Addressing cultural issues associated with health care among patients with severe mental disorders is part of recovery-oriented care (
1). This is in line with the concept of “psychiatry for the person,” which has been advanced in recent years by the World Psychiatric Association. The concept places the patient's whole person at the center of clinical care and health promotion, at both individual and community levels (
2).
Obviously, religion is part of the cultural dimension of humans. Religion, in its broadest sense, encompasses spirituality (concern with the transcendent and with the significance and meaning of life and similar issues) and religiousness (specific behavioral, social, and doctrinal practices and denominational characteristics). Spirituality and religiousness have been identified as pivotal in the psychological process of recovery from severe mental disorders such as schizophrenia, in that they may provide meaning and hope in suffering (
3,
4). Nevertheless, ways of addressing religion in clinical settings remain to be established, particularly among individuals with severe disorders, such as psychosis (
5).
Some studies have shown the importance of religion to patients with psychosis. A study of 406 persons with persistent mental illness found that 80% used religious beliefs or practices to cope with daily difficulties or frustrations, particularly those who were experiencing more severe symptoms (
6). Another study of 58 persons with severe mental disorders showed that they used positive religious coping strategies; however, some reported feeling ignored, judged, or condemned by the religious community (
7). Recently, our research group conducted a study involving outpatients with schizophrenia (
8). We found a higher prevalence of positive religious coping compared with negative religious coping (that is, a negative effect of religion, such as inducing spiritual despair or excessive guilt). Also, treatment and illness representation—that is, patients' explanatory models—frequently involved a spiritual component that was likely to influence treatment adherence (
9). These results were further replicated by our research group in Quebec, Canada (
10).
These findings suggest that a spiritual assessment could introduce positive issues into the clinical care of patients with schizophrenia. However, the effect of such an intervention has not been evaluated. As recently noted by Baetz and Toews (
5), research on practical psychospiritual interventions for patients with psychiatric disorders is limited. It is known that clinicians rarely address religious or spiritual issues with their patients. Further investigation is required to understand what patients seek, and more specifically, the possibility that a subgroup of patients may not wish to share religious or spiritual issues with clinicians. In addition, it is still not evident that such an intervention would be applicable in clinical practice.
The aim of this study was to determine, in a randomized protocol, whether patients accept and tolerate a spiritual assessment by their psychiatrist and to elicit psychiatrists' feedback on the process. The study also assessed primary outcomes at three months (treatment adherence and satisfaction with care, as measured by the strength of the therapeutic alliance), as well as some secondary outcomes. We also conducted a thematic analysis of existential and interpersonal issues that were raised during the spiritual assessment and reported by the participating psychiatrists.
Methods
Sample
The outpatient clinics in which the sample was recruited between May 2007 and November 2008 are affiliated with the Department of Psychiatry at the University Hospitals of Geneva. They offer supportive psychotherapy, somatic treatments, and rehabilitation. Study objectives were described in staff meetings, after which resident psychiatrists were individually asked to participate. They were in their postgraduate years—that is, they had three to eight years of residential training in psychiatry and psychotherapy. Of the 11 psychiatrists invited to participate, the first eight who accepted were included.
To ensure that psychiatrists were familiar with their patients, only patients who were treated by their current psychiatrists for at least three months were included in the study. All patients were stable—that is, they had not been hospitalized in the previous six months. Patients were excluded if their clinical condition prevented them from participating in the interviews. The study was approved by the Ethics Committee of the University Hospitals of Geneva. Participants (both patients and psychiatrists) signed a detailed written consent form.
Randomization
In each clinic, about 200 patients were eligible to participate (total of about 800 eligible patients). To ensure random selection, all eligible patients of each psychiatrist were assigned a random number and then listed in numerical order. Up to 14 patients per clinician were selected (psychiatrists who worked part-time had fewer patients in the study). The first seven patients on the numerical list were assigned to the intervention group, which receive standard treatment plus a spiritual assessment by their psychiatrist. The last seven patients on the list were assigned to the control group, which received only standard treatment. [A flowchart illustrating recruitment and assignment is available in an online supplement to this article at
ps.psychiatryonline.org.] Of 117 patients recruited, 33 (28%) refused to participate. The final sample included 84 outpatients, with ages ranging from 20 to 60 years, who met
ICD-10 (
11) diagnostic criteria for schizophrenia or other nonaffective psychoses.
Psychiatrists' training
Psychiatrists completed an attitude questionnaire about the integration of the spiritual dimension into clinical practice. They then attended a 90-minute training session during which they were informed about the rationale for taking into account the spiritual dimension in the treatment of patients with schizophrenia and how to conduct a spiritual assessment. They were made aware of how their own religious and spiritual experiences could influence their identity and worldview, as well as how their attitudes toward such experiences might introduce biases into clinical assessment and treatment. Finally, psychiatrists were reminded to show respect for patients with different religious and spiritual backgrounds.
Initial assessment
The Mini-International Neuropsychiatric Interview (
12) was used to assess current or past diagnosable psychiatric illnesses. The Positive and Negative Syndrome Scale (
13) was also administered to patients. Psychosocial adaptation was measured by the Global Assessment of Functioning (
14), the Social Functioning Questionnaire (
15), and the World Health Organization Quality of Life instrument (WHOQOL-BREF) (
16). Satisfaction with care was evaluated with the Client Satisfaction Questionnaire (CSQ) (
17). A measure of recovery from mental illness, the Recovery Assessment Scale (
18), was also used. Number of hospitalizations, number of days spent in the hospital, history of suicide attempts, treatment adherence (as assessed by the rate of attendance at clinical appointments during the past three months) were also documented, and the Medication Adherence Rating Scale was used (
19). The therapeutic relationship between the therapist and the patient was assessed with the patient and therapist versions of the Working Alliance Inventory (French translation) (
20), which was also considered a measure of the patient's satisfaction with care. Assessment was performed by trained psychologists blind to the patient's group assignment.
Intervention
Patients in the intervention group were assessed by their psychiatrist, who used a semistructured interview guided by the topics listed in the box on this page (
21). After each assessment, the psychiatrist met with two of the authors (PH and P-YB), a psychiatrist and a psychologist of religion, in a supervisory session at which the individual patient was discussed for ten to 40 minutes, depending on the clinical context. During these meetings, the participating psychiatrist reported the outcome of his or her spiritual assessment and was given guidance and advice, similar to clinical coaching; when needed, a more thorough discussion from a psychotherapeutic perspective was undertaken.
Assessment of the intervention
At the supervision session, psychiatrists' suggestions for treatment that arose from information that they had gathered in the spiritual assessment were documented. Four of the authors (PH, P-YB, SM, and IR) used a consensus process to categorize the suggestions into themes (
22) and then rated them according to their importance: likely to be helpful or should be carefully monitored over time (for example, foster socialization of the patient); a subject of importance (for example, discussion of the patient's religion as an important identity component); and a major influence in the patient's life, in care, or in the therapeutic relationship (for example, discussion of a patient's religious belief that competes with pharmacological treatment and that is likely to lead to nonadherence and relapse).
Before the spiritual assessment, a semistructured interview and visual-analogue scales were used to evaluate patients' willingness to undergo the assessment. After the assessment, similar methods were used to assess their acceptance of and satisfaction with the procedure. A semistructured interview and visual-analogue scales were also used to evaluate each clinician's perceptions of the spiritual assessment conducted for each patient.
Control group
For the control group, psychiatrists were instructed to avoid speaking about religious issues during the three-month follow-up period unless patients spontaneously brought up the subject.
Three-month follow-up
Three months after the initial assessment, the primary outcome measures—the Medication Adherence Rating Scale (
19) and Working Alliance Inventory (
20)—were readministered, as were the clinical and psychosocial measures described above. As noted above, patients' and clinicians' subjective opinions about the spiritual assessment were elicited by use of open questions with a quantitative evaluation by visual-analogue scales. Regular attendance at clinical appointments was monitored and compared with attendance during the period before the initial assessment.
Statistical analysis
Comparisons at baseline between the intervention and control groups were analyzed with chi square and independent t tests, with a probability level of .05. Linear mixed models with maximum likelihood estimation were used to analyze between-group differences in outcome measures, with treatment time as a fixed effect and the individual a random effect, as described elsewhere (
23). The subject-specific random intercept was included in order to relax the assumption of conditional independence in the responses of the same person. Comparisons of patients' outcome measures between psychiatrists were analyzed with chi square tests, Wilcoxon rank tests, and Kruskal-Wallis tests, with a probability level of .05. Statistical analyses were performed with Stata, version 10.
Results
Initial assessment
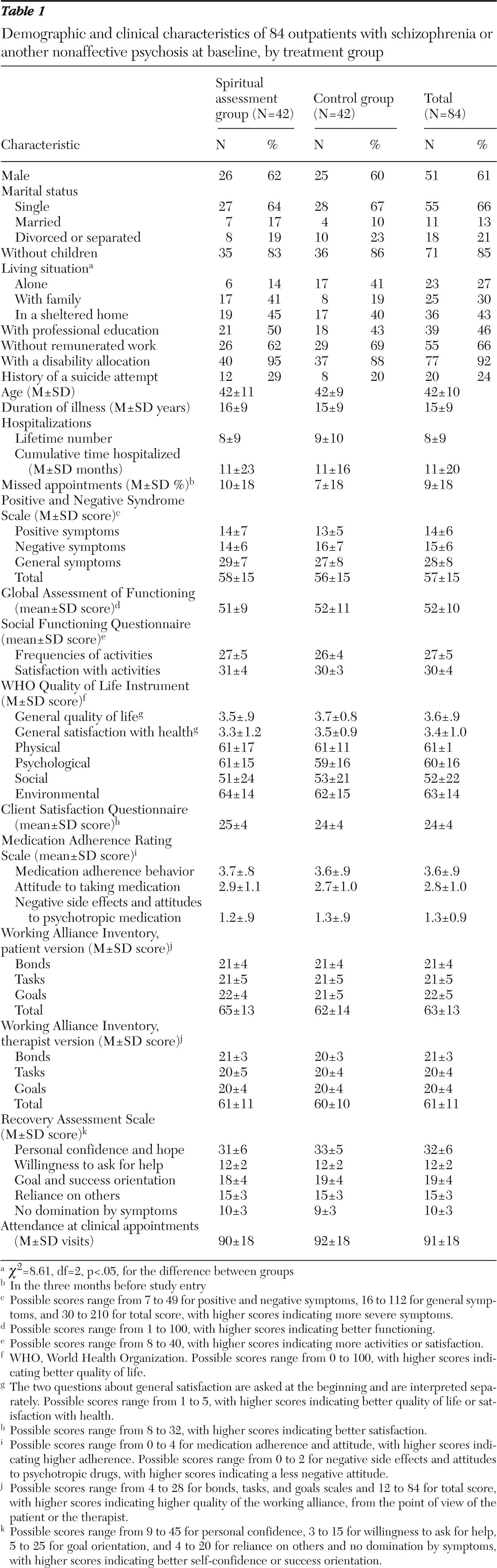
Sociodemographic and clinical data for the two groups are presented in
Table 1. No significant between-group differences were found for any variable except living alone: a greater proportion of patients in the control group lived alone (
χ2=8.61, df=2, p<.05).
Acceptance of the intervention
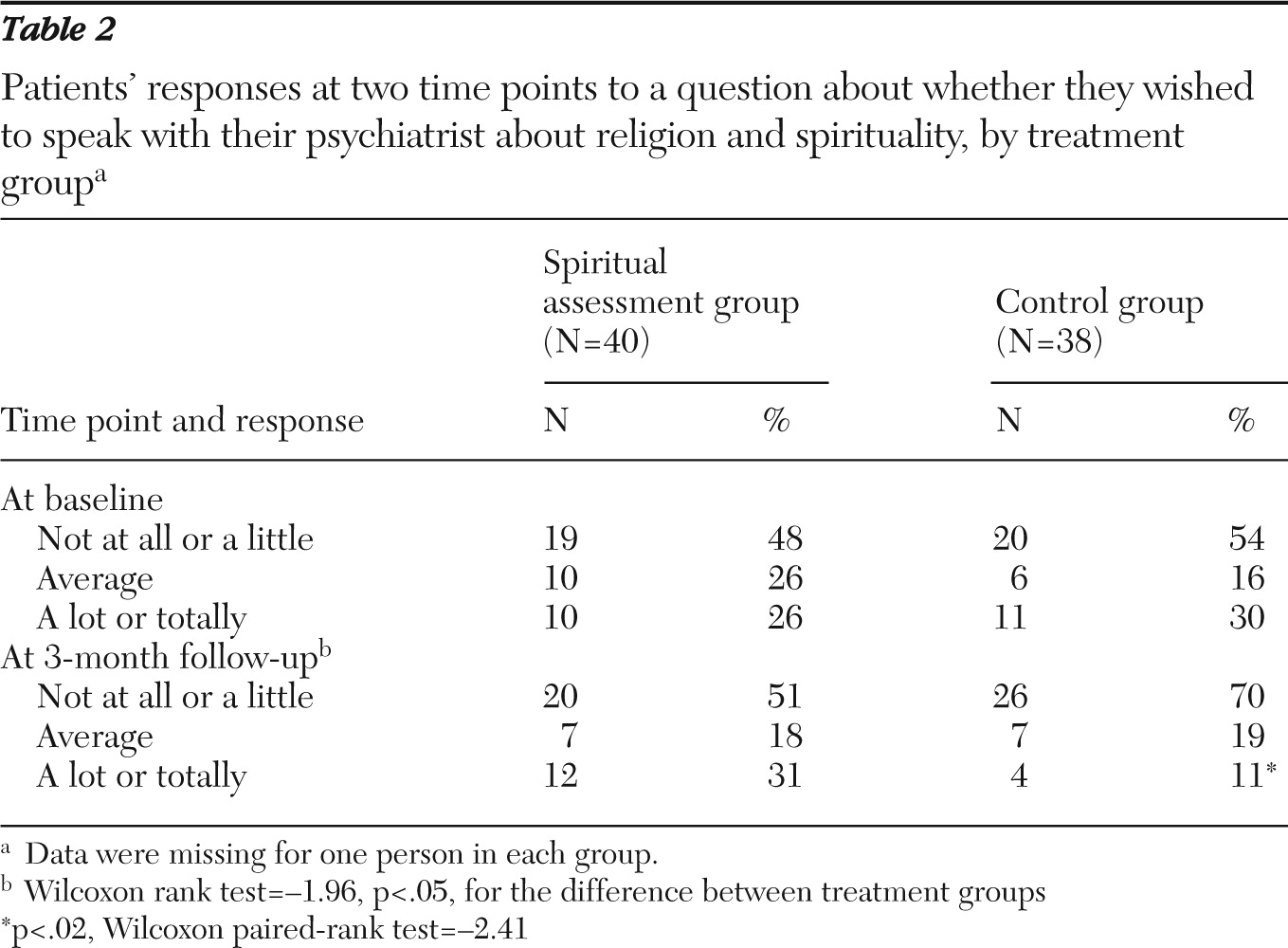
Overall, spiritual assessment was well tolerated by the patients, and none of them spontaneously expressed concerns to their psychiatrists. Patients' desire to address spiritual issues was independent of psychiatrists'. Psychiatrists did not consider this intervention as contraindicated for any patient. Five patients reported that their religious beliefs conflicted with their expectations for treatment, although such conflict was reported in only two of the postassessment supervision sessions. As shown in
Table 2, at baseline more than a quarter of patients in both groups strongly wished to discuss religion and spirituality with their psychiatrist. At the three-month follow-up, patients in the spiritual assessment group maintained their interest, whereas many patients from the control group were no longer interested. Moreover, only three patients (8%) in the intervention group missed appointments during the three-month follow-up, compared with ten patients (26%) in the control group (
χ2=4.97, df=1, p=.03).
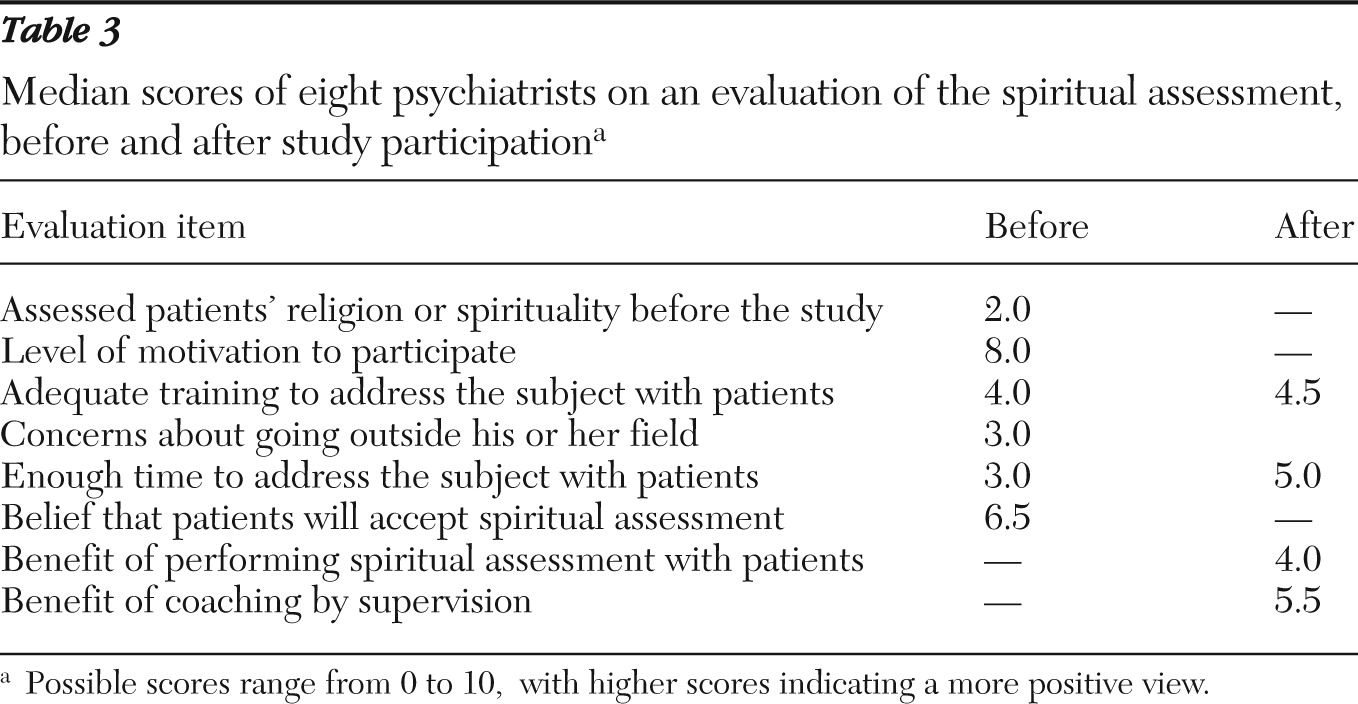
Table 3 presents data from the psychiatrists' evaluation of the spiritual assessment. Before the study, religion was rarely discussed with patients. Clinicians reported being highly motivated to assess spirituality, despite a lack of training and time. However, after the study they did not seem enthusiastic. Most of their answers about the study were politely in the midrange, both for the practice of spiritual assessment itself and the supervision. Furthermore, some clinicians were concerned about going outside their field—that is, becoming involved in topics pertaining to chaplains or clergy. This finding supports the supervisors' impression that not all the psychiatrists were greatly interested in the process.
For each patient, the psychiatrist evaluated the contribution to clinical care of the spiritual assessment and supervision by using a visual-analogue scale, with a range from 0, no contribution, to 10, essential. The overall median was 4. For the first quarter of patients assessed, median scores were 1 or below, whereas median scores were 6 or higher for the last quarter of patients assessed. The scores indicate that at least for the latter patients, clinicians considered the spiritual assessment and supervision important. A significant correlation was found between the positive impact of the intervention expressed during supervision and the value that psychiatrists attributed to the intervention (r=.42, p<.01), indicating that interventions with better outcomes were more appreciated by the psychiatrists.
Outcomes at three months
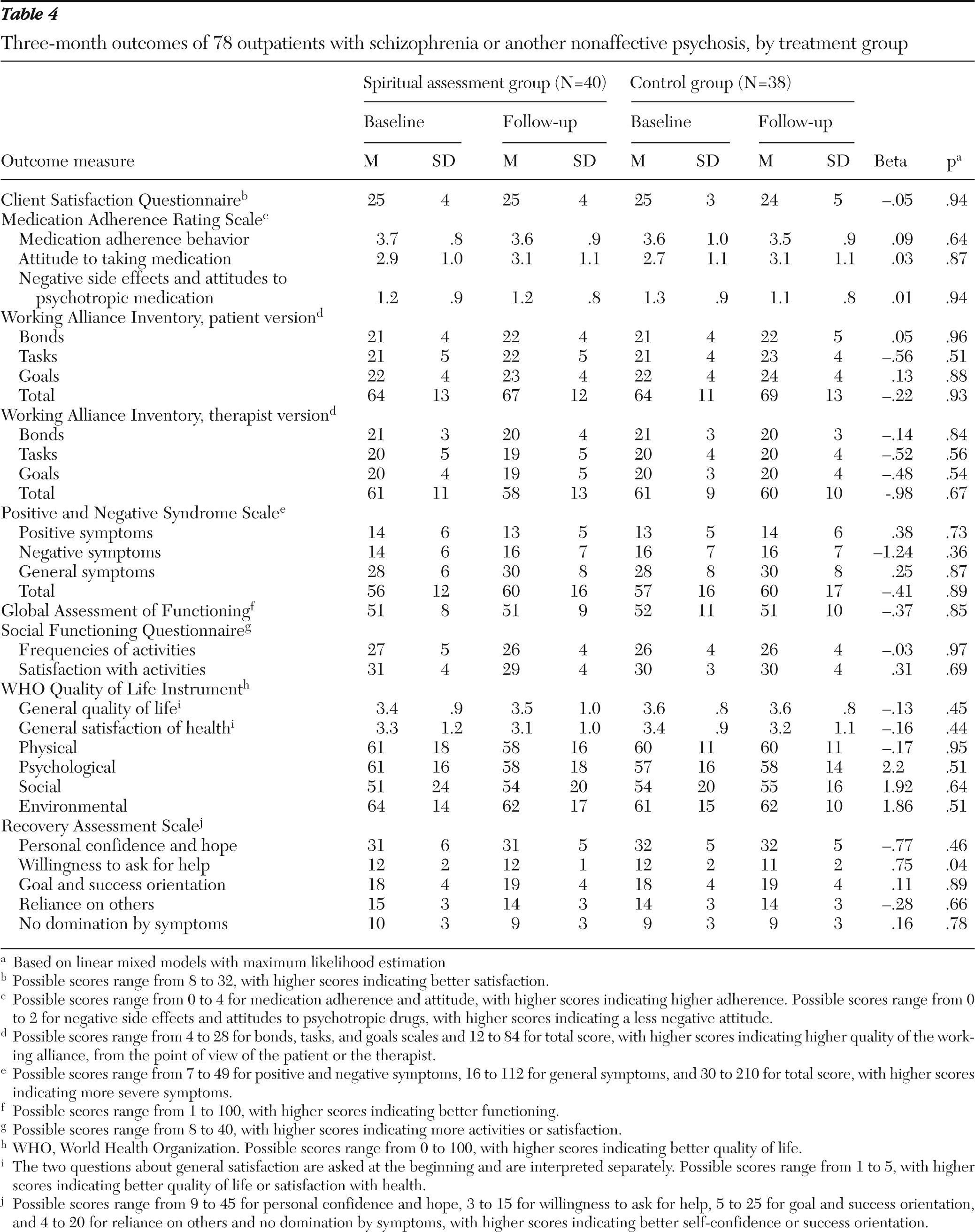
Data on outcome measures are presented in
Table 4. After three months, contrary to our expectations, no differences were found across groups in primary and secondary outcome measures, except for “willingness to ask for help” (as assessed by the Recovery Assessment Scale), which remained higher in the intervention group than the control group. Also, the intervention group had better attendance at clinical appointments during the follow-up period (t=−2.45, df=1, p=.02).
We also compared patients' outcome in regard to their investment in spirituality. We selected patients from both groups for whom religion was important according to their scores on the item “importance of beliefs in daily life” in the WHOQOL-BREF questionnaire (17 patients in the intervention group and 15 in the control group). We found no significant between-group difference. We also selected the 28 patients from the intervention group whose psychiatrist had proposed suggestions for their treatment in the postassessment supervision session and compared their outcomes with those of all patients in control group. No significant difference was found between groups. Finally, we evaluated outcomes by psychiatrist and found no significant effect—that is, no psychiatrist obtained better outcomes than others.
Themes raised in the assessment
At the supervision session, psychiatrists made suggestions for treatment related to the spiritual assessment for 28 of the 42 patients (67%). The thematic analysis of suggestions yielded six themes. In order of importance, the themes were support positive coping (most frequent); work on identity and values; differentiate delusion from faith and work on this issue; mobilize the patient toward clergy, chaplains, or a religious community; work on negative religious coping; and work on representations of psychiatric disorder and treatment from a religious perspective. [An appendix with ratings of importance and examples of the suggestions for treatment is available as an online supplement at
ps.psychiatryonline.org.]
Discussion
This study evaluated outcomes of patients with psychotic disorders who agreed to a spiritual assessment by their psychiatrist. The assessment was well tolerated by all patients. Moreover, their wish to discuss religious matters with their psychiatrist persisted after the spiritual assessment. Even though clinicians acknowledged the usefulness of the supervision for some patients, especially when religion was important in the clinical care of a patient, they reported only moderate interest in conducting spiritual assessments in clinical settings. No differences between the intervention and control groups in the primary outcome measures—the Medication Adherence Rating Scale and the Working Alliance Inventory (used as an indicator of patients' satisfaction with care)—were observed at the three-month follow-up. However, attendance at clinical appointments during the follow-up period was significantly higher in the intervention group. The same results were found when analyses were restricted to patients who had a greater investment in religion and to patients whose psychiatrist had proposed suggestions for their treatment based on the information gathered in the assessment.
Patient-level factors may explain some outcomes. Patients in this study had chronic schizophrenia—some for more than 30 years. In this context, their clinical and social conditions were not likely to change. However, patients' willingness to ask for help remained high at baseline and follow-up in the intervention group, and it fell off slightly but significantly in the control group. Appointment attendance was also significantly higher in the intervention group than in the control group. The ability to ask for help has been associated with a potentially higher recovery rate in schizophrenia, which is attributable to better integrative and less avoidant coping strategies (
24). For patients who are believers, having a relationship with a spiritual figure can provide a sense of security in the face of distress (
25). Thus supporting patients' positive religious coping, which was the most frequent suggestion for treatment in this study (suggested for 17 patients), may foster more secure attachment patterns for some patients. In a broader sense, the value attributed to positive religious coping in this study highlights the relevance of addressing cultural issues, such as religion and spirituality, in patient care, even though our expectation was not supported that satisfaction with care (a factor likely to change) would improve after spiritual assessment.
Factors related to the psychiatrists may also partly explain our overall results. The clinicians in the study were mostly young residents, and most had not received extensive training about the interface between culture and medicine. They found the idea of performing a spiritual assessment novel because they had not conducted anything similar in their work with patients. The 90-minute training session and the individual supervision sessions may not have been sufficient to familiarize them with this topic. Even though we observed clinicians express interest in information obtained in the assessment and in the coaching provided in supervision sessions, it may be that in the relatively short time they had spent with these patients, complex issues such as those raised in the spiritual assessment were not fully explored.
To our knowledge, this study is the first to examine an individual spiritual intervention for patients with psychosis. Most studies of the interface between psychosis and religion address ways to disentangle religious delusions from healthy spirituality and religiousness (
26) or examine group treatments involving spirituality (
27). There is little evidence-based knowledge about how to intervene effectively in regard to religious issues with patients who have psychiatric disorders (
5). Short interviews, such as HOPE (source of Hope or meaning, Organized religion, Personal spirituality or Practices, and Effect on medical care or End of life) (
28), have been developed; nevertheless, further studies are needed to evaluate their implementation in populations with psychosis.
The study had some limitations. First, cultural context is likely to have influenced the results, and the study should be replicated in other areas. Only patients in the intervention group received additional attention from the psychiatrists, who explored and discussed patients' personal beliefs, which may have introduced significant bias. The additional time invested by the psychiatrists could have made a difference, an effect having little to do with the focus on spiritual issues. Furthermore, psychiatrists received supervision only for patients in the intervention group, and supervision itself could have altered patients' outcomes. Patients signed an informed consent form to participate in the study and then were randomly assigned to the intervention or control group. The latter patients might have been disappointed at not having received a spiritual assessment, which may have altered their evaluations.
Other limitations were noted above: the short training session and the lack of commitment among some clinicians. Issues raised in a spiritual assessment might best be addressed in repeated supervision sessions over several months, as in psychotherapy training. Thus additional supervision may have led to different outcomes. The themes raised in the supervision session were categorized by consensus. The themes overlap to some extent (see examples in the online appendix). Thus the categorization of themes should be considered tentative. Finally, the high refusal rate should be noted. Some potential participants may have been ill at ease at the prospect of talking about sensitive issues, such as treatment incompatibility with the person directly responsible for their care.
Conclusions
Despite these limitations, the qualitative results of this study support a more person-centered approach to mental health care as recommended by the World Psychiatric Association. “Psychiatry for the person” emphasizes the need to assess both illness and protective factors (resilience, resources, and supports) (
2). Baetz and Toews (
5) noted that that evidence-based knowledge is lacking about how to manage religious issues with psychiatric patients. From this perspective, we showed that a spiritual assessment was well tolerated by patients with psychosis and that a large portion of the assessments raised issues judged to be important to clinical care. Some of these issues are easy to incorporate in usual clinical settings, such as supporting patients' religious coping or helping mobilize them toward clergy or a religious group in the community. Other issues, such as use of religious topics to help patients work on identity, may be more difficult to implement because of their psychotherapeutic nature. Other issues warrant immediate concern because of their clinical implications, such as disentangling faith from religious delusion or addressing a patient's belief that might lead to rejection of treatment. The moderate interest in spiritual assessment that we noted among many psychiatrists underscores the need for incorporating training in cultural issues early in the medical school curriculum. Also, more in-depth and repeated supervision sessions devoted to this topic should be implemented and assessed, both in research settings and in the clinical practice of residents, in order to better address religious and spiritual issues.
Acknowledgments and disclosures
This study was supported by grant 325100-114136 from the Swiss National Science Foundation.
The authors report no competing interests.