Researchers and health professionals have long observed that psychiatric patients have reduced life expectancy (
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18). Controlled studies of patient populations have quantified this risk in the United States and abroad, and the reported standardized mortality ratio—the ratio of deaths in the patient population to the number that would be expected in the general population—has ranged from 1.7 to 5 (
3,
4,
5,
6,
7,
8,
9,
10,
11,
12). Studies of general populations have also confirmed the increased risk of death associated with serious mental illnesses, especially schizophrenia, major affective disorder, and substance use disorders (
13,
14,
15,
16,
17).
Recently Felker and associates (
18) reviewed mortality and morbidity findings and recommended development of models of primary care specific to psychiatric patients. However, samples in studies to date have typically been too small to guide such development in any detail. The last large-scale published study of mortality in the United States analyzed 331 deaths among 5,412 patients admitted to a single facility between 1972 and 1981 (
6). None have examined data on multiple causes of death, which have been available in all states only since 1989.
The study reported here used a cross-sectional survey of an administrative patient registry linked electronically to vital records to provide data on deaths over the six-year period from January 1989 through December 1994. The study objectives were to update findings on the mortality of persons with serious mental illness and to provide greater detail on causes of excess mortality. The findings were intended to focus on specific health risks likely to be encountered by primary care and mental health professionals treating the most disabled populations.
Methods
Study design and data sources
The Massachusetts administrative patient registry was linked electronically to vital records for 43,274 persons age 18 and older who used inpatient, residential, or case management services of the State Department of Mental Health (DMH) between July 1985 and October 1994. To be eligible for these intensive services, a person needed to have a diagnosis of at least one "serious or long-term mental illness" other than mental retardation or substance abuse, although these disorders may also have been present. In addition, there must have been evidence of serious dysfunction, such as a risk of danger to self or to others or the inability to care for oneself as a result of the mental disorder (
19,
20,
21).
Data for inpatients were entered into the patient registry starting in July 1985, and data for patients receiving residential and case management services were added beginning in 1988. Cases were included in the study whether or not the individuals continued to receive services from the department of mental health over the study period. In about 45 percent of cases the primary diagnosis was schizophrenia or schizoaffective disorder, and 37 percent of the sample had a major affective disorder. This breakdown of diagnoses was based on internal agency reports. However, because treatment diagnoses were not uniformly available at the time of this study, we did not analyze mortality by psychiatric disorder.
Death certification and vital records linkage
Each state maintains electronic records of all deaths occurring within the state. The records originate with the U.S. Standard Certificate of Death and include data on place of death, whether an autopsy was performed, and the presence of up to 20 medical conditions originally noted by a certifying physician. Medical conditions are reviewed by state nosologists and coded in standard
ICD-9-CM nomenclature, after which records are subjected to electronic editing to remove duplicate or invalid codes and to assign a single underlying cause of death (
22,
23). The underlying cause is the condition judged, in the context of all valid contributing causes, to have initiated morbid events leading ultimately to death.
The DMH registry was electronically matched with state death files for the six-year period from January 1989 through December 1994. Access to patient records by the first author was authorized by the department's institutional review board for the protection of human subjects for matching purposes only. Matching was based on iterative comparisons of names, sex, birth dates, and Social Security numbers, followed by manual inspection of complete records to eliminate false positives. All personal identifying data were removed from the resulting analytic files.
Coding of cause of death
One data file based on underlying cause of death was created, with one record per decedent (N=322,806). A second file containing one record for every mentioned condition was also created. This file therefore contained more than one record per decedent when multiple causes of death were reported (N=819,588). Codes for cause of death were grouped using the Clinical Classification for Health Policy Research (
24), a system that combines all
ICD-9-CM codes into 18 broad classes and 260 clinically related conditions. The classification was expanded to include
ICD-9-CM E codes, which are used when the underlying cause of death is injury. E codes specify the manner in which an injury occurred—accident, suicide, homicide, and undetermined—while the nature of the injury, such as poisoning, is captured by codes already included in the classification.
Life expectancy
To provide a measure of relative excess mortality, we estimated years of potential life lost relative to current life expectancy for each decedent. Unlike life expectancy at birth, which does not change, current life expectancy is the mean survival age for a living cohort of each age and sex. Years of potential life lost is thus always a positive value and approaches zero at advanced age. This method has been used routinely by the Centers for Disease Control and Prevention (CDC) since 1982 to report the relative burden of disease and injury (
25). Various methods of measuring years of potential life lost have been adopted as alternatives to standardized mortality rates to assess the impact of specific causes of death (
26,
27). For this study the number of years of potential life lost was derived for each decedent based on current life expectancy in the U.S. in 1992 (
28).
Age adjustment
The state's non-DMH population was used as the standard for comparison of expected frequencies and years of potential life lost. Because the living DMH and non-DMH populations have different age and sex distributions, valid comparisons could not be made without adjusting for this difference. Data for the DMH population were standardized following the direct standardization procedure recommended by CDC (
29). Age and sex distributions for the total Massachusetts population from the 1990 census were used to approximate the non-DMH population in the following formula. Analysis weights were computed for each decedent served by the department of mental health asW=P
GP/P
DMHwhere W is the final analysis weight for each DMH case by age and sex, PGP is the proportion of the total state population for each age and sex, and PDMH is the proportion of the total DMH population for each age and sex. For example, young adults and males—groups that are overrepresented in the DMH population—received weights of less than one, while females and the aged received weights greater than one. The weights were applied to the data for each decedent in the DMH population and used in all analyses reported in the results section.
Statistical analysis
SAS software was used to calculate expected frequency distributions and derive associated chi square values and significance levels by cause of death (
30). SUDAAN software was used to compute weighted differentials for mean years of potential life lost and associated t test values and significance levels for each cause-of-death group (
31).
Results
Patient characteristics
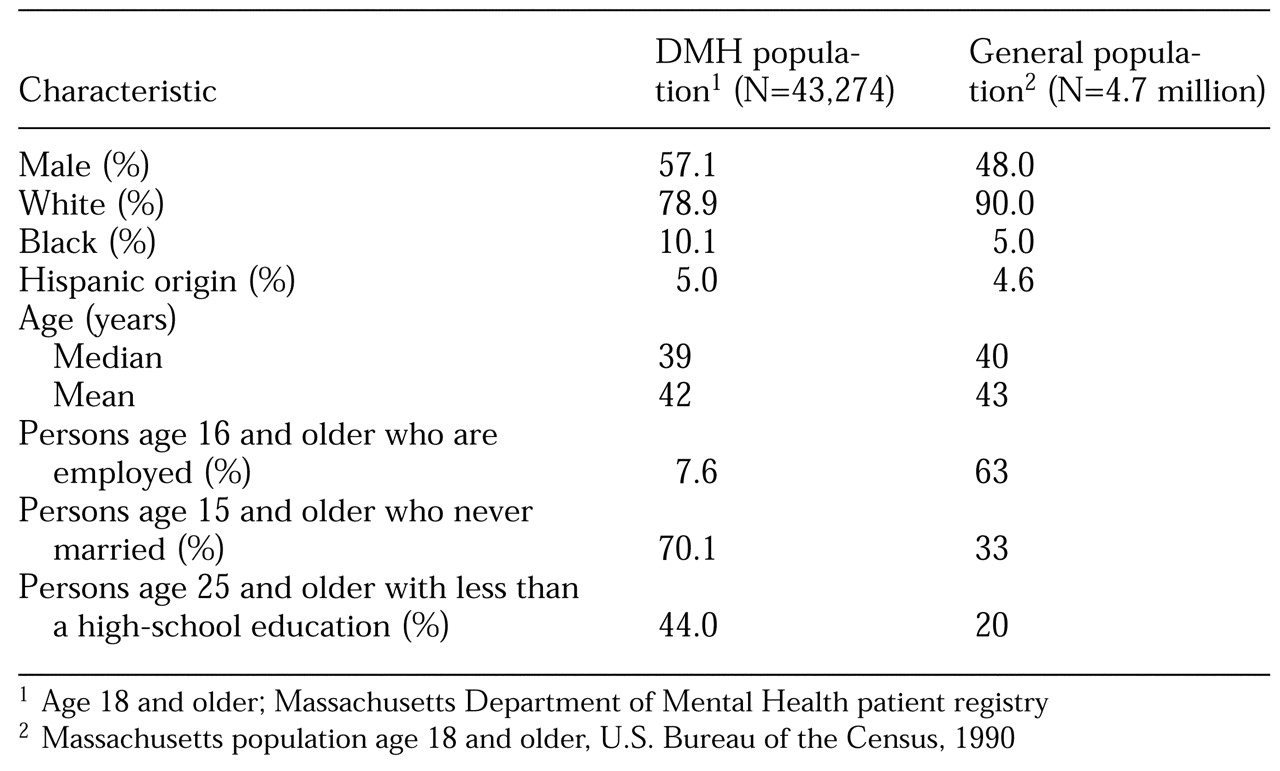
Table 1 shows characteristics of the living population of persons served by the DMH and the living general population before the data were adjusted for age and sex. Adjustment corrected for the dominance of males in the DMH population and for any underlying differences in the age distributions; however, differences in employment, marital status, and education remained.
A total of 1,890 persons served by the DMH and 320,916 persons in the non-DMH general population age 18 and older were identified in death records for the six-year period from 1989 through 1994. After the data were adjusted, the weighted total for the DMH population was 2,214. The median age at death was 66 years for the DMH population and 76 for the non-DMH population. DMH decedents were slightly less likely to die in a hospital than decedents in the non-DMH population—49 percent versus 51 percent, not a significant difference—but were much more likely to have an autopsy (26 percent compared with 10 percent, 2=742, df=1, p<.001).
The average number of conditions that were reported to contribute to death was approximately the same for each group at 2.5 per death. Mental disorders were reported as a contributing cause for 19.1 percent of the deaths of persons served by the DMH (N=423) and 8 percent of the deaths in the non-DMH population (N=25,502) (2=370, df=1, p<.001). Among suicides, mental disorders were reported in only 6 percent of DMH deaths and 4 percent of non-DMH deaths.
Underlying cause of death
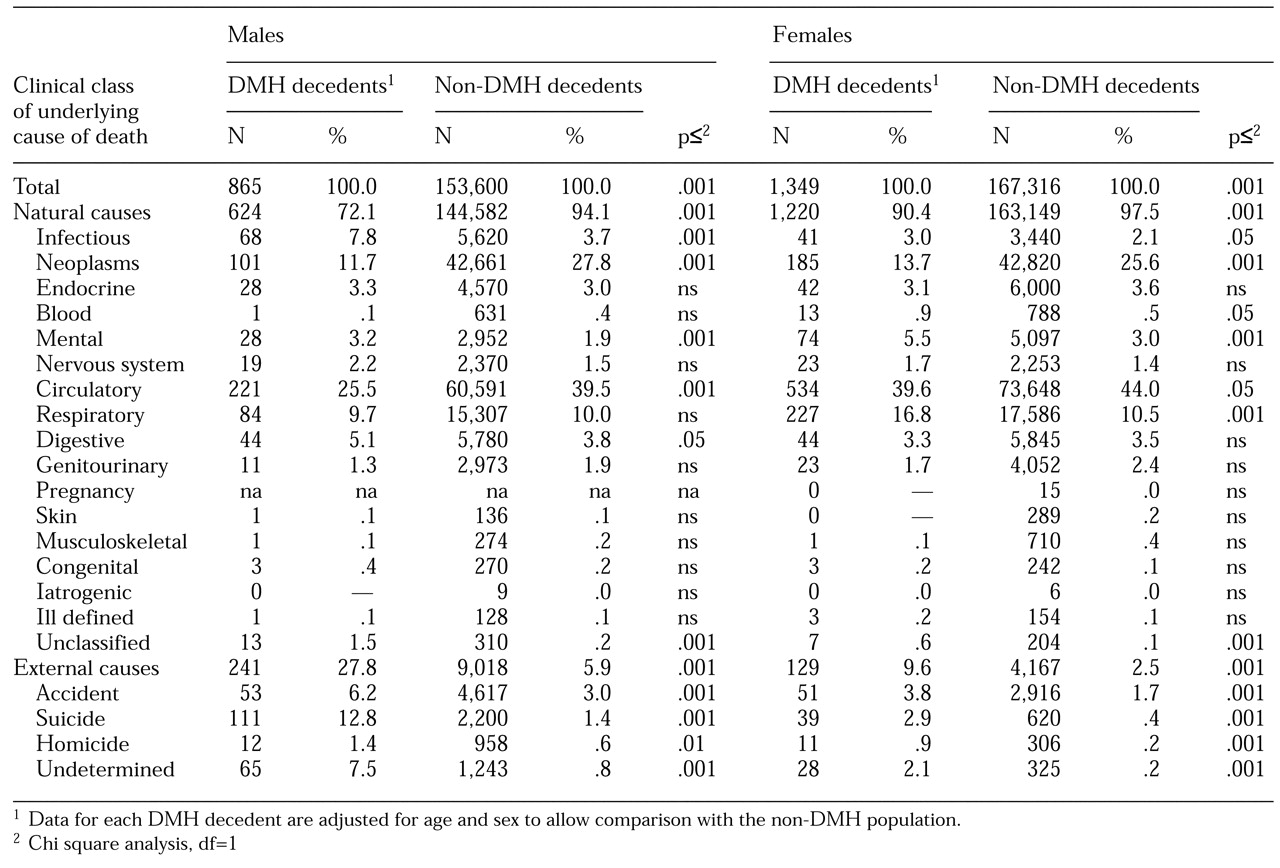
The distribution by sex and underlying cause of death for each person is shown in
Table 2. DMH decedents had a disproportionately high frequency of deaths from external causes, which include accidents, homicides, suicides, and unexplained injuries. The proportion of males in the DMH population with an external cause of death was almost six times higher than the proportion of males in the non-DMH population with an external cause of death (27.8 percent compared with 5.9 percent, (
2=688, df=1, p<.001). For females served by the department of mental health, the proportion of deaths from external causes was nearly four times that for females in the non-DMH population (9.6 percent compared with 2.5 percent, (
2=270, df= 1, p<.001).
Males in the DMH population also had a significantly higher frequency of deaths from infectious and digestive disorders and a significantly lower frequency of deaths from neoplasms and circulatory disorders than males in the non-DMH population. Females in the DMH population were significantly more likely to die from infectious and respiratory disorders and significantly less likely to die from neoplasms and circulatory disorders compared with females in the non-DMH population.
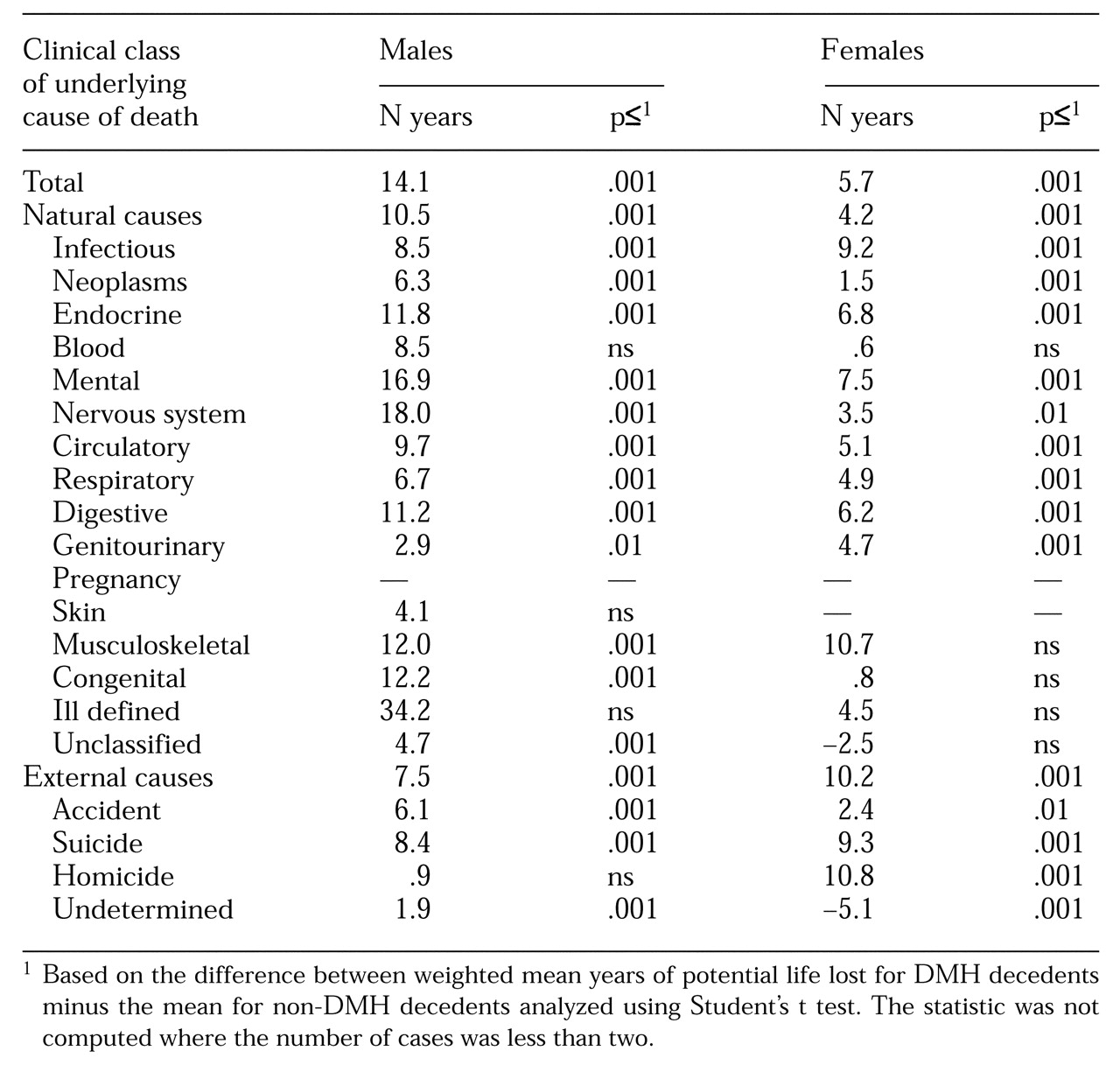
Table 3 summarizes differentials in years of potential life lost by underlying cause of death. Overall, the difference in means between decedents served by DMH and others was 8.8 years (t=65.5, df=1, p<.001). Differentials in years of potential life lost were positive for males and females across all causes of death for which the comparisons were statistically significant. For males in the DMH population, external causes accounted for 39.3 percent of the aggregate years of potential life lost, compared with 13.6 percent for males in the non-DMH population. For females in the DMH population, external causes accounted for 19.1 percent of aggregate years of potential life lost, compared with only 5.3 percent for females in the non-DMH population.
Multiple causes of death
Multiple causes of death are all conditions judged to have contributed to death and reported on the death certificate. Among the 1,890 DMH decedents, a total of 5,577 conditions were mentioned, and 814,011 conditions were mentioned for 320,916 non-DMH decedents.
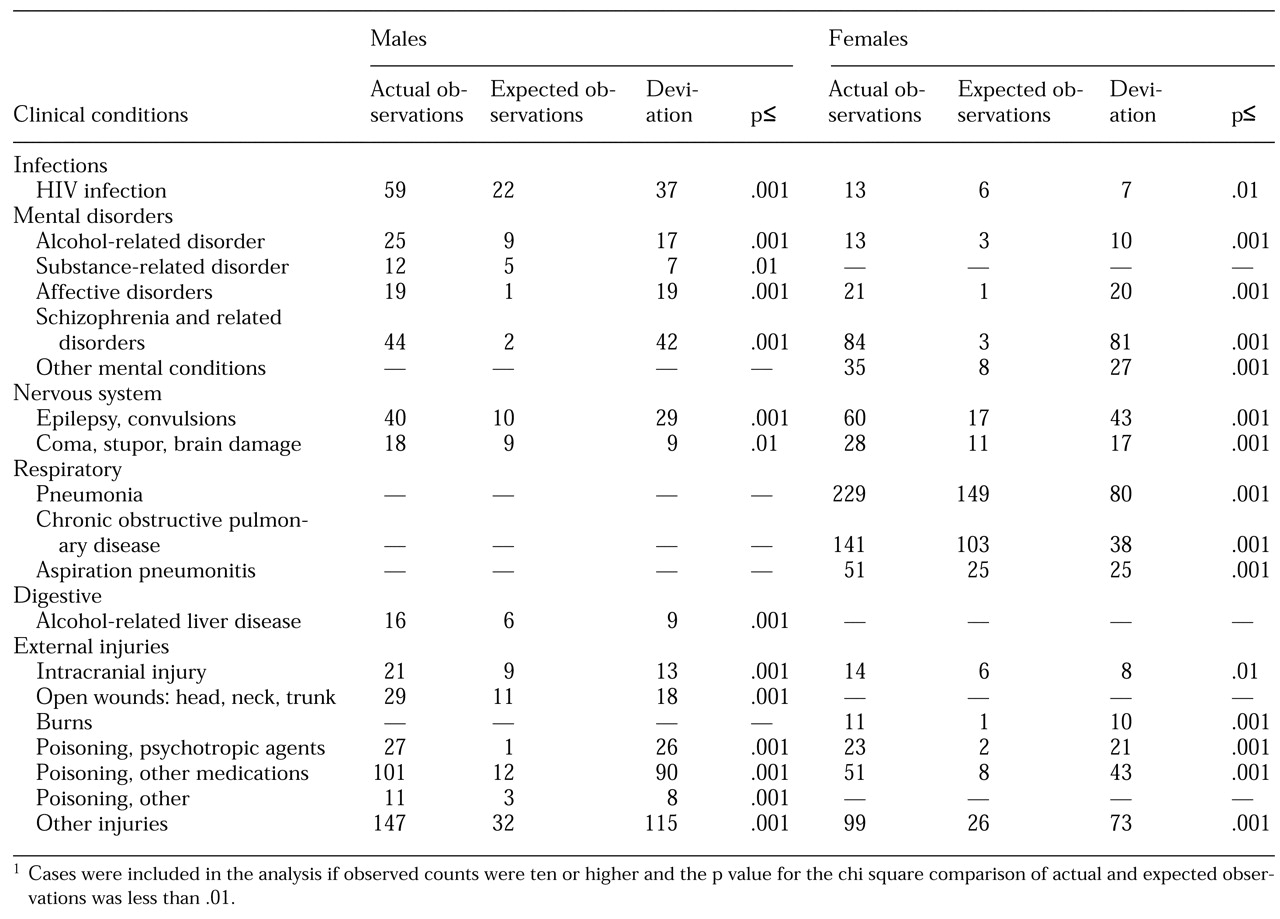
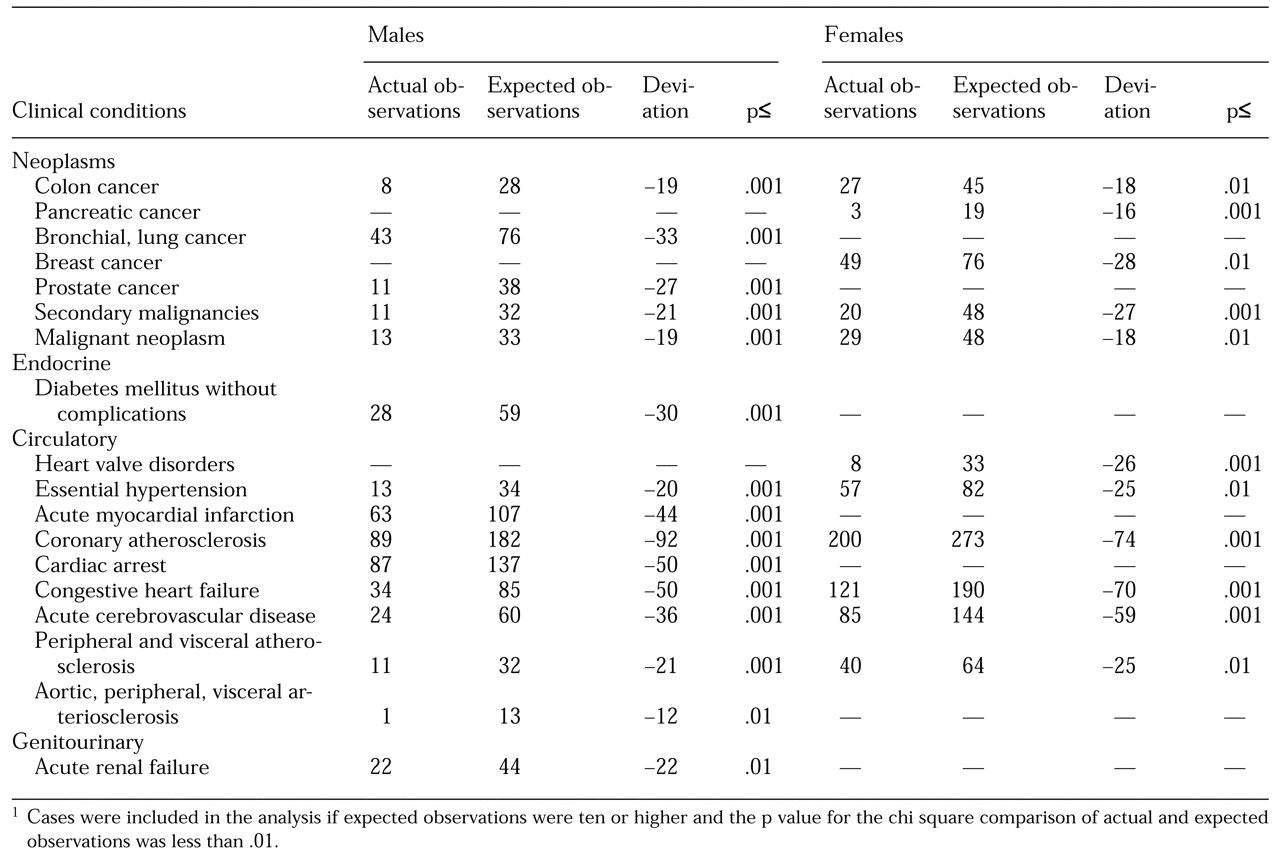
Tables 4 and
5 show conditions reported in the DMH population at significantly higher or lower rates than expected. Chi square statistical significance was based on the hypothesis of homogeneity of the DMH and non-DMH populations.
Table 4 shows conditions overrepresented in the DMH population with ten or more observed mentions and a statistical significance of <.01.
Table 5 shows conditions underrepresented in the DMH population with ten or more expected mentions and a statistical significance of <.01.
To further test the significance of underrepresented conditions shown in
Table 5, we compared separately only cases in which death occurred in hospitals or in which autopsies were performed, circumstances where disease conditions were more likely to be detected. The overall pattern in DMH and non-DMH cases remained, with significantly fewer neoplasms and circulatory disorders among DMH decedents.
Discussion
Our purpose was to describe causes of death that distinguish a contemporary population of persons with serious mental illness from the general population. We did not set out to isolate the excess mortality specifically attributable to particular psychiatric disorders, or to establish the precise causal link between mental disorders and early death. We did not address the prevalence of nonfatal illnesses, which may have a profound impact on the quality of a life but are not captured on death certificates.
Our results are relevant to similar populations in other states, but may not apply to all persons with serious mental illness. Populations served by state mental heath departments share several characteristics associated with early death among those who never married, lived in poverty, were poorly educated, smoked, and lived in urban areas (
32,
33,
34). The interaction of mental illness with these risk factors accounts for some of the results shown here. Populations who were never treated, or who received care entirely in other systems such as the Department of Veterans Affairs or the private sector, may show different outcomes.
The inclusion of an entire DMH registry eliminates sampling error, but other measurement error is possible. Undercounting deaths in the DMH population could have occurred from inconsistencies in names or other key identifiers used in matching, and deaths out of state were not included. We assume these errors do not bias the general findings.
We have described excess mortality in a population of persons with serious mental illness in three ways: frequency of the underlying cause, frequency of multiple-cause conditions, and differential life expectancy. We found high frequencies of deaths due to HIV, alcohol-related disease, and injuries as well as reduced life expectancy across all disease and injury conditions in the DMH population. The high rates of intentional and unintentional poisonings are an area of obvious concern to those who care for this population.
Tables 4 and
5 are derived from data on multiple contributing causes of death. As a new fruit of a methodological advance, these data are important, but they are challenging to interpret. For instance, respiratory disorders are overrepresented in DMH women, but not in DMH men. Similarly, diabetes mellitus without complications, while not significantly different in women, is underrepresented in DMH men—an observation that goes against most clinical experience.
Reduced life expectancy may partly explain conditions underrepresented in the DMH population, as early death would precede the emergence of cancer and circulatory disease, which generally occur at later ages. Additional studies would help determine if underreporting of these conditions is due to inadequate detection or a true low prevalence.
Undetermined causes of death—injuries which cannot be positively judged as accidental or intentional—are remarkably high in the DMH population, even though 88 percent of such deaths were followed by autopsies. This category of undetermined causes of death has not been addressed in previous studies. Medical examiners, aided by circumstantial data from families, health care providers, and others, are able to successfully classify most injury deaths. Consequently, undetermined deaths are very rare in the general population. Such deaths reflect the social isolation and lack of medical care that place seriously mentally ill populations at risk, and reduction in the rate of these deaths would be a potential indication of improvement in these risk factors.
Of special note are rates of mental disorders reported as contributing to death. This rate for DMH decedents was more than twice that among the non-DMH decedents. Yet for this population, selected entirely for the presence of severe and disabling mental illness, we believe the death records understate the impact of these disorders. The low rates of mental disorders reported among suicides suggest this understatement is true for both the DMH and non-DMH populations. Mental health providers are not likely to have direct knowledge of patient deaths, which generally occur outside their settings or after care has ceased. Conversely, medical caregivers and death certifiers may be unaware of a history of mental illness. Even when they are aware, they may not associate a mental illness with medical conditions and subsequent death. Taken together these factors would tend to understate the effects of serious mental illness on life expectancy from death records alone.