibly because patients turned 22 while residing in these settings), but most utilization within this age group (8.9%) was in general hospitals. Inpatient treatment for mental disorders was least frequent among beneficiaries aged 65 and over (4.0%); inpatient stays in psychiatric hospitals for this group averaged 95 days.
Among beneficiaries using substance abuse services, 12.6% used inpatient settings for treatment of their disorder and stayed for an average of ten days; differences between age groups were substantial. Inpatient stays for substance use disorders were most common among those aged 22 to 64 years (16.1%) and least common among those aged 21 years and under (3.1%).
Other inpatient treatment
Within the group of beneficiaries using mental health services, 13.8% received treatment in inpatient settings other than mental health treatment settings, staying an average of six days (
Table 4 ). Almost one-quarter of beneficiaries using substance abuse services (24.7%) received treatment in these other settings, staying an average of nine days. Beneficiaries aged 65 years and over who used mental health or substance abuse services were most likely to have an inpatient stay for treatment of a condition other than their mental or substance use disorders, reflecting the overall increase in inpatient treatment for the elderly population. Average annual stays appear low because Medicare likely covered many inpatient costs in this age group.
Overall, 12.7% of beneficiaries who did not use mental health or substance abuse services received inpatient treatment in 2003, staying an average of six days (data not shown). This treatment was, by definition, for conditions other than mental or substance use disorders.
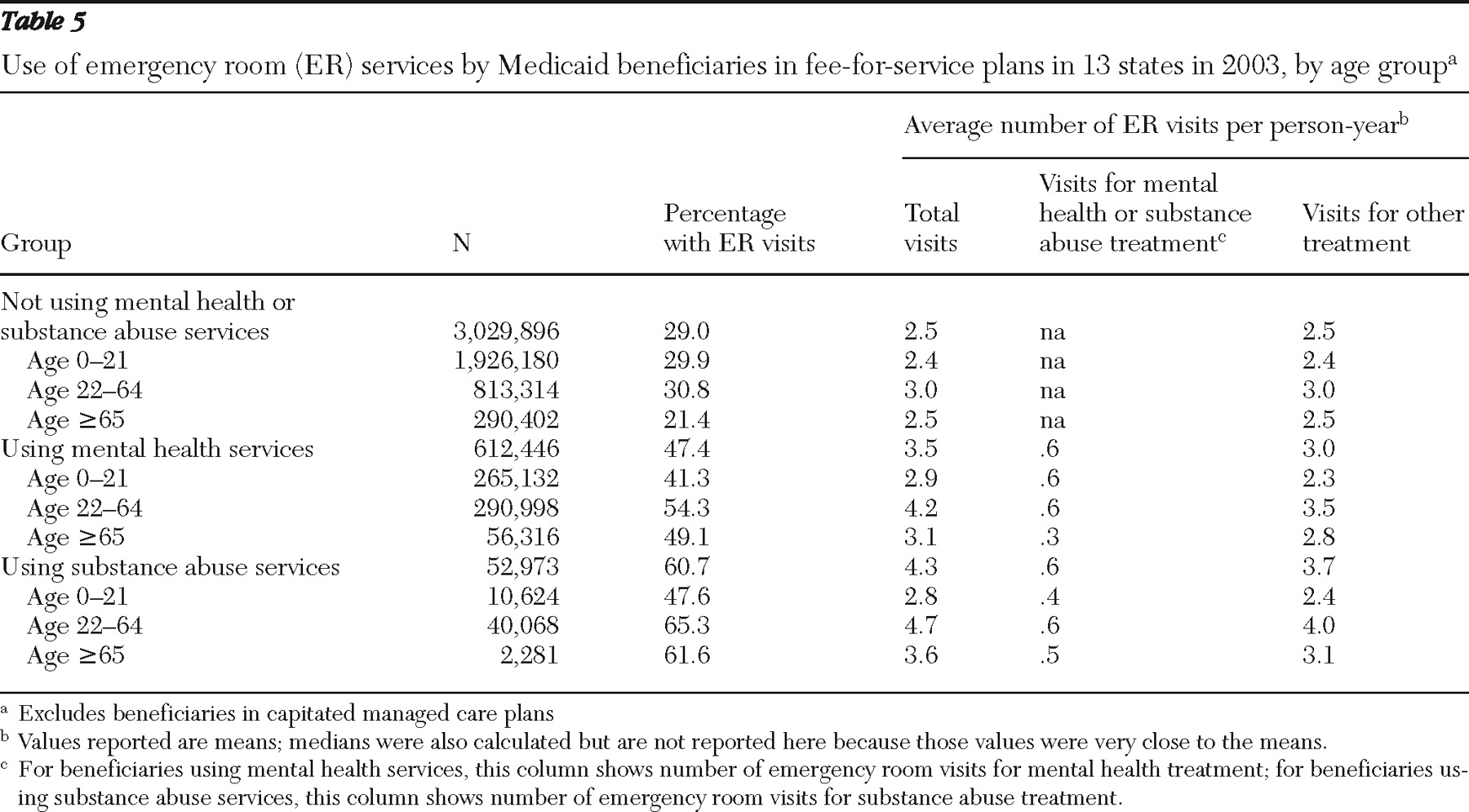
Emergency room use
Almost half (47.4%) of beneficiaries using mental health services and 60.7% of beneficiaries using substance abuse services visited an emergency room in 2003 (
Table 5 ). These beneficiaries made an average of 3.5 and 4.3 visits, respectively. Of the 3.5 visits made by beneficiaries using mental health services, three were for non-mental health treatments.
Within the group of beneficiaries who received substance abuse treatment and who visited the emergency room, most of these visits (3.7 of 4.3) were for treatment not directly related to their substance use disorders. In contrast, less than one-third (29.0%) of Medicaid beneficiaries who did not use mental health or substance abuse services visited an emergency room in 2003, with an average of 2.5 visits.
Discussion
Our findings on the age distribution of Medicaid beneficiaries who used mental health or substance abuse services have implications for the extent to which these services will be needed as Medicaid expands to cover new populations of low-income individuals. For example, the number of beneficiaries aged 45–64 is relatively low compared with other age groups, but this age group has the highest percentage of individuals who used mental health or substance abuse services (23.1%). Plans to expand Medicaid may increase the number of individuals in this age group substantially, with the potential for corresponding increases in the demand for mental health and substance abuse services.
Our findings also document the high use of psychotropic drugs among Medicaid beneficiaries. Within the group of beneficiaries who did not use mental health or substance abuse services, 17.3% of beneficiaries aged 22–64 filled a prescription for at least one psychotropic drug during 2003, and more than one-quarter (25.6%) of beneficiaries aged 65 and over did so. These findings may be driven by two factors. First, many individuals may have received prescription drugs as the sole treatment for their mental disorders, and because these claims do not include diagnostic codes, we did not identify these individuals as having mental disorders. Second, some beneficiaries use psychotropic drugs but do not report having mental disorders (
11 ).
In addition, almost half of the beneficiaries over age 21 who used mental health services received prescriptions for more than one class of psychotropic drug (45.9% for beneficiaries aged 22–64 and 47.4% for beneficiaries aged 65 and over). Depending in part on whether these drugs were prescribed simultaneously or sequentially, these figures may signal overuse (
12 ) and suggest the potential value of using administrative data to assess quality of care.
Another important study implication involves the extent to which beneficiaries who used mental health or substance abuse services also used general medical services. In the group of beneficiaries aged 22–64 who used mental health services, 8.9% used general hospitals for mental health treatment, with an average stay of ten days, and 18.9% used inpatient settings for non-mental health care, with an average stay of seven days. In addition, 47.4% of beneficiaries using mental health services and 60.7% of those using substance abuse services visited an emergency room in 2003, compared with 29.0% of other beneficiaries. These findings may indicate partly that beneficiaries with mental or substance use disorders rely on emergency room care because they lack a medical home that can attend to their mental health needs (
13 ). These findings also suggest the potential importance of strategies to improve the integration of mental health and general medical services for Medicaid beneficiaries.
Our findings should be interpreted in light of several caveats. First, the actual prevalence of mental or substance use disorders among Medicaid beneficiaries is likely to be higher than suggested by utilization figures because some beneficiaries likely never sought services during the observation period; for others (especially those with Medicare coverage as well), the mental or substance use disorder was not included on the Medicaid claim. Adelmann (
14 ) examined data from two national population surveys and found the 12-month prevalence rate for these disorders to be about 34% among Medicaid beneficiaries.
Second, our findings are based on information from the 13 states with the highest-quality data related to mental health services and managed care penetration rates below 33%. Although this approach minimized problems of missing data, it is not possible to generalize our results to Medicaid beneficiaries enrolled in managed care plans or to the population with fee-for-service plans in other states. However, many states do not enroll Medicaid beneficiaries with disabilities in managed care plans; to the extent that Medicaid beneficiaries with mental or substance use disorders in other states are eligible on the basis of disability (and therefore likely to be in fee-for-service systems), their patterns of service use may be similar to those reported in this study.
Third, the Medicaid program has changed since 2003. Most notably, the passage of Medicare Part D in 2006 shifted much of the cost of prescription drugs from Medicaid to Medicare for persons dually eligible to receive benefits from both programs (
15 ). This shift pertains directly to our findings on psychotropic medications for beneficiaries aged 65 and over.
Finally, our findings on the differences in use of medical services between beneficiaries who use mental health or substance abuse treatment services and other beneficiaries do not account for differences between these groups with respect to demographic or other characteristics or between states with respect to coverage policies. Investigators may wish to address this topic in future studies by using multivariate approaches that can account for the effects of multiple demographic and state factors on service use. In particular, the issue of variation between states, the possible reasons for such variation, and the effect of such variation on service use would be critical to address in another study.
Conclusions
In 2003, 11.7% of Medicaid beneficiaries (1.4 million individuals) in the 13 study states used mental health or substance abuse services. More than a quarter (28.6%) of Medicaid beneficiaries who were eligible on the basis of disability used these services in these states. These beneficiaries also received more general medical care than other beneficiaries. For example, 47.4% of beneficiaries using mental health services and 60.7% of those using substance abuse services visited an emergency room in 2003, compared with 29.0% of other beneficiaries. In part, study results may arise from differences in access to and use of other medical services, such as regular outpatient treatment, between beneficiaries who did and did not use mental health services and substance abuse treatment.
This study illustrates the value of using Medicaid administrative data to identify beneficiaries who use mental health or substance abuse services and to document their utilization patterns. Although MAX files can be delayed somewhat because of the time needed to prepare high-quality data suitable for research, they are a valuable source of information for tracking mental health service use in vulnerable populations. Recent improvements in data quality and timeliness suggest they will be especially useful for tracking the impact of upcoming policy and program changes.