Noncompletion of alcohol abuse treatment due to dropout or expulsion is the fate of about 20 to 50 percent of participants in inpatient treatment programs (
1.—
3.) and is associated with poor outcomes (
4). Although expulsion and dropout both threaten recovery, they are not the same. However, previous studies have not focused on this distinction and have often included expelled patients in the same category as those who drop out.
The different methods used to examine treatment noncompletion, including computerized registries (
3,
5), patient charts (
6), and psychological testing (
7,
8), have been cited as contributing to variations in results about specific variables associated with treatment noncompletion. Another contributing factor could be that these studies do not distinguish between subjects who drop out and who are expelled.
A common finding in most studies is the association of social marginality or deviance with noncompletion of substance abuse treatment. These studies have found that at least one of several such factors are associated with dropping out; they include less education (
3,
5,
9), antisocial or criminal behavior or psychopathy (
1,
5,
7), and unemployment (
5,
9). Perhaps not surprisingly, these findings are similar to correlates of dropout from other medical, mental health, and substance abuse treatment. Baekeland and Lundwall (
1) reviewed treatment dropout and noted that among the prominent associated factors are social isolation and unaffiliation, less social stability, aggressive and passive-aggressive behavior, and sociopathy.
From the perspective of social deviance and prognosis, differentiating between patients who drop out of treatment and those who are expelled is conceptually important. Persons who drop out are more likely to have recovered than those who are expelled.
This study tested the hypothesis that social marginality or deviance is a predictor of treatment noncompletion due to expulsion and not clearly related to dropout. The study was conducted in Israel, a family-oriented society where alcoholism and substance abuse are a relatively rare phenomenon (
10,
11) compared with the United States (
12,
13). Thus in Israel, alcoholics by definition are socially deviant, which afforded the opportunity to subject the social marginality hypothesis to a more extreme test.
Methods
Data from 1985 to 1994 were extracted from structured patient charts of 764 consecutive first-time admissions to a freestanding inpatient alcohol detoxification facility with 30 beds that provided a three-month treatment program. It is the only such facility in Israel. During this time, 105 additional admissions represented readmissions, and data for these admissions were excluded from the analysis. Among the 764 patients, 40 were women. No significant gender difference was found in treatment completion; however, due to the small number of women, they were excluded from the analyses. Information about termination status was missing for 37 patients, and in 11 cases termination occurred for other, nonspecified reasons. Thus the final sample consisted of 676 male patients.
For all patients, data included date and type of admission to the facility (first or repeat), sex, religion, age, birthplace, number of years in Israel, family status, number of children, education, employment, preferred drink, and status at termination. Status at termination included three categories: completed the program, was expelled, or dropped out. Since 1989, data on additional variables were available—level of religious observance, number of drinking years, and presence of a drinking partner.
Within the context of Israel and using the available data, social deviance in this study was defined as not being married, having no children, drinking alone, being unemployed, and not having completed elementary school.
Data analysis included three comparisons: completers versus quitters (dropouts who left treatment on their own), completers versus expelled patients (patients discharged for breaking rules or for substance abuse), and quitters versus expelled patients. Because the data are population data and represent all patients served for almost a decade in the only facility of its kind in Israel, differences are not attributable to sampling error. Significance testing was used as a criterion for selecting variables that had differences of potential interest between the groups. To show differences between groups, odds ratios are presented.
Results
Of the 676 patients, 436 (64.5 percent) completed the program, 57 (8.3 percent) were expelled for drinking, 31 (5.3 percent) for drug use, and 59 (10.1 percent) for breaking rules. Ninety-three patients (13.8 percent) left by choice. This distribution was about the same for all study years.
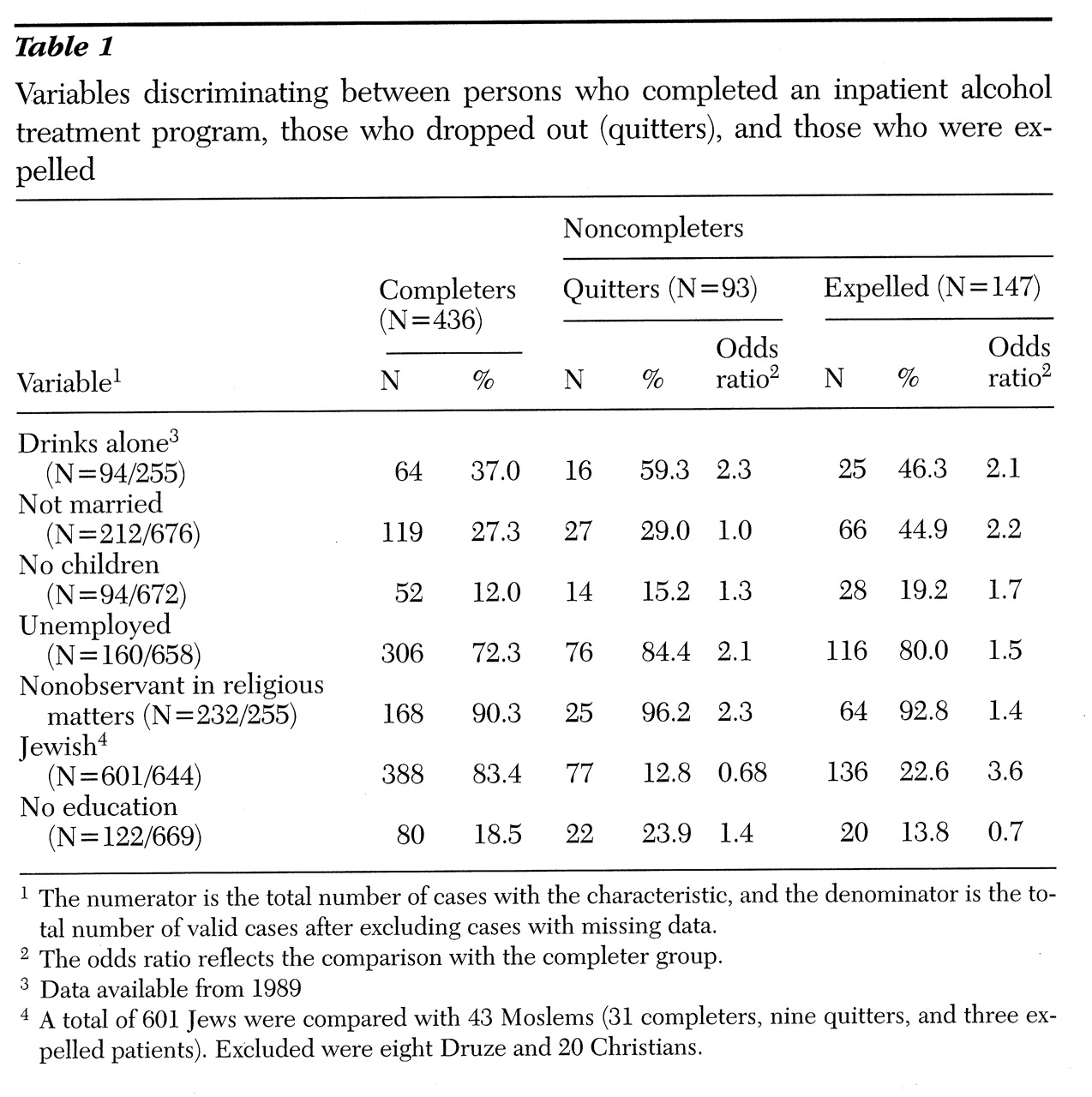
Table 1 presents the variables that significantly differentiated between at least two of the groups based on significance testing. (Specific test results are not reported here.) The variables are worded to reflect their hypothesized association with expulsion from treatment (for example, unmarried rather than married, unemployed rather than employed). The columns are ordered by the hypothesized strength of the association between the variables and each group—that is, the first column representing completers should reflect the weakest association. The rows are in order by the variables that revealed the greatest difference between the groups.
As
Table 1 shows, about a third of completers reported that they drank alone, whereas more than half of the quitters and almost half of the expelled patients did so. This difference is further illustrated by the odds ratios showing that patients who drank alone were a little more than twice as likely to be quitters or expelled from treatment than to have completed treatment. Although the percentages and odds ratios for the quitters and expelled patients supported the hypothesized difference between these groups and the completers on this variable, they did not indicate that the two groups were different from one another. On the other hand, the proportion of unmarried patients was similar for completers and quitters and twice as high among the expelled patients.
Unemployment differentiated between completers and noncompleters and was higher among the quitters. Fewer noncompleters were religiously observant and non-Jewish.
Surprisingly, the smallest proportion of patients who had not completed elementary school was in the expelled group. This finding might be partly due to the relationship between age and education. Completers were older than quitters and expelled patients (approximate median ages of 49.2, 48, and 46.8 years, respectively). A clear association was noted between having no education and age: 7.4 percent of patients in the 26- to 35-year age group and the 36- to 45-year group had no education, compared with 20.3 percent in the 46- to 55-year group, 32.3 percent in the 56- to 65-year group, and 34.2 percent in the group over age 65.
The age difference between completers, quitters, and expelled patients was mainly due to the oldest group of patients—38 patients who were over age 65—of whom 81.6 percent (31 patients) completed treatment, compared with 64.5 percent of the sample. The rest of the age groups were in the 60 percent range of treatment completion.
Examination of other variables did not reveal differences between groups. They included birthplace (North Africa, 29 percent of the sample; Israel, 27.3 percent; Asia [not India], 10.8 percent; and other places, 32.9 percent); number of years in Israel (born in Israel, 27.2 percent; ten years or more in Israel, 68.5 percent; and less than ten years in Israel, 3.7 percent); number of drinking years (less than five, 7.7 percent; five to ten, 18.2 percent; 11 to 15, 14.1 percent; 16 to 20, 29.6 percent; and 21 or more, 29.3 percent); and preferred drink (nonspecific whiskey, 61.7 percent; vodka, 18.5 percent; arak, 8.9 percent; brandy or cognac, 7.3; and beer or wine, 3.5 percent).
Completers and noncompleters were further studied using logistic regression, which included all variables in
Table 1 and which controlled for age. Two sets of analysis were conducted, one using variables for which data were available for all patients, and the second including data on the additional variables available since 1989. The model comparing completers and expelled patients found that not being married and drinking alone were the only variables significantly associated with being expelled.
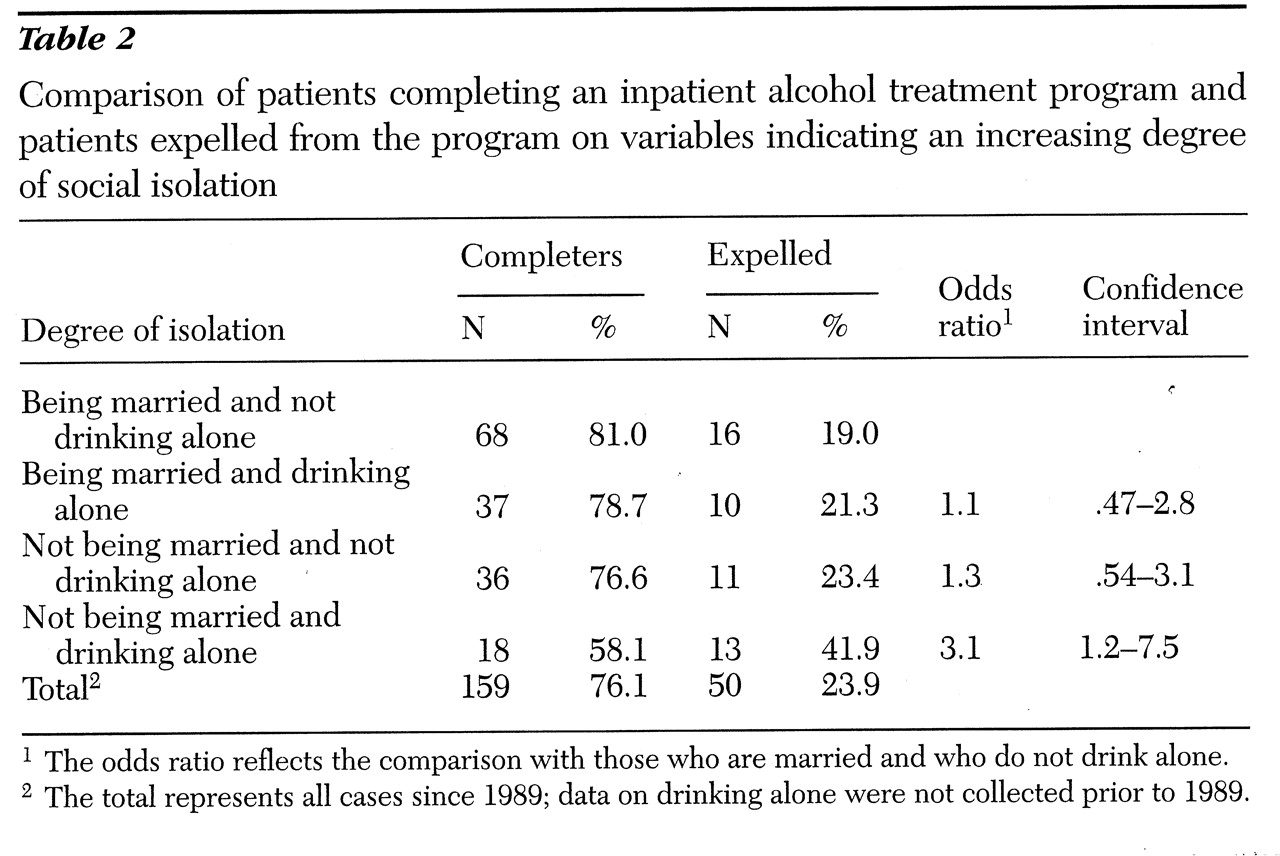
These variables were then combined into an index of social isolation, and another logistic regression model was estimated. As
Table 2 shows, 19 percent of patients at the least isolated end of the social isolation scale—those who were married and did not drink alone—were expelled. The expulsion rate increased almost monotonically along the scale of isolation, as also reflected by the odds ratio of being expelled versus completing treatment. The most dramatic difference was between the last two scale points, with almost half of the most isolated patients being expelled.
In further regression analyses comparing completers and quitters, drinking alone was the only significant predictor of quitting treatment. Similar analyses were conducted comparing quitters and expelled patients. Not being married emerged as the only significant variable.
Discussion and conclusions
The results suggest that social isolation is an important variable in predicting treatment noncompletion and that it has a dramatic effect on treatment expulsion. These findings support the important role of social isolation and marginality as risk factors for poor treatment outcomes among males. Future studies should attempt to include women, which was not possible in the current study because of the small number of female patients in the program.
The large proportion of expelled patients among the noncompleter group suggests that future studies should more carefully differentiate between noncompleters who are expelled and those who drop out.
The results suggest that in screening patients for treatment and in treatment planning, special attention should be given to the extent of their social isolation, which dramatically increased treatment noncompletion in the study reported here. In this study, indicators of isolation included not being married, drinking alone, and having no children. They may be associated with clinically observable variables like social avoidance and antisocial personality disorder, which may interact with such indicators.
Acknowledgments
The authors acknowledge the helpful comments of Evelyn Bromet, Ph.D., and the help of Gili Goren with data collection.