By all accounts, contact with the criminal justice system is not a rare experience for people in the United States; it was recently reported that an estimated 47 million people in the United States have an arrest record (
1). Data from the U.S. Bureau of Justice Statistics describing America's correctional population—just one segment of those involved with the criminal justice system—indicate that at the end of 2008 over seven million persons (3.2% of all adults) were on probation, in jail or prison, or on parole (
2). As is well known, however, the risk of such involvement is not evenly distributed throughout the population. Instead, the risk clusters in social groupings whose members share certain individual or social statuses and risk factors. As evidenced by the characteristics of the correctional population, this risk is highly skewed by gender, age, and race. Other data from the U.S. Bureau of Justice Statistics for 2008 indicate that men are roughly ten times more likely than women to be incarcerated and that African Americans are six times more likely than whites to be confined in jail or prison (
3).
Persons with serious mental illnesses are also known to be at high risk of arrest and incarceration. It has been estimated that each year in the United States nearly one million bookings involve persons with mental illnesses (
4). Two longitudinal studies, one examining recipients of services from a state mental health agency (
5) and another focusing on Medicaid beneficiaries with psychiatric illnesses (
6), observed that rates of arrest were between 25% and 28% over a ten-year period. Pandiani and colleagues (
7), using probabilistic population estimation techniques, observed rates of arrest among public mental health service recipients that were roughly 4.5 times higher than those observed in the general population.
The literature about persons with serious mental illness in correctional settings is consistent with this trend. A recent study of jail inmates in Maryland and New York, using the Structured Clinical Interview for DSM-IV, found point prevalence rates of nearly 15% for males and 31% for females (
8)—levels far in excess of those observed in the general population. Substantial system crossover is also observed from the perspective of the mental health system, as evidenced by Theriot and Segal's (
9) report of high levels of previous criminal justice involvement among new clientele at California community mental health centers. System involvement in this population also appears to skew heavily toward the criminal justice system; Morrissey and colleagues (
4) recently estimated that a person with a serious psychiatric illness has a higher likelihood of spending a night in jail than being admitted to an inpatient psychiatric facility.
It is thus well established that persons with serious mental illnesses have high rates of criminal justice involvement, and there is evidence that these rates exceed those observed in the general population. Our study focused on a question that is not addressed in these studies—that is, whether the higher arrest rates observed among persons with mental illnesses are for certain types of offenses or for a broad array of offenses. The answer to this question has important ramifications for framing policy and practice at the interface of the mental health and criminal justice systems. This is particularly true with respect to conceptualizing risk factors and perhaps shifting resources toward offense-specific interventions that might help persons with mental illnesses avoid involvement or reinvolvement with the criminal justice system.
Background
Research focusing on the criminal justice involvement of persons with mental illnesses has been a consistent and increasingly common feature of the psychiatric, psychological, sociological, and services research literature since the early 1970s. A number of perspectives have emerged within this literature, each emphasizing different types of offending behavior. A substantial body of research has shown substance abuse (
10), long-standing antisocial personality disorder (
11), and paranoid delusions (
12,
13) to be risk factors, especially for engaging in violent behaviors, only some of which ever come to the attention of police. Research grounded in this perspective does not typically address the level of risk that these factors pose for other offenses, such as crimes against property.
A second perspective implicates features of the social environments in which many individuals with serious mental illnesses reside. These include known criminogenic risk factors, such as poverty, unemployment, lack of access to prosocial networks, pervasive substance abuse, and concentrations of persons who engage in various antisocial and illegal behaviors (
14,
15,
16,
17,
18). This perspective argues that, to paraphrase Silver's (
19) observation with respect to violent behavior, persons with mental illnesses offend for many of the same reasons that others do in similar social situations, suggesting that the offenses with which they are charged will be roughly the same ones as those in the general population exposed to the same concentration of risk factors. Further evidence for this point, again with respect to violence but arguably generalizable to offending behavior in general, comes from the MacArthur Violence Risk Assessment Study, which found that the likelihood of persons with mental illnesses engaging in violence was similar to that of others in their neighborhoods (
20).
Finally, the criminalization model (
21) traces the source of criminal justice involvement to system failures for persons with mental illnesses. That is, problematic operations of mental health services, the laws and policies driving these services, and the failure of mental health systems to promote continuity of treatment engagement among their clientele often result in decompensation and expressions of deviant behavior among persons with mental illness, and police are often forced to make arrests (
21). This perspective and the jail diversion mechanisms that have been motivated by it tend to focus on low-level offenses, such as disturbing the peace and trespassing, and to deemphasize involvement in criminal activity that is more serious (
22).
As this very brief overview suggests, different conceptual foci tend to lead researchers to emphasize certain offending behaviors, such as violence or low-level misdemeanors, to the exclusion of other kinds of offenses. As a result, there have been few reports that have quantified the excess risk of criminal justice involvement across offense types. Our study represents an effort to provide such offense-specific data, comparing arrest rates on a range of key charges in a cohort of state mental health service recipients with those observed in their state's general population.
Methods
This study used data from a longitudinal study of arrest in a cohort of public mental health service recipients. The cohort included persons aged 18–54 who received inpatient, residential, or case management services from the Massachusetts Department of Mental Health (DMH) during Massachusetts fiscal year 1992 (July 1, 1991, through June 30, 1992) (N=10,742). Their eligibility for receiving services was based on having received a diagnosis of a severe and persistent psychiatric disorder (most typically a psychotic or major affective disorder) of significant duration that caused substantial functional impairment and resulted in a history of multiple hospitalizations over a defined period.
Diagnostic data for this cohort were incomplete, and those available were based on clinical assessments, not structured research diagnostic protocols. However, given the nature of the DMH service eligibility criteria, we are reasonably assured that the cohort in this study is representative of public mental health agency clientele across the nation who were served over this period. Arrests for these individuals were tracked through December 2000, or for just under ten years. This period predates the widespread development of diversion programs in Massachusetts that could potentially have reduced the arrest rate among persons with serious mental illness.
Data
The DMH data included elements allowing matching with the arrest or arraignment data maintained by the Massachusetts Criminal Offender Record Information (CORI) system, the official registry of criminal history data compiled by the Massachusetts Trial Court. These data include all charges and dates of arraignment for all arrests occurring in nonfederal Massachusetts courts. Arrest data spanning this period for the general population were also obtained from the CORI system. Published data from the 1990 U.S. census for Massachusetts were used to construct denominators for general population arrest rates.
This study was reviewed and approved by the Committee for the Protection of Human Subjects in Research at the University of Massachusetts Medical School and by the DMH Central Office Research Review Committee. Access to CORI data also required review of the study by the Massachusetts Trial Court's Criminal History Systems Board, which oversees operation of the CORI system.
Categorizing offenses
In order to compare offense-specific rates of arrest for the DMH cohort with those of the general population, it was first necessary to reduce more than 100 charges in these data to a workable number. To do so, an interdisciplinary team, including a law professor who is also a former trial attorney as well as a researcher with graduate training in criminal justice, identified a set of key legal categories and then grouped offenses within them. The same coding schemes were used for classifying DMH and general population offenses. These categories included felony and misdemeanor crimes against persons and property, crimes against public order, drug-related offenses, crimes against public decency, and assault and battery on a police officer. A number of hard-to-categorize low-level offenses, as well as offenses with low prevalence rates in the service use cohort (for example, firearm charges, motor vehicle violations, and white collar crimes, such as embezzlement) were not included in the analysis. A full listing of the offenses included in each category is provided in the box on this page. (More detail on this process is provided in a study by Fisher and colleagues [
5].)
Comparative approach
Our comparison utilized a retrospective cohort design, in which the offense-specific rates of arrest (that is, the proportion of persons experiencing at least one arrest during the observation period in the various charge categories) for the DMH cohort were compared with those from the general population observed over the same period. The numerators of these rates are the number of persons experiencing at least one arrest for an offense in each category. For the general population, the numerator for a given charge category is the number of persons in the population with an arrest in a given charge category minus the number of DMH cohort members with similar charges. That is, the denominator for the general population (N=3,318,269) is based on the number of persons aged 18–54 counted in the 1990 Federal Census for Massachusetts minus the number of persons in the DMH cohort. The general population rates are thus unaffected by activities in the DMH cohort, although they inevitably include persons with serious mental illness in the population who are not members of this particular service use cohort. The DMH cohort rate is the weighted number of cohort arrestees divided by the total number of cohort members (N=10,742).
Statistical analysis
Simple odd ratios (ORs) were calculated to determine the degree and statistical significance of differences between the service use cohort and the general population in the odds of arrest for each offense category. For any given OR, a 95% confidence interval (CI) not including 1.00 was assumed to be statistically significant at p<.05. Calculations were carried out with Stata, version 10.1.
Results
Sample characteristics
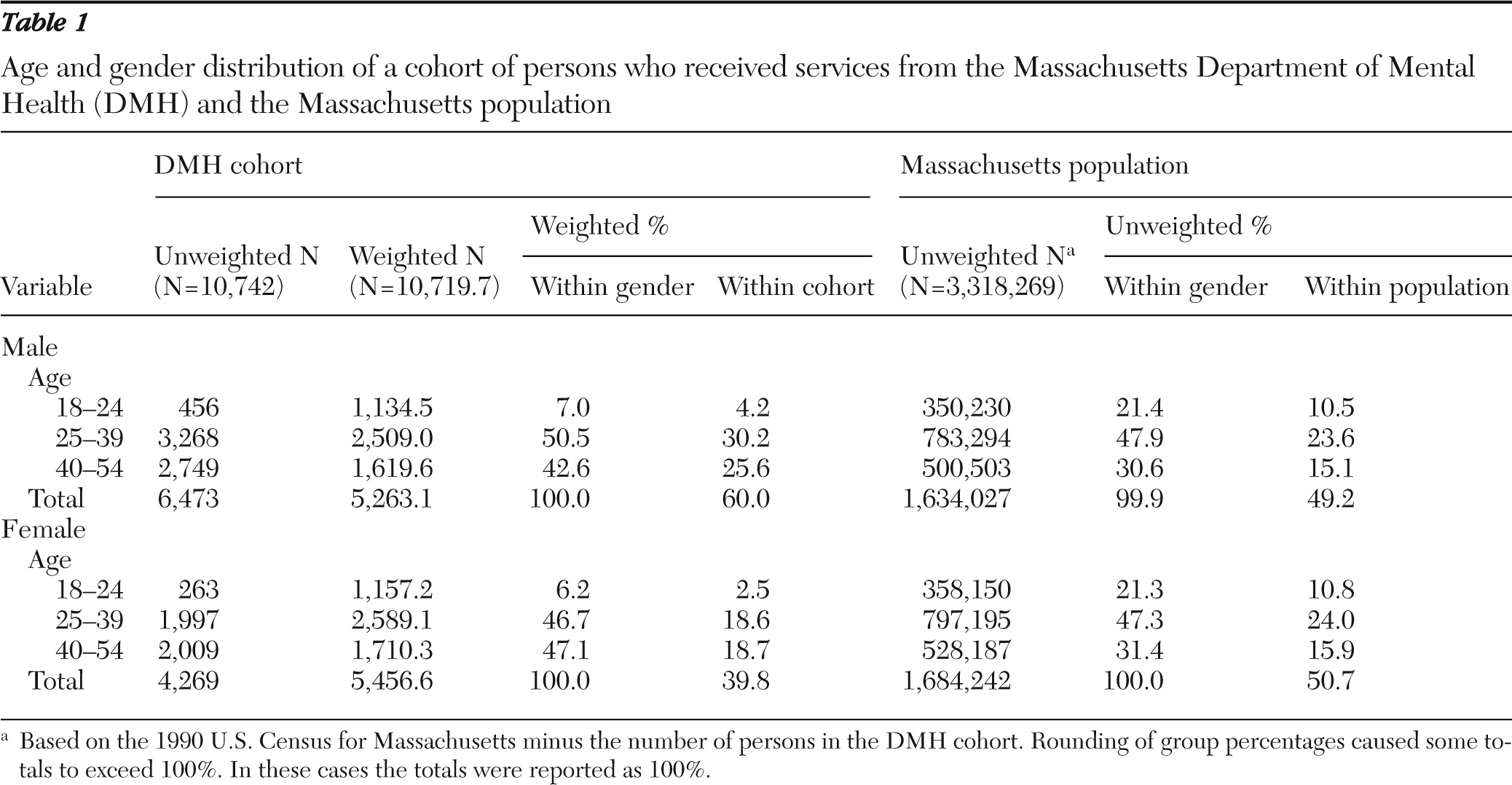
The gender and age breakdowns of the DMH cohort and the Massachusetts population are shown in
Table 1. As indicated in
Table 1, the age and gender, as well as age-within-gender distributions of the two groups were distinctly different. The DMH cohort membership was slightly older and included a much higher percentage of males. Weights based on these differences for each of the six age-by-gender groupings were estimated and used to align the DMH cohort's age and gender distribution with that of the general population. Data on race-ethnicity that had sufficient detail in the various age and gender groups were unavailable in the published census data for this period; thus race-ethnicity was not able to be incorporated in the weighting scheme. Both weighted and unweighted values for the DMH sample are shown in
Table 1.
Overall arrest rates
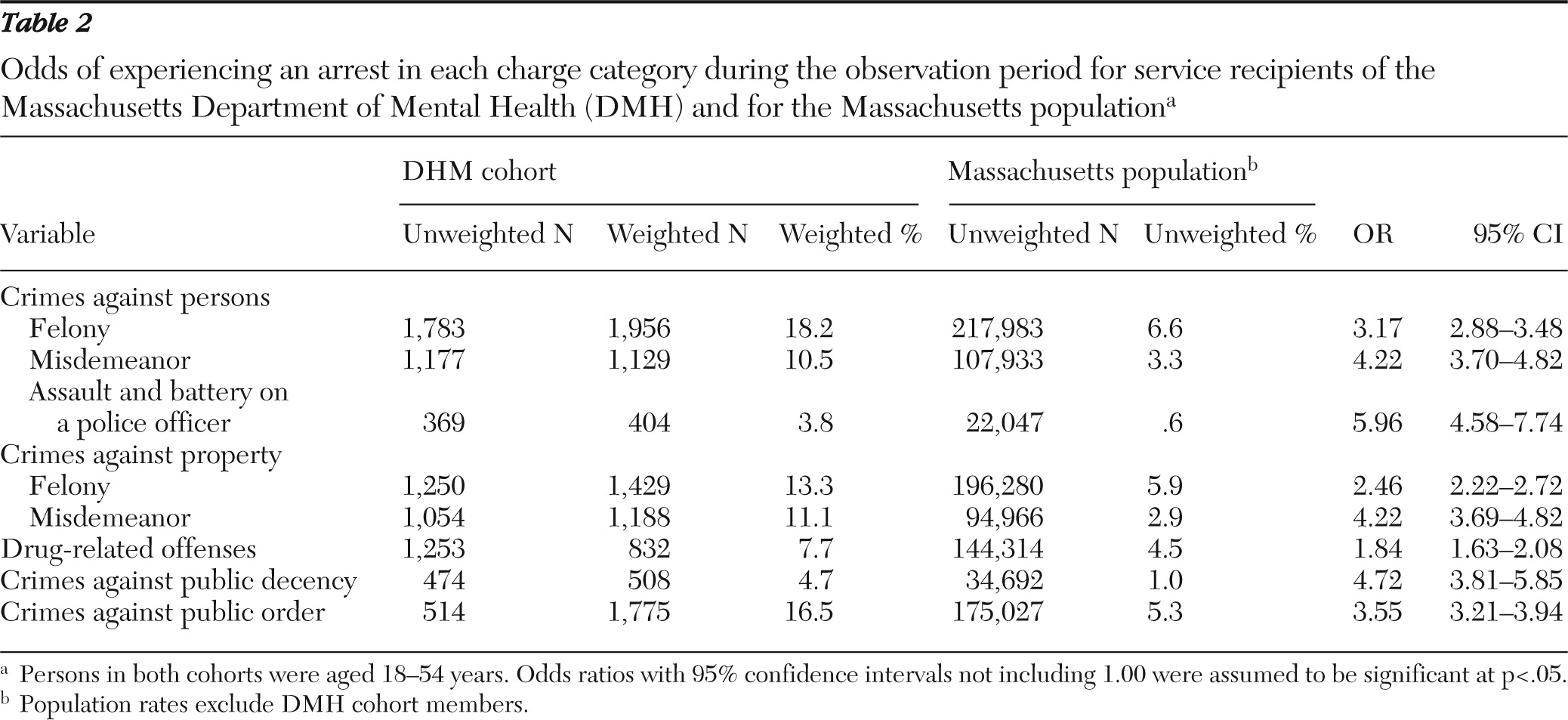
Weighted DMH cohort data were used to compare the odds of experiencing at least one arrest on any of the listed charges in the service use cohort with those of the Massachusetts population. Among the DMH cohort members, 3,662 (32.8%) were arrested at least once during the observation period, compared with 773,792 (23.2%) Massachusetts residents (OR=1.62, 95% CI=1.52–1.72 ), indicating that the cohort members were nearly two-thirds more likely to experience at least one arrest during the observation period. Offense-specific arrest rates for each group, ORs, and 95% CIs are shown in
Table 2.
As indicated in
Table 2, for every offense category, the DMH group's age and gender-adjusted arrest rate was significantly higher than that for the general population, and in some cases, dramatically so. ORs ranged from 1.84 for drug-related offenses to 5.96 for assault and battery on a police officer.
Discussion
Several things should be kept in mind when considering the data presented here. First, arrests represent police officers' perceptions and categorizations of the behaviors they see, which they fit into a legal framework that can be managed by the criminal justice system. Many charges are dropped before prosecution. The data presented here thus represent initial, street-level definitional processes. Whether the outcome of these processes is different for persons with a severe mental illness is unclear. But whatever their social meaning, arrests represent involvement with the criminal justice system, a phenomenon that in and of itself is of extreme importance to mental health authorities seeking to minimize rates of involvement.
Several methodological limitations warrant attention. First, we were unable to adjust for racial and ethnic differences between the DMH cohort and the general population. It is well known that persons from racial or ethnic minority groups are at greatly elevated risk of arrest (
3), and our inability to adjust for this factor represents a serious shortcoming. Moreover, simple demographic adjustment, even when race-ethnicity is included, is clearly inadequate to answer the question of whether being a public mental health services recipient per se places persons at greater risk of arrest. As we noted earlier, such individuals encounter a host of potentially criminogenic socioenvironmental and socioeconomic risk factors. In order to adjust for these factors one would need to adopt the strategy of the MacArthur Violence Risk Assessment Study (
20), comparing cohort members with neighbors exposed to the same factors. This was clearly beyond the scope of our project.
Also, our data did not capture adequately the differences between the DMH cohort and the general public with respect to time in which the person is at risk of arrest. Persons such as the cohort's members experience a range of incapacitating events, including arrest and psychiatric hospitalization, which may be less common in the general population. Thus the time in which the person is at risk of arrest may be lower for persons with mental illnesses than for the general population.
An additional concern is the age of the data—a problem plaguing many longitudinal studies. Since the time spanned by the observation period, numerous diversion mechanisms have been developed at the interface of the mental health and criminal justice systems that, had they been in place in the 1990s, might have affected the arrest rates of the service use cohort. For our purposes this can be seen as both a curse and a blessing; by observing activity in the prediversion era we can assume that these rates are "uncontaminated" by the effects of those services. Comparisons with a similar cohort identified in the early 2000s would be interesting in this regard.
Finally, the general population comparison group did not exclude all persons who are mental health services recipients. There were undoubtedly recipients who happened not to receive services in the index year as well as persons who had not yet begun receiving services. However, this number is presumably small relative to the entire Massachusetts population and unlikely to have significantly biased our results.
With those considerations in mind, we shift attention to the implications of the data presented here. These data show arrest to be a far more common experience for persons in the DMH cohort than it was for the general population, both overall and within all of the offense categories shown here. However, with the exception of assault and battery on a police officer, the largest ORs were associated with misdemeanor crimes against persons and property and against public order and public decency, which typify the low-level misdemeanors that are the focus of most diversion efforts. But the importance of the felony charges is not to be overlooked. An arrest and conviction for one of the misdemeanor charges may have an impact on individuals' housing, employment, and other prospects but lack serious long-term consequences and few public safety implications. Felony charges, on the other hand, may be associated with events that significantly affect other persons' health or property, and convictions on these charges can lead to long-term incarceration in settings where mental health services may be inadequate (
23,
24). These offenses are not generally the focus of diversion programs; nonetheless, understanding the pathways to involvement in these events and the individual, environmental, and systemic factors associated with them is critical given their societal importance.
Conclusions
Administrative data such as those used in this study have the advantage of providing glimpses of large populations and providing information on population and subpopulation offending rates and patterns. As such, they can inform policy and service delivery discussions. However, the lack of key variables—detailed diagnostic profiles, information on changing social networks and environments, routine activities, use of mental health services, continuity of treatment, and other factors—limits the extent to which important causal relationships can be explored. The significance of this problem argues for the development of a research agenda that includes longitudinal studies featuring comprehensive interview protocols coupled with administrative data on treatment, employment, criminal justice involvement, and other factors that are routinely captured over time. Understanding what differentiates persons with intensive justice involvement from those with little or no such involvement is essential if the excess risk of arrest faced by public mental health services recipients is to be reduced.
Acknowledgments and disclosures
This study was supported by grant 1R01-MH65615 from the National Institute of Mental Health and by the Center for Behavioral Health and Criminal Justice Research and the Sidney R. Baer, Jr. Foundation. The authors thank Jeffrey Swanson, Ph.D., for helpful comments on an earlier version of this article. This work is dedicated to our beloved colleague, the late Dr. Steven Banks, without whom none of these analyses could have been undertaken.
The authors report no competing interests.