With the growth of managed care, the role of primary care physicians in the treatment of common psychiatric disorders is increasing. Their ability to provide appropriate care, however, needs to be assessed more thoroughly. This report uses data from the National Comorbidity Survey (NCS) (
1) to compare patterns of prescription medication use among individuals with mood and anxiety disorders who received care from psychiatrists and those who received care from primary care physicians (general practitioners or family physicians). The NCS surveyed psychiatric disorders in a representative household sample of U.S. residents age 15 through 54 between 1990 and 1992.
The study examined data on individuals with DSM-III-R diagnoses of major depression, dysthymia, generalized anxiety disorder, panic disorder with or without agoraphobia, simple phobia, social phobia, agoraphobia, and posttraumatic stress disorder who reported using prescribed antidepressants, anxiolytics (including benzodiazepines), hypnotics, or sedatives within the past 12 months.
Overall, 1,407, or 23.9 percent, of 5,877 NCS respondents met the criteria for at least one of the diagnoses. Of these, 6 percent saw psychiatrists and 7.2 percent saw primary care physicians for emotional or substance problems over the past 12 months. (Only .9 percent saw both.) Among those who saw a psychiatrist, 57.7 percent received medications in any of the three categories compared with 43.6 percent of those who saw a primary care physician.
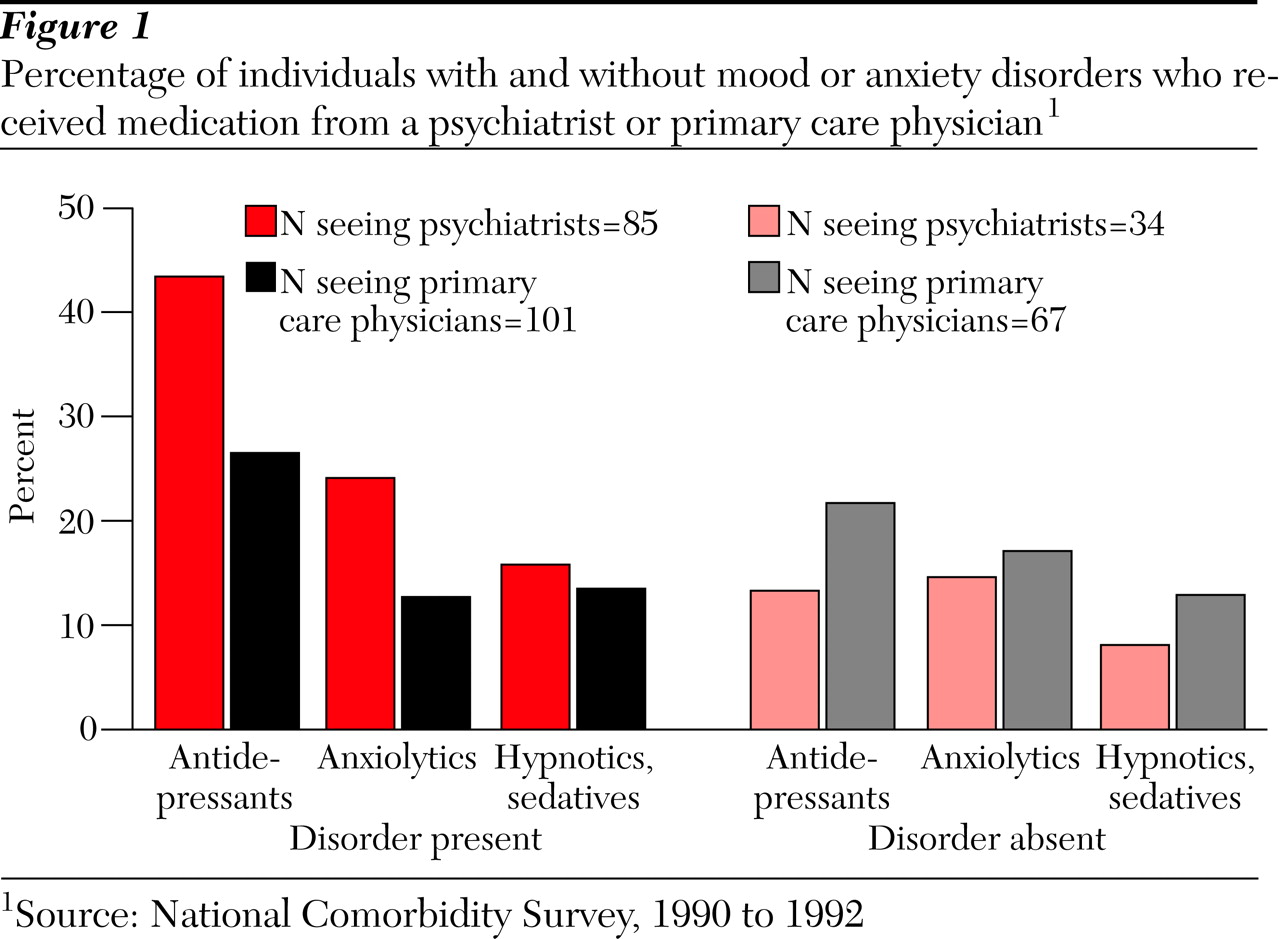
Figure 1 shows that individuals with a mood or anxiety disorder were more likely to receive antidepressants and anxiolytics from psychiatrists than from primary care physicians, while individuals without these disorders were less likely to receive psychoactive medications from psychiatrists than from primary care physicians. On the other hand, individuals with mood or anxiety disorders who saw psychiatrists were two to three times more likely to receive psychoactive medications than individuals without these disorders. No such pattern was observed for individuals who saw primary care physicians.
These data suggest that individuals with mood or anxiety disorders who receive care from primary care physicians are less likely to receive antidepressant or anxiolytic medications—drugs with proven efficacy in such conditions. Compared with psychiatrists, primary care physicians are less selective in their use of psychoactive medications, perhaps because of lower sensitivity and specificity of diagnoses in primary care settings. These findings are consistent with findings from studies conducted in primary care settings and raise doubts about the ability of primary care physicians to provide optimal care.
Acknowledgments
The National Comorbidity Survey is funded by grants R01MHDA46376 and R01- MH49098 from the National Institute of Mental Health, a supplemental grant R01MHDA46376 from the National Institute on Drug Abuse, and grant 90135190 from the W. T. Grant Foundation. Ronald Kessler, M.D., is the principal investigator.