Illicit drug and alcohol abuse and dependence (substance use disorders) have harmful effects on individuals and society (
1). Individuals with substance use disorders have higher rates of suicide attempts than individuals in the general population (
2–
5), high health care expenses (
6), and significant disability (
7). In the U.S. population age 12 and over, 8%reported illicit drug use and 23% reported binge drinking in the past month (
8). In racial-ethnic minority populations, blacks have higher rates of illicit drug use than whites and similar rates of alcohol abuse, and Latinos have rates of illicit drug use and alcohol abuse that are similar to those of whites (
9).
Studies have consistently found disparities in access to and utilization and quality of mental health care (
10–
13) and other types of health services (
14–
16). However, findings on substance abuse treatment disparities have been mixed. Studies using data from the National Survey on Drug Use and Health (NSDUH) have identified Latino-white disparities in rates of substance abuse treatment for certain years (
17) but not others (
18,
19). Other studies of specific populations have identified black-white and Latino-white disparities in needed treatment among the uninsured population (
20) and black-white disparities among problem drinkers (
21). These discrepant results are partly a result of differing populations and definitions of need and receipt of substance abuse treatment (
22), but they are also related to differences in accounting for the confounding of the relationship between race-ethnicity and substance abuse treatment by income, severity of the disorder, insurance, participation in social service systems, and interaction with the criminal justice system.
Further exploration of the association between race-ethnicity and substance abuse treatment may help to shed light on these inconsistent findings. In this study, we assessed whether criminal history and socioeconomic status reduce or contribute to disparities. We describe a conceptual framework to ground the measurement of racial-ethnic disparities in substance abuse treatment.
The need to support drug use leads some individuals to resort to petty theft or other crimes that initiate contact with the criminal justice system (
23). Individuals who have been incarcerated are likely to have a history of illicit drug or alcohol abuse (
24,
25), and, as expected, illicit drug abusers are more likely than nonabusers to have been arrested for committing a crime (
26). Eighty percent of state prisoners and 70% of federal prisoners reported ever using illicit drugs, and 50% of state and federal prisoners reported using alcohol or drugs when they committed their offense (
24,
25).
Many individuals receive substance abuse treatment only after committing a criminal offense—via court mandate, as a condition of parole or probation supervision, or as a condition of regaining employment after conviction (
27–
30). In 2003, 36% of all substance abuse treatment admissions, 40% of all alcohol abuse treatment admissions, and 57% of all marijuana abuse treatment admissions were referrals from the criminal justice system (
31). Within this context, persons from racial-ethnic minority groups are more likely to commit crimes that cause them to interact with the criminal justice system (
32) and are more likely than whites to be mandated to treatment by the criminal justice system (
33).
Studies have found a negative correlation between socioeconomic status and receipt of substance abuse treatment (
18,
21). For example, individuals with less than a high school education were found to be nearly six times as likely as college graduates to receive substance abuse treatment (
18). One potential explanation is that individuals with substance use disorders may be more likely to “drift” downward (
34) into disadvantaged communities that have limited access to preventive care but greater exposure to substance abuse services offered by government agencies or correctional systems.
The Institute of Medicine (IOM) definition of racial-ethnic disparities in health care (
15) provides a conceptual framework that can be applied to the measurement of racial-ethnic disparities in receipt of substance abuse treatment and provides guidance on how to account for criminal history and socioeconomic status in the measurement of disparities. According to the IOM, disparities exclude differences that result from clinical appropriateness and need and patient preferences but include differences that result from the operation of health care systems and the legal and regulatory climate, as well as from discrimination. Differences attributable to need for services should not be considered as constituting a disparity, but differences attributable to socioeconomic status and other factors that are affected differentially by the health care, legal, or regulatory systems should be considered as contributing to the disparity. Differences that result from discrimination, whether because of biases, prejudice, or statistical discrimination, should also be considered as disparities.
Extending this definition to substance abuse treatment requires careful consideration of variables that represent clinical appropriateness and need. Adherence to the IOM definition further requires adjustment for patient preferences, although this is difficult to implement in surveys, which rarely capture fully informed preferences (
35,
36). On the other hand, the differential treatment of persons who have committed a criminal offense should be considered as a disparity under this framework, because this difference results from the operation of the legal system. In substance abuse treatment, unlike other health care services, the legal system may provide more treatment to vulnerable populations than to those without vulnerability.
To operationalize the IOM definition, we assessed racial and ethnic no disparities in treatment of individuals with substance use disorders after adjustment for level of substance use and mental health status. We also explored how criminal history and socioeconomic status reduce or contribute to these service disparities.
Methods
Data
We pooled five years of NSDUH data (2005–2009) to create a nationally representative sample (N=25,159) of 18,565 white, 2,782 black, and 3,812 Latino adults reporting illicit drug or alcohol abuse or dependence in the past year. The NSDUH provides national estimates of the prevalence of illicit drug and alcohol use and information on substance abuse treatment and sociodemographic characteristics. For the purposes of this study, individuals of any race claiming to be of Latino or Hispanic origin were identified as Latino. Other respondents were classified as black or non-Latino white on the basis of responses to the question about race. Because of small samples of Asian Americans and Native Americans, we were unable to assess disparities for these groups and did not include them in our analyses.
The first dependent variable of interest, any substance abuse treatment in the past year, indicates treatment for a substance use disorder in a hospital, rehabilitation center, community mental health center, emergency room, physician's office, and jail or prison, but not treatment in a self-help group (for example, Alcoholics Anonymous). The second dependent variable, any specialty substance abuse treatment, indicates inpatient treatment in a hospital, inpatient or outpatient treatment in a rehabilitation facility, or inpatient treatment in a mental health center.
We based our selection of variables in theoretical frameworks that explain disparities in help seeking for and utilization of behavioral health services (
37,
38). Variables are related to predisposing factors, such as demographic characteristics, enabling factors, such as income and health insurance, and need factors, such as level of need and severity of symptoms. On the basis of previous studies (
18,
21,
39), we hypothesized that lower socioeconomic status and greater need and severity would predict receipt of substance abuse treatment. We also hypothesized that respondents living in urban settings would be more likely than those in rural settings to access substance abuse treatment (
40) and that women would be less likely than men to access services for fear of losing their children and the greater stigma of substance abuse among women (
41).
To implement the IOM definition of disparities, independent variables were classified into two categories—those to be adjusted for (need) and those allowed to enter into the disparity calculation (socioeconomic status and criminal history). Need variables used were indicators of a diagnosis of a substance use disorder (categorized into illicit drug dependence, illicit drug abuse, alcohol dependence, and alcohol abuse), any functional limitation at work, self-rated health status (excellent, very good, good, fair, or poor), serious psychological distress, and major depressive episode. Serious psychological distress was measured by the K-6 (
42), a clinically validated scale measuring respondents' frequency of experiencing feelings such as nervousness, hopelessness, restlessness, and depression. Major depressive episode was assessed by
DSM-IV criteria (
43), measuring whether a respondent had five or more of nine symptoms related to depression nearly every day in a two-week period, with at least one of the symptoms being depressed mood or loss of interest or pleasure in daily activities. Age, gender, and marital status were also adjusted for because there are significant differences in need among the categories captured by each of these variables. Adjustment was also made for year to account for secular time trends in the multiple-year data set.
Variables not related to need to work criminal history, income as a percentage of the federal poverty level (<100%, 100%–124%, 125%–199%, 200%–399%, and 400%), education (less than high school, high school graduate, any college, and college graduate), employment status (employed or not), health insurance (private insurance, Medicare, Medicaid or State Children's Health Insurance Program SCHIP, other public insurance, and uninsured), and urbanicity (metropolitan statistical area population greater than 1,000,000, between 250,000 and 1,000,000, and less than 250,000). The criminal history variable used was a positive indicator of one of the following: a lifetime arrest or conviction of a crime and past-year probation or parole, supervised release, or other conditional release from prison in the past year.
Statistical analysis
In an unadjusted analysis, we assessed the significance of differences by race-ethnicity in receipt of substance abuse treatment, need, socioeconomic status and criminal history variables. In addition, we measured unadjusted rates of criminal history among only individuals who had received substance abuse treatment in the past year.
For each dependent variable, three staged logistic regression models were used to identify disparities concordant with the IOM definition, mechanisms underlying racial-ethnic differences in treatment, and correlates of treatment. To measure IOM-concordant disparities, we assessed the significance of the racial-ethnic indicator variable in a statistical model (model 1) that included only need variables and interactions between race-ethnicity and sex, age, self-reported health, and dependence on an illicit drug or alcohol. In this reduced model, unjustifiable differences between variables unrelated to need that should be counted toward the disparity according to the IOM definition (differences resulting from systems-related factors and discrimination) are captured by the race-ethnicity indicator variables.
To assess the extent to which adjustment for criminal history increased disparities, we estimated a second model that included the covariates in model 1 plus an indicator of any criminal history (model 2). Next we assessed the extent to which adjustment for socioeconomic status increased disparities, and we identified the full set of significant correlates of receipt of substance abuse treatment by estimating a third model that included model 2 covariates plus education, income, employment status, health insurance, and urbanicity (model 3). We focused on the change in black-white and Latino-white odds ratios (ORs) across these three models to assess the direction and magnitude of influence of criminal history and socioeconomic status on the association between race-ethnicity and substance abuse treatment (
44). This is similar to a traditional test of mediation (
44), except, following recommendations of Shrout and Bolger (
45) in the presence of small effect sizes and possible suppression effects, we ignored the requirement that there be a significant direct effect between the independent variable (race-ethnicity) and the outcome (receipt of substance abuse treatment).
In addition, we tested the significance of suppressor or mediating effects of six variables (any criminal history, Medicaid enrollment, being uninsured, college graduate, income greater than 400% of the federal poverty level, and being employed) in the fully specified model using the Sobel test (
46,
47). This test incorporated the association between race-ethnicity and the mechanisms of interest as well as the association between the mechanism and substance abuse treatment, conditional on other covariates. We estimated variances for model coefficients and unadjusted rates using Stata software, version 10, that accounted for survey weights, the complex sampling design, and nonresponse rates of the NSDUH.
Results
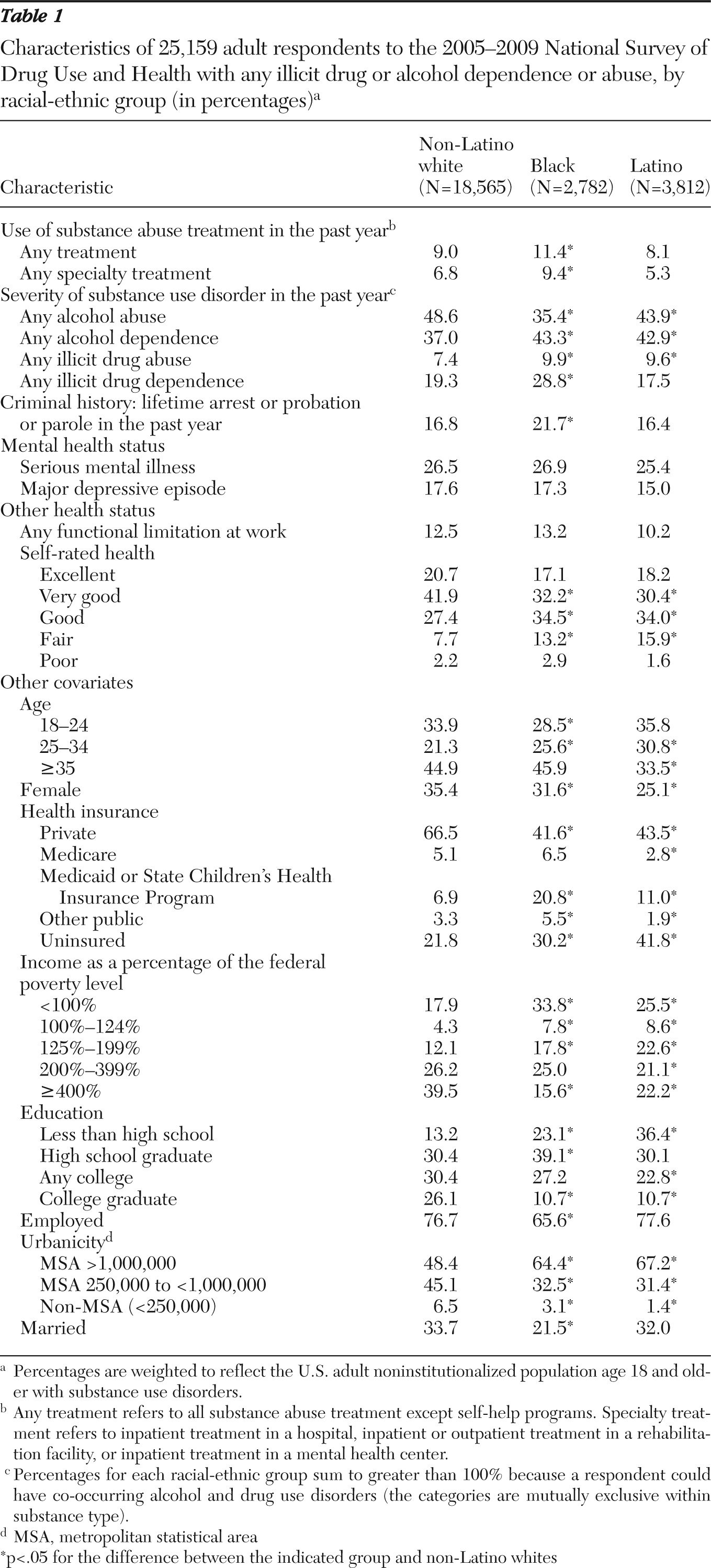
In unadjusted analyses, blacks were significantly more likely than non-Latino whites to receive any substance abuse treatment and any specialty substance abuse treatment in the past year (
Table 1). Blacks had higher rates of alcohol dependence, illicit drug abuse, and illicit drug dependence than whites but lower rates of alcohol abuse. Compared with whites, Latinos had higher rates of alcohol dependence and illicit drug abuse but lower rates of alcohol abuse. Blacks were more likely than whites to have a criminal history (22% compared with 17%).
Several other important racial-ethnic differences were found. Blacks and whites reported similar mental health status; however, as measured by percentage of the federal poverty level, blacks' socioeconomic status was lower than whites. Compared with whites, Latinos were less likely to be privately insured and more likely to be uninsured, enrolled in Medicaid, and to have lower socioeconomic status.
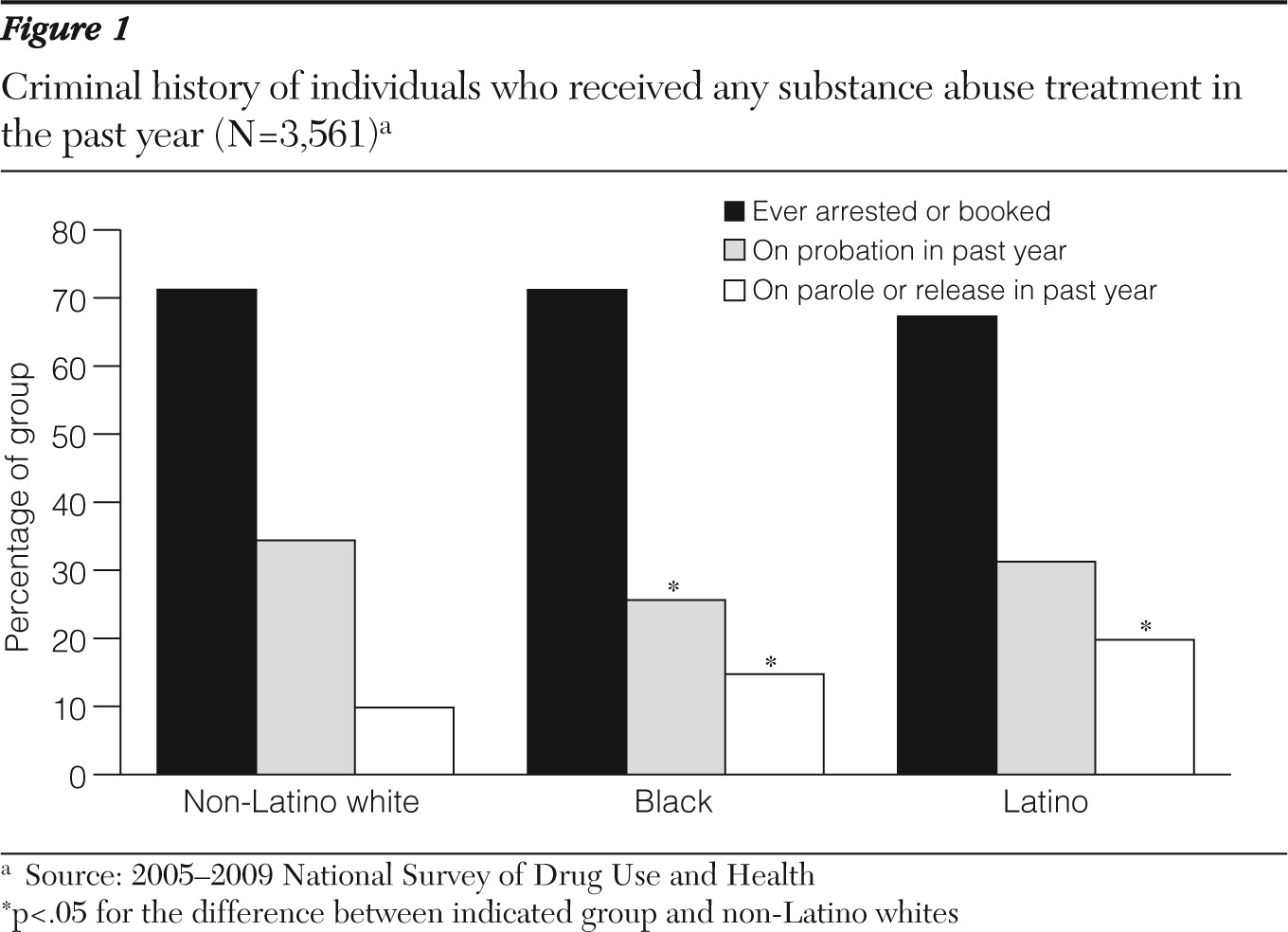
Figure 1 shows the criminal history of individuals who received any substance abuse treatment in the past year. Approximately 70% of whites, blacks, and Latinos had ever been arrested or booked for a criminal offense. Blacks were significantly less likely to be on probation in the past year and more likely to be on parole or release in the past year than whites. Latinos were more likely than whites to be on parole or supervised release in the past year.
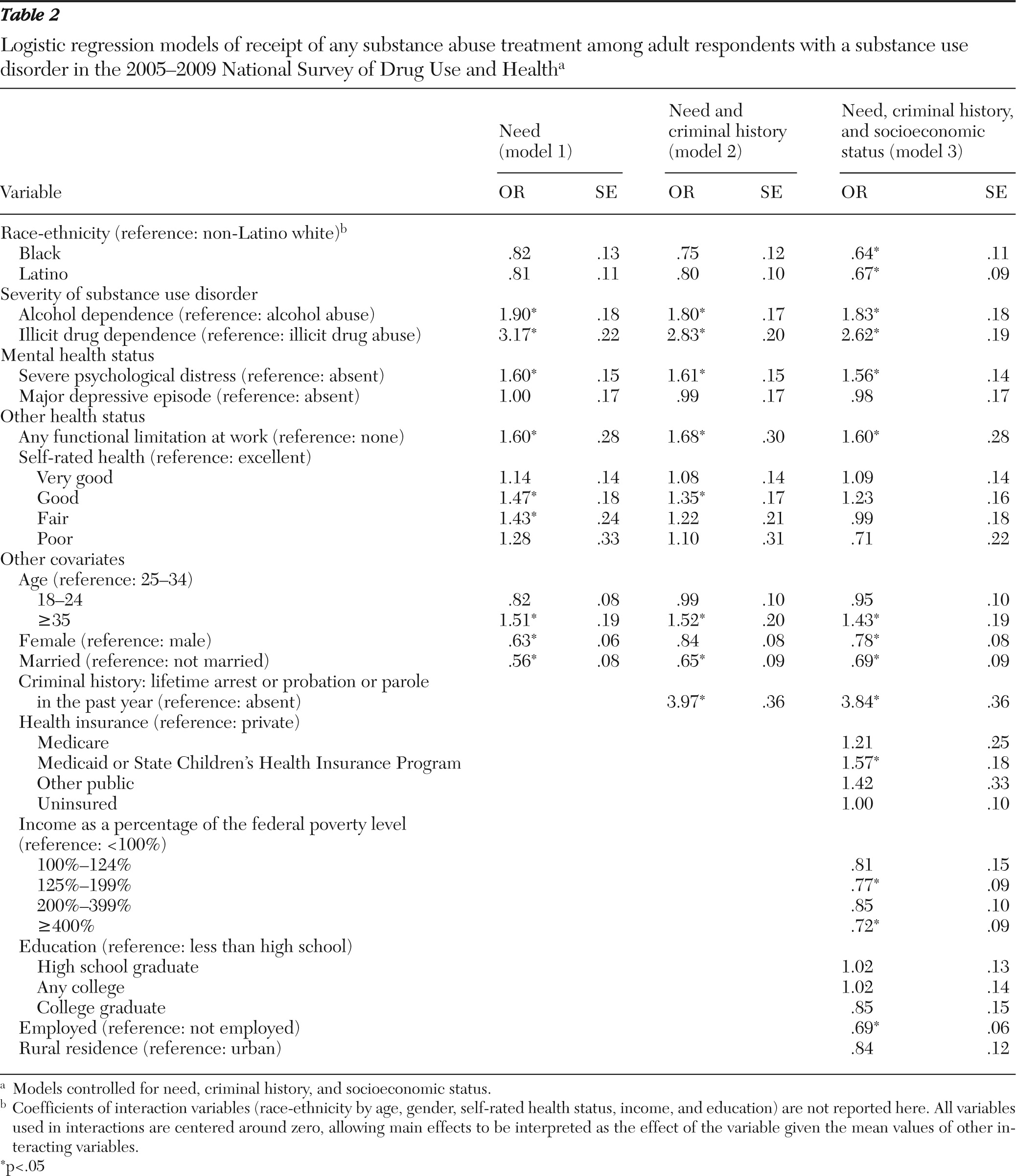
We assessed IOM-concordant racial-ethnic disparities in a regression model of any substance abuse treatment with need covariates only. No significant differences between blacks and Latinos were found (
Table 2, model 1). When the analysis adjusted for the full set of predictors of substance abuse treatment (
Table 2, model 3), black-white and Latino-white disparities were significant. Individuals with a diagnosis of dependence on alcohol or illicit drugs were more likely to receive any substance abuse treatment than those with a diagnosis of abuse of alcohol or illicit drugs. Those with severe psychological distress were more likely than those without it to receive any substance abuse treatment. Other positive predictors of treatment receipt for all groups were having any functional limitation at work, being older (age 35 or older compared with age 25 to 34), having a criminal history, and being enrolled in Medicaid. Negative predictors were having income above 400% of the federal poverty level (compared with having income below the poverty level) and being female, married, and employed.
To describe mechanisms that explained the substance abuse treatment disparities seen in fully adjusted models, we assessed the change in ORs for blacks and Latinos from model 1 to model 2 to model 3 (
Table 2). When criminal history was added to the IOM-concordant model, the OR for receiving substance abuse treatment was significantly reduced for blacks compared with whites—from .82 to .75; however, it was not significantly reduced for Latinos (from .81 to .80). In the third extended model, which also included socioeconomic status variables, the OR for blacks was reduced further to .64 compared with whites, and the OR for Latinos was reduced to .67 compared with whites; both differences represent significant racial-ethnic disparities. Sobel tests of mediation identified adjustment for racial-ethnic differences in criminal history as significantly increasing black-white differences in receipt of substance abuse treatment. Adjustment for racial-ethnic differences in being in the highest income category and enrolled in Medicaid significantly increased black-white and Latino-white disparities in receipt of substance abuse treatment. Adjustment for employment, college education, and being uninsured did not significantly change racial-ethnic disparities in receipt of treatment.
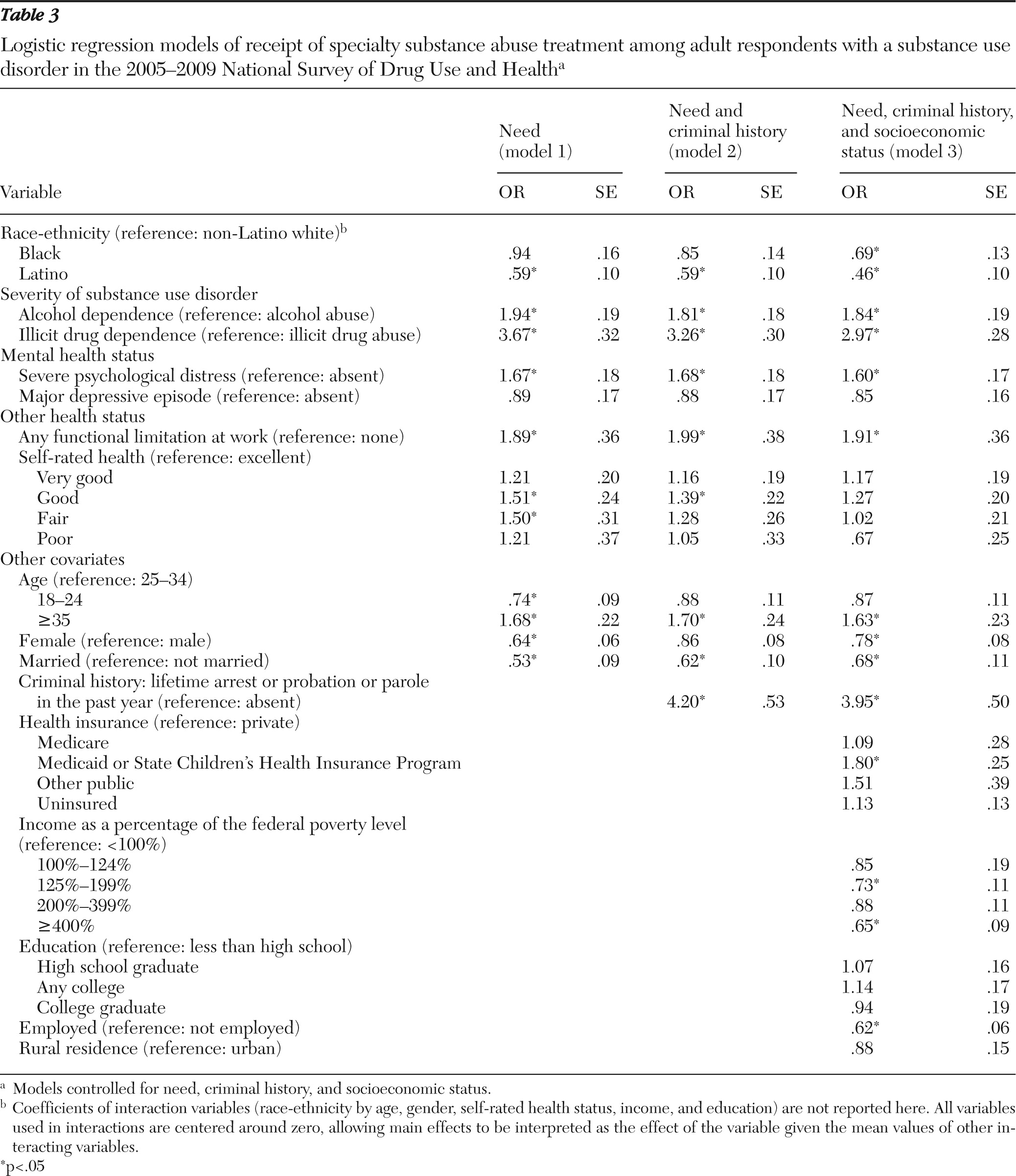
When the three staged regression models were re-estimated using receipt of any specialty substance abuse treatment— inpatient treatment in a hospital, inpatient or outpatient treatment in a rehabilitation facility, or inpatient treatment in a mental health center—we identified Latino-white disparities across all models and black-white disparities in the fully specified model (
Table 3). Significant correlates of receipt of any specialty treatment and mechanisms contributing to disparities were very similar to those identified for receipt of any substance abuse treatment. Adjustment for criminal history increased black-white disparities in receipt of specialty treatment, and adjustment for income and Medicaid enrollment increased black-white and Latino-white disparities.
Discussion
We measured black-white and Latino-white disparities in receipt of substance abuse treatment and assessed criminal history and socioeconomic status as mechanisms explaining the relationship between race-ethnicity and receipt of such treatment. As in previous studies by others (
18,
48), we did not find black-white or Latino-white disparities in receipt of any substance abuse treatment when the IOM definition of racial-ethnic disparities was used. However, black-white disparities were significant after adjustment for variables related to criminal history and socioeconomic status, and Latino-white disparities were significant after adjustment for socioeconomic status. Of particular concern was that Latino-white disparities in receipt of specialty substance abuse treatment were significant in regression models that adjusted for need, and the odds of Latinos receiving treatment were less than half those of whites in models that adjusted for criminal history and socioeconomic status.
As in other studies (
13,
18), we found that across racial-ethnic groups, a small proportion of individuals with substance use disorders (approximately 10%) sought treatment. Because of data limitations, we were not able to report on racial-ethnic disparities in the quality of the treatment, and we can only speculate that the effectiveness of treatment is markedly different for individuals who are coerced into treatment because of prison or parole requirements compared with those who seek treatment voluntarily in the traditional health care system (
49). We were not able to identify from the data set the exact legal circumstances under which treatment was received, and future research should examine this area using other data. A further limitation is that the NSDUH does not contain direct measures of severity, such as the count of
DSM-IV symptoms of dependence, scores on the Addiction Severity Index (
50), or treatment history. However, when estimating disparities, we adjusted for a number of variables associated with severity, including dependence (versus abuse), comorbid mental and general medical illness, and activity limitation. Another possible limitation is that it was necessary to pool five years of data to make meaningful comparisons between racial-ethnic groups. Even though we controlled for survey year in regression models and the stability of rates of substance use and treatment in our sample (analysis not shown), unobserved time trends over the five-year period may still have confounded our findings.
The significance of income as a mechanism underlying racial-ethnic differences in receipt of substance abuse treatment resulted from two trends in the data: individuals with lower income were more likely to use substance abuse treatment, and blacks and Latinos were more likely to be in these impoverished groups. The first of these phenomena is not representative of other areas of health care (
14,
51) and mental health care (
11,
36). Mental health treatment for individuals with substance use disorders may be less available to those in traditionally impoverished socioeconomic status groups, whereas these individuals may have greater exposure to government-sponsored substance abuse treatment services that are typically located in more disadvantaged neighborhoods. Enrollment in Medicaid also significantly changed the black-white difference in receipt of substance abuse treatment. This finding is consistent with that of a previous study that found that public insurance (blacks are more likely than whites to be insured by public programs) was a more significant predictor of substance abuse treatment than private insurance among individuals who were dependent on alcohol or drugs in the past year (
20).
The high percentage of referrals to substance abuse treatment from the criminal justice system and as a result of charges of driving under the influence (
31) and the strong correlation between involvement in the criminal justice system and receipt of substance abuse treatment found in this study suggest that more efforts at disentangling criminal activity and substance abuse is warranted. Our exploration of this area was limited because the NSDUH does not include individuals who are in jails or prisons. However, we found that approximately 70% of the noninstitutionalized population that used substance abuse treatment services in the past year had a criminal history, which is similar to findings of other studies that a majority of individuals who receive treatment were in mandated treatment programs for parole or probation requirements (
52,
53). This is understandable given that individuals in the throes of substance abuse and dependence are unlikely to voluntarily enter treatment (
54). In addition, in mandated care, outcomes related to substance abuse and legal outcomes are as good as or better than those in voluntary care (
55,
56), and treatment programs in prisons have been shown to be successful and are likely to provide treatment to many persons who would not otherwise receive it (
57–
60).
On the other hand, it is unfortunate that blacks' greater interaction with the criminal justice system (
61) is an underlying reason for their having unadjusted rates of substance abuse treatment equal to or greater than those of individuals who receive mandated treatment; such treatment is more likely to be perceived as coercive and dehumanizing (
62). This finding suggests the need to identify clinical and policy interventions and treatment programs (for example, anonymous workplace treatment services and employer treatment mandates for persons who disregard employee drug and alcohol policies) that increase motivation for voluntarily accessing treatment before dependence reaches the point at which an individual is likely to become involved with the criminal justice system.
Conclusions
Significant black-white and Latino-white disparities in both receipt of any substance abuse treatment and of specialty substance abuse treatment were identified only after controlling for blacks' higher rates of criminal history and both groups' lower socioeconomic status compared with whites. The intersection of race-ethnicity, socioeconomic status, and criminal history is particularly important to understanding substance abuse treatment disparities and should not be overlooked in future studies.
Acknowledgments and disclosures
This research was supported by grant P60-MD002261 from the National Institute on Minority Health and Health Disparities. The authors acknowledge helpful comments and suggestions from Philip J. Cook, Ph.D., and Thomas G. McGuire, Ph.D.
The authors report no competing interests.