Psychosocial rehabilitation is an important component of community support systems for persons with severe and persistent mental illness. Yet it is often buffeted by competing policy options for mental health service delivery.
This paper, based on a literature review, assesses the empirical status of psychosocial rehabilitation within community support systems. It begins by defining what is encompassed by the term psychosocial rehabilitation and then describes longitudinal outcome studies of persons with severe and persistent mental illness that demonstrate their long-term need for psychosocial rehabilitation services of varying levels of intensity. Findings of a "bare-bones" meta-analysis of recent outcome studies of psychosocial rehabilitation and of an integrative cost-outcome analysis are presented, along with a discussion of policy implications of the findings and recommendations for future research.
Methods
A literature review was conducted of experimental or quasi-experimental outcome studies of psychosocial rehabilitation interventions with subjects diagnosed with severe and persistent mental illnesses. The psychosocial rehabilitation domains reviewed were skills training, family psychoeducation, and supported employment. For policy issues, the literature review included empirical outcome investigations of heavy service utilizers, cost-effectiveness of alternatives to inpatient care, and service utilization over the course of illness. Due to the number of empirical domains reviewed, the search concentrated on earlier literature reviews and meta-analyses, supplemented by subsequently published studies in major psychiatric journals.
In addition to the literature review, a meta-analysis of findings from recent outcomes studies of psychosocial rehabilitation services was done using a bare-bones method (
1) that does not systematically correct for various experimental artifacts other than sampling error and is intended primarily to confirm or refute the main effect across studies.
Findings from several cost-effectiveness studies of psychosocial rehabilitation were used in an integrative cost-outcome analysis examining allocation of resources among various levels of service intensity.
Definition of psychosocial rehabilitation
Researchers have noted the lack of a clear definition for the term psychosocial rehabilitation (
2). In this article, the term refers to a range of social, educational, occupational, behavioral, and cognitive interventions for increasing the role performance of persons with serious and persistent mental illness and enhancing their recovery (
3,
4,
5,
6,
7). Psychosocial rehabilitation includes services aimed at long-term recovery and maximization of self-sufficiency, as distinguished from the symptom stabilization function of acute care (
8,
9).
The term psychosocial rehabilitation, as used here, does not refer to any particular theoretical model for accomplishing rehabilitative goals. In a review of definitions of psychosocial rehabilitation and research on their construct validity, Cnaan and associates (
2) identified 13 principles and eight factors that have been associated with psychosocial rehabilitation. The factors can be further grouped conceptually into three programmatic orientations—empowerment, competency, and recovery—that are typically manifested in four service domains.
The first domain—skills training—involves systematic skill building through curriculum-based psychoeducational and cognitive-behavioral interventions. Typically, these interventions break down complex objectives for role performance into simpler components, including basic cognitive skills such as attention, to facilitate learning and competency.
The second service domain is peer support, which includes consumer social clubs, drop-in centers, clubhouse crews, and self-help and advocacy networks. These programs typically occur in nonclinical settings with minimal, if any, professional facilitation. They usually focus on normalization and empowerment of persons with severe and persistent mental illness.
The third domain is vocational services, which include supported employment, transitional employment, supported education, consumer job clubs, specific job training, and prevocational skills training. A common approach in these programs is that consumers set their own vocational goals, which form the basis for motivation toward recovery of vocational roles.
The fourth domain—consumer-community resource development—includes direct services such as family education. It also includes indirect services in which professionals help consumers and families to create and operate support and advocacy networks and to initiate such projects as speakers' bureaus, drop-in centers, and consumer-run businesses. This domain is considered particularly important from a public health perspective, because it creates an infrastructure of community supports that can help manage clinical risk and reduce reliance on direct treatment services, especially more restrictive levels of care (
10,
11).
Psychosocial rehabilitation can be viewed as a specific program within a array of community mental health services or as a paradigm that transforms all mental health services (
12). The following three-part provisional definition was used to guide this review.
• Psychosocial rehabilitation is an organized set of psychosocial interventions that includes one or more of the areas of skills training, peer support, vocational rehabilitation, and consumer-community resource development.
• It is targeted to individuals who have major psychotic disorders and functional impairments equivalent to the federal definition of severe and persistent mental illness (
13).
• It is oriented toward empowerment, recovery, and competency.
This definition does not address some of the qualitative principles of psychosocial rehabilitation identified by Cnaan and associates (
2). In addition, not all skills training can be considered psychosocial rehabilitation—only training that uses systematic, curriculum-based interventions. Because an intervention's orientation toward empowerment, recovery, and competency is often not specified in outcomes studies or literature reviews, these important dimensions of psychosocial rehabilitation could not be operationalized for purposes of this review.
Life course of psychotic disorders
Some of the most dramatic support for psychosocial rehabilitation and long-term recovery comes from the longitudinal outcome studies conducted by Harding and associates (
14,
15,
16). The results of their studies and of other studies from around the world that they reviewed showed that the long-term outcomes of schizophrenia are widely heterogeneous. The results also suggested that patients may have a higher potential for recovery than previously thought, even when recovery rates are controlled for hypothetically higher mortality rates among the most seriously impaired patients.
Harding and colleagues conducted a 32-year follow-up study that examined outcomes for 118 patients from the back wards of Vermont State Hospital who had been described in hospital records as treatment resistant, chronically disabled, and multiply hospitalized. The patients retrospectively met DSM-III criteria for schizophrenia. At follow-up, the patients were living in a variety of community settings. Forty-five percent of the patients were symptom free, and 61 percent received a Global Assessment Scale score of 61 or higher, indicating fair functioning or better.
A matched comparison with a sample of patients in Maine showed that the Vermont patients had significantly better outcomes in global functioning, community adjustment, amount of time in the hospital, use of community resources, employment, and symptom levels (
16). The only salient difference between the two samples was the Vermont sample's early exposure to psychosocial rehabilitation. These findings draw attention to the developmental aspects of psychiatric disability and recovery and the cumulative effects of rehabilitative interventions within a population over time. They also highlight the risks of the "clinician's illusion," that is, the error of generalizing from a sample in treatment at a particular point in time to the entire population of persons with severe and persistent mental illness (
17).
Variation in the severity of illness and disability over the course of the individual patient's life is likely to be reflected in fluctuating need for services. This conclusion is supported by studies of heavy service utilization, which have found that 10 to 35 percent of clinical psychiatric populations are heavy users of services and consume 50 to 80 percent of total resources (
18,
19,
20). However, membership in the category of heavy users changes over time; it is not a consistent characteristic of individual patients in a majority of cases and is influenced by social and system factors as well as by the needs of individual patients (
18). The proportion of resources consumed by heavy service users and the system factors that influence which patients become heavy service users have policy implications that will be discussed later.
Service responses
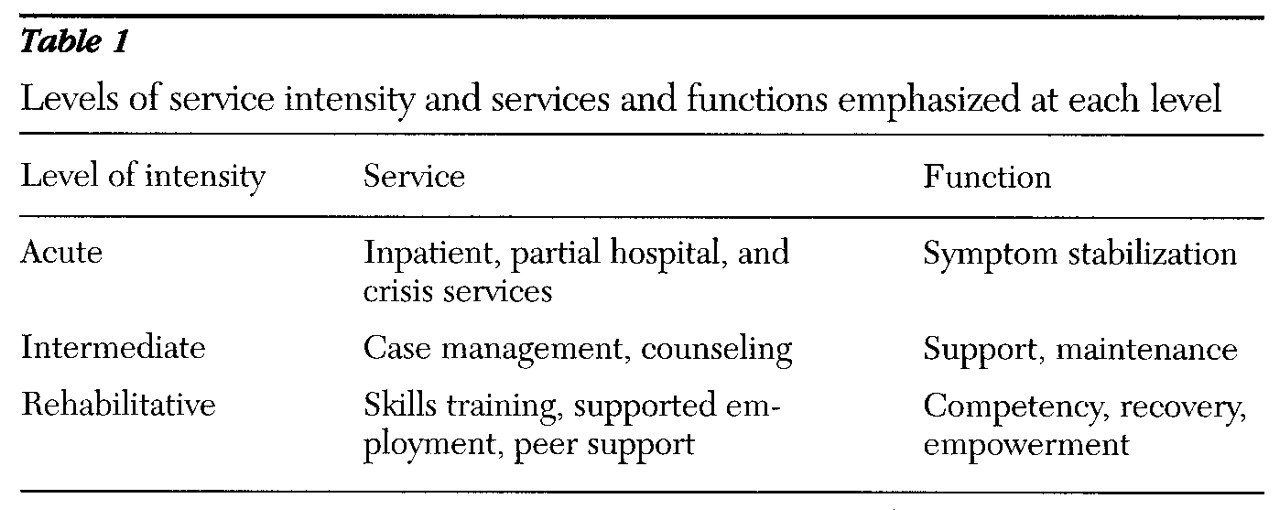
Levels of service intensity
Service intensity can be understood as a combination of the frequency of contact between the consumer and service provider and the restrictiveness of the service setting. Community support services, and mental health services in general, can be divided into three levels of service intensity—acute, intermediate, and rehabilitative. Although some types of interventions, such as medication, crisis intervention, and counseling, may occur across the three levels, the emphases of each level can be differentiated, as shown in
Table 1.
Policy decisions about levels of service intensity are generally based on several assumptions. The first is that poorly managed acute care services can easily absorb all of the available resources. Second, to utilize resources more effectively and efficiently, a variety of alternative community services must be available. Third, even if intensive case management is targeted to individuals with the most intense service needs, these individuals are at risk of relapse if they do not have adequate community supports and coping skills (
21,
22). Finally, without investment in rehabilitative care, the service system will tend to stagnate at a less than optimal level. A fully developed service system balances resources among the three levels of service intensity, allowing more persons to be served at a lower average cost per client.
Although the systemic relationships between the three levels of care are intuitively obvious, they may nonetheless play a limited role in services planning and allocation decisions, which are structured by annual budget cycles that tend to neglect long-term, developmental considerations. Efforts to reduce utilization of acute levels of care can rely on either supply-side or demand-side strategies. The former focus on restricting access; the latter focus on reducing need through managing risk factors and enhancing resilience. Although most systems will first exhaust the economic possibilities of supply-side strategies before pressures to consider the demand-side become salient, the demonstrated benefits of demand-side strategies, which are reviewed in the following sections, should not be ignored.
Outcomes of rehabilitative services
Skills training, supported employment, and family education.
Research-based behaviorally oriented skills training with seriously dysfunctional inpatients began in the 1970s with the groundbreaking work of Paul and Lentz (
23). Their rigorous demonstration of the effectiveness of this intervention stimulated continued research and further development of this approach. Recent meta-analyses and reviews have found that behavioral skills training is effective for training persons with psychiatric disabilities in a variety of social and functional skills, but that this approach requires continued attention to issues of transfer, generalization, and maintenance (
24,
25,
26).
The most recent and most comprehensive meta-analysis, comprising 68 studies, judged their methodology to be good overall. It found that the 59 between-group studies generated a medium effect size (between .33 and .55) at posttest (p≤.001) and a large effect size (over .55) at follow-up (p≤.01) (
24). Although the authors were critical of skills training for failing to produce significant employment outcomes, employment is only one of many client outcome domains.
Psychosocial rehabilitation in general and skills training in particular, for both consumers and family members, are intended to promote a range of outcomes (
27). These interventions have demonstrated success in symptom reduction, community adjustment, relapse prevention, medication compliance, and reduced use of the hospital and other restrictive settings (
28,
29,
30,
31,
32,
33,
34,
35,
36).
Cognitive skill remediation has shown promising results in helping patients relearn basic information processing abilities such as attention, concentration, and memory (
37,
38,
39), which are critical to the acquisition of other skills and, in some approaches, are taught together with other skills in an integrated program (
40). Cognitive skill remediation has also shown success in directly reducing psychotic symptoms (
38). Controlled studies of cognitive therapy have shown significant effects in reducing positive and negative symptoms and reductions of 25 to 50 percent in recovery time (
41,
42). Hogarty and colleagues (
43,
44) conducted controlled trials of personal therapy for schizophrenia and found that the structured, disorder-specific, carefully titrated intervention was effective in restoring patients' interpersonal and intrapsychic functioning. Although this intervention is intended for individual patients—unlike the previously reviewed group approaches—it is nonetheless a psychosocial intervention for improving functional skills.
Reviews of supported employment have found consistently positive employment outcomes but have found no evidence that employment gains are generalized to other outcomes (
45,
46). McFarlane and associates (
47) showed that patients who participated in an intensive case management program that had a vocational and rehabilitation orientation and provided family psychoeducation had significant improvement in community adaptation compared with patients who received intensive case management alone.
Reviews and meta-analyses of family psychoeducation studies show consistently strong outcomes for the mentally ill relative (
48,
49), including reduced relapse (
49,
50,
51), reduced psychotic symptoms (
48,
51), and increased self-efficacy for the family member (
52). One investigator concluded that "consistent evidence for the efficacy and feasibility of family intervention in schizophrenia has now demonstrated an effect, in medicated patients, equivalent to antipsychotic medication itself" (
51).
The relative contributions of medication and psychosocial interventions to patients' improvement is complex and deserving of investigation. It is possible that some interventions may derive a significant portion of their effectiveness from subjects' becoming more engaged in their medical treatment and, as a consequence, more regular in taking medication or more likely to receive a better titration of medication. Without experimental manipulation of these variables and random assignment of subjects, the causal contribution cannot be determined.
A meta-analysis of research on family psychoeducation published in 1994 (
49) and the meta-analyses of studies of social skills training published between 1990 and 1996 (
24,
25,
26,
53) encompassed more than 80 studies and 4,000 subjects and showed substantial positive effects. However, a brief summary of research published after these analyses is warranted. I conducted a bare-bones meta-analysis of all studies of social skills training published between January 1995 and June 1998 in five major journals that represented a range of methodological orientations toward measurement of efficacy and effectiveness. A bare-bones meta-analysis does not systematically correct for various experimental artifacts other than sampling error (
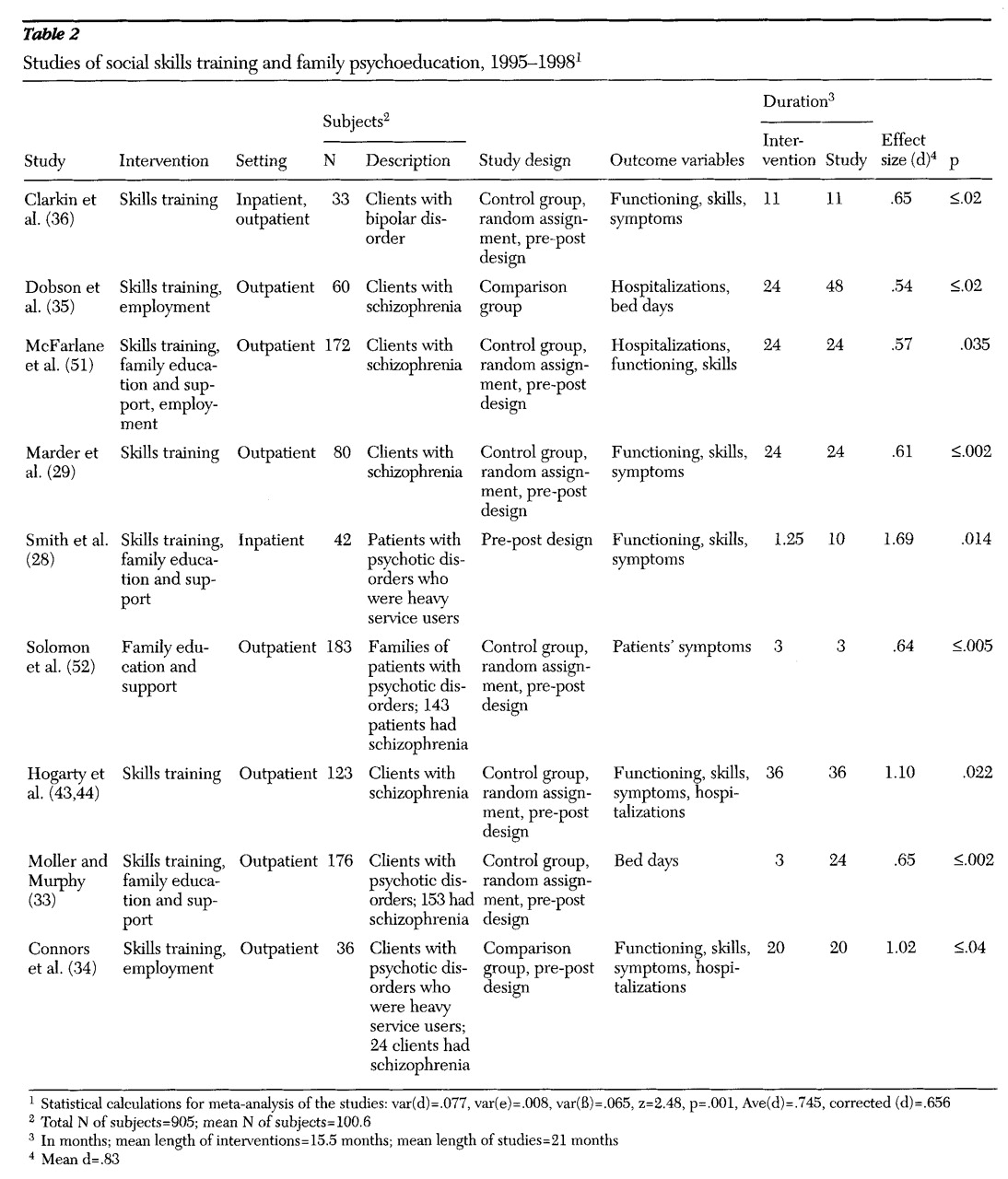
1). The purpose of the analysis was to confirm or refute the main effect across studies, not to examine moderator variables.
The analysis included studies of skills training for clients, including inpatient and outpatient interventions and family interventions. Studies using nonparametric statistics were omitted. The nine studies selected for the meta-analysis (
28,
29,
33,
34,
35,
36,
43,
44,
51,
52) are summarized in
Table 2. Of the total of 998 subjects, 878, or 88 percent, had a diagnosis of schizophrenia or schizoaffective disorder. Two-thirds of the studies used random assignment with pre-post measures.
Although the selection procedure obviously eliminated unpublished studies, the risk of source bias toward positive and significant results was thought to be minimal, even though a general tendency to somewhat lowered values in dissertation studies has been noted (
1). However, restricting selection of studies to five journals could have been a source of bias. To address this possibility, Hunter and Schmidt's corrections (
1) for bias and standard error were used. Because the chi square test for homogeneity of variance is thought to be trustworthy only for very large samples (
1), heterogeneity was assumed and the sampling error variance was computed, resulting in a 95 percent confidence interval of .563 to .927 for the average population effect size. Average effect sizes equal to or greater than .55 are considered large. Because the entire confidence interval is greater than .55, there is a 95 percent probability that the actual effect is large, thus confirming previous reviews and meta-analyses.
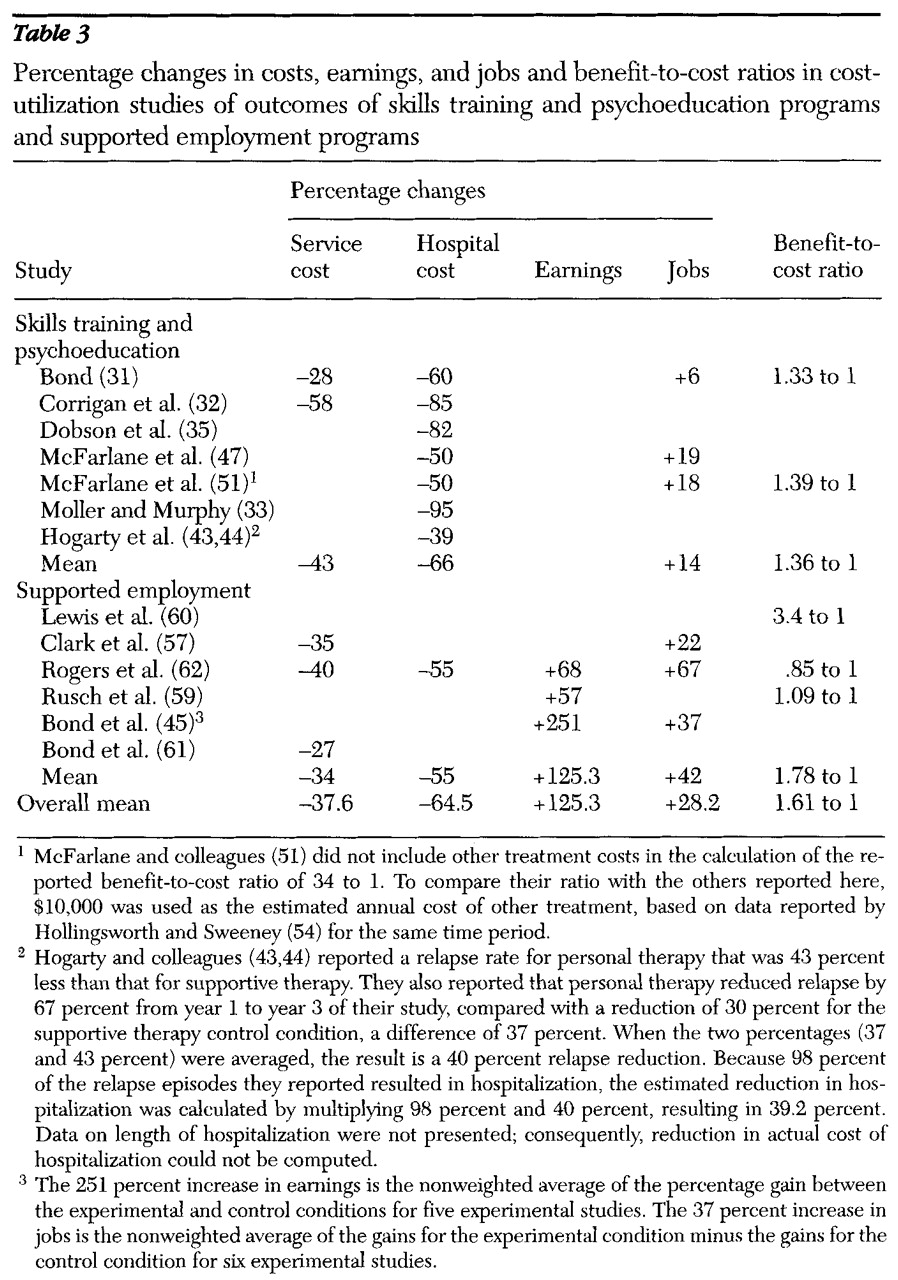
Costs and benefits of skills training and supported employment.
Few studies have examined overall expenditures for services for people with severe mental illness (
54). Cost-effectiveness research on skills training is also limited, although the studies that have been done have shown cost-effective outcomes due mainly to reduced use of hospitalization (
31,
32,
33,
34). Studies of supported employment have also found positive outcomes, despite inconsistencies in how different investigators calculate costs and benefits (
55,
56). In the 14 cost-effectiveness studies on skills training and supported employment reviewed here (
31,
32,
33,
34,
35,
43,
44,
45,
47,
51,
57,
59,
60,
61,
62), the average benefit-to-cost ratio was 1.61 to 1, which means that for every dollar invested in program costs, $1.61 in benefits were generated. The average improvement in all of the cost-related outcomes for the 14 studies was 63 percent. (
Table 3 shows these results.)
Some findings in studies of supported employment have prompted investigators to call for direct job placement, bypassing skills training and dropping day treatment altogether (
57,
58). However, other findings have shown that 40 to 78 percent of clients end a supported employment placement within six months, that the effects of supported employment do not appear to generalize to other outcomes, and that an approach that integrates mental health services with vocational services and outreach tends to produce better results. Also, studies of supported employment have not analyzed the contribution of subjects' previous experience with skills training to outcomes and dropout rates (
56,
63).
Based on study findings and field experience (
64), supported employment appears to be an effective and efficacious component of psychosocial rehabilitation. However, a comprehensive psychosocial rehabilitation model is necessary to address the range of individual differences in consumers' functional needs and goals. Replacing all skills training—which showed an average effect size of more than .56 in the meta-analysis reported here—with supported employment, for which dropout rates of 40 percent or more have been reported, seems precipitous at best. Relapse prevention and community adjustment skills are equally as important as job placement, especially for clients who drop out of supported employment programs.
In summary, longitudinal and outcomes research strongly supports the effectiveness and efficacy of psychosocial rehabilitation, but continued research is needed to further refine intervention strategies. Various practice guidelines and recommendations reflect current research in supporting a comprehensive and integrated approach to psychiatric rehabilitation (
65,
66,
67,
68). The accumulation of empirical support calls for a policy analysis that situates psychosocial rehabilitation in relation to system design and allocation of resources among levels of service intensity.
Policy implications
The community support systems model includes several components, some operating like prostheses to compensate for patients' psychiatric disabilities and others operating to retrain and rehabilitate patients' neurocognitive and neurobehavioral capacities (
69,
70). In general, these systems are intended to be comprehensive, in that all components of the model, including psychosocial rehabilitation and support services, should be present (
69,
70,
71). The systems are also intended to be balanced, in that available resources are allocated among the various components in a way that does not privilege particular components.
Outcome studies of acute and intermediate levels of service intensity have shown that a policy of balancing resources among system components is consistent with both consumer needs and cost-effectiveness. These data have suggested that length of inpatient stay is unrelated to clinical outcome (
72), that partial hospitalization and ultra-short hospitalization can generate clinical outcomes equivalent to traditional inpatient hospitalization (
73,
74,
75,
76,
77), and that cost savings can be realized from alternatives to traditional hospitalization (
73,
78,
79,
80,
81) that may enhance clinical outcomes (
82). The policy of carefully limiting inpatient utilization to the minimum necessary while promoting access to outpatient services has also been empirically supported (
83,
84,
85,
86). Because delays in treatment have been shown to increase the length of psychotic episodes, both rapid response treatment and relapse prevention should be priorities (
87).
In many regions, resources have been allocated in a way that creates a crisis-oriented mental health system. The third of the target population estimated to be heavy users of services consumes roughly two-thirds of the available resources, with the result that a majority of resources are devoted to expensive acute care for a minority of those in need. Most of the remaining third of available resources is allocated to intensive case management and other intensive services for those at risk of hospitalization. In such a system, rehabilitative services may not even be offered as a service option. However, ignoring these services in policy making at the national and state levels will result in missed opportunities for moving the mental health system toward more humane and cost-effective long-term solutions.
Effectively balancing appropriations within a service system implies taking into account not just the service system design and the characteristics of the target population, but their evolution over time. Longitudinal studies of serious mental illnesses have indicated that the functional deterioration and deficit symptoms underlying chronicity may originate in the early years of the disorder (
88) and that reduction in clinical needs over the life cycle is possible if patients receive rehabilitative and support services early in the illness (
14,
15,
16).
Although additional research is certainly needed, these findings suggest an age-specific vulnerability to external stresses that can be modified by appropriately timed rehabilitative interventions. Because the external circumstances and stressors that influence relapse and heavy service utilization ebb and flow in unpredictable ways, the service system must continue to evolve to compensate for such random or insufficiently understood fluctuations. As findings about the relationship between resource shifts and functional improvement of the target population accumulate, the service system can more effectively anticipate and respond to the factors that generate relapse.
Consideration of balanced appropriation in a community support system implies a vision of deinstitutionalization, like recovery itself (
9,
89), as a dynamic process, with an evolving knowledge base that continues to revise and extend the vision. Now that long-term institutional care is no longer the central focus of the service delivery system, policy makers can shift their attention to the consequences of deinstitutionalization within the community. For example, the nursing home reforms that were initiated by the Omnibus Budget Reconciliation Act of 1987 (OBRA) were a response to the fact that many persons with psychiatric disabilities who had formerly resided in state psychiatric hospitals had been transinstitutionalized to nursing homes and other long-term-care facilities. Despite the beneficial consequences of OBRA, many still reside in those settings (
90,
91).
Now that rehabilitative techniques have been developed and proven effective, the vision of deinstitutionalization can be broadened to include a move away from acute services and structured residential settings toward independent living, employment, and improved quality of life. This phase of deinstitutionalization requires a shift in future resource allocation toward rehabilitation. However, if savings due to improved utilization management are diverted to other uses, such as corporate profits or government cost shifts, rather than following the client, the potential systemic gains will be undermined.
Recommendations for research
Although the literature on the effectiveness of psychosocial rehabilitation is convincing, a limitation is that the published studies have examined intervention strategies individually rather than in combination. Consequently, we do not know which combinations and amounts of interventions produce optimal effects for which subjects, nor do we know what the additive population effects might be. For example, individual differences in capacity and responsiveness to currently available treatments have been shown to vary considerably (
92,
93), and individual differences in prior treatment and current medication usually have not been analyzed. In addition, studies of supported employment interventions have shown high dropout rates of 41 to 77 percent within six months, but they have not identified client characteristics that predict success or failure other than prior work history.
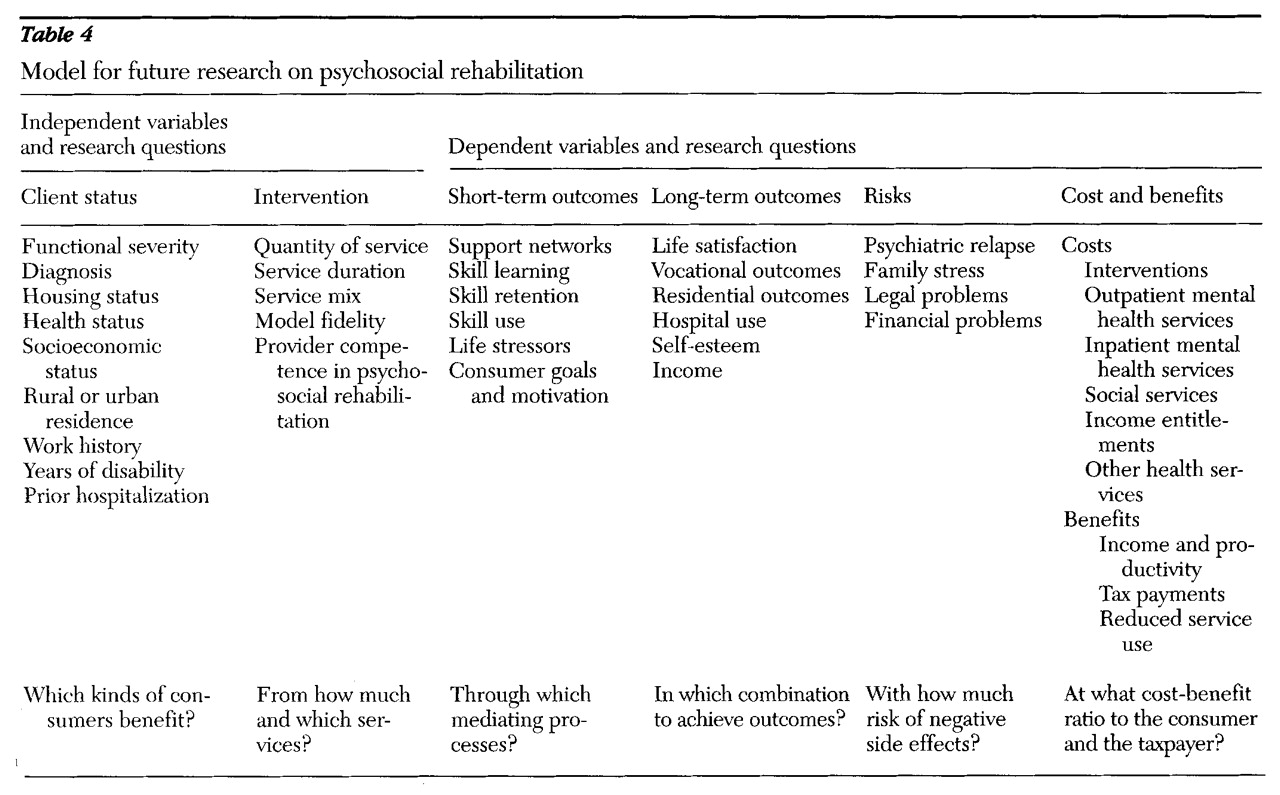
A model to guide future research on psychosocial rehabilitation interventions is presented in
Table 4. Future research should address several issues:
• The outcomes and costs of psychosocial rehabilitation components as they interact in combination with client characteristics and situational variables should be examined.
• Literature reviews and additional outcome studies on empowerment and ecological analyses of community resource development are needed. Although these types of psychosocial rehabilitation activities have received some attention from researchers and have been described in some first-person accounts by consumers (
94,
95,
96,
97,
98), additional attention to practical strategies and empirical outcomes would be useful.
• Traditional day treatment services that do not have psychosocial rehabilitation and recovery as a primary focus should be more fully described and analyzed as a baseline for comparison with rehabilitative interventions.
• Methods for defining, measuring, and implementing fidelity to psychosocial rehabilitation principles should be developed.
• Staff competencies and training approaches that are empirically successful in replicating psychosocial rehabilitation models should be identified.
• Existing longitudinal data on the service utilization patterns of persons with severe mental illnesses and the effects of rehabilitative interventions should be analyzed.
• Allocation of resources among levels of service intensity and the effects on outcomes and heavy service utilization should be compared across states.
• Theoretical research is needed to integrate service system dynamics with the population dynamics of remission, relapse, and resilience and the developmental aspects of recovery.
Conclusions
The long-term developmental course of serious psychiatric illness, the consequent functional deterioration in those afflicted, and various service system characteristics contribute to relapse in complex ways. Research findings have indicated that without continued improvement in skill acquisition and social supports or ongoing case management, many consumers will be at risk of relapse and some will be at risk of becoming heavy users of service systems.
As a set of responses to this clinical need, the essential direct service elements of psychosocial rehabilitation—skills training, family education, and vocational services—are supported by substantial empirical evidence of improved clinical and economic outcomes. Longitudinal studies have indicated that recovery is a realistic vision and that symptom remission and normal role functioning can be achieved by about 60 percent of those with psychiatric disabilities.
The accumulated evidence of clinical need and of effective and efficacious outcomes of psychosocial rehabilitation suggests revised population parameters for policies affecting utilization and allocation of resources. Specifically, investment in psychosocial rehabilitation can reduce expenditures for intensive, high-cost services while extending the reach of deinstitutionalization. A preponderance of the evidence is sufficient to support such a policy, since the decision is between one allocation balance and another.
A second phase of deinstitutionalization involving substantial resource shifts from acute to rehabilitative levels of care is now possible. Such shifts can enhance the comprehensiveness and effectiveness of community support systems in ways that address the unique developmental course of serious psychiatric disorders while generating better outcomes for consumers and taxpayers.