The President's New Freedom Commission on Mental Health (
1) recommended that mental health systems transform to become more patient centered and recovery oriented. The commission defined recovery as “the process in which people are able to live, work, learn, and participate fully in their communities.” As part of the recovery model, the commission envisioned a transformed system in which people with serious mental illness could work if they wanted to, receive vocational rehabilitation support, and seek employment without fear of prejudice or discrimination. The commission identified supported employment, an evidence-based practice for helping clients obtain community-based competitive employment, as a means to achieve these ends (
2,
3).
Supported employment varies from traditional Department of Veterans Affairs (VA) compensated work therapy (CWT) vocational rehabilitation programs in which patients are hired by the VA for noncompetitive work. Patients in conventional CWT can be placed in sheltered workshops supervised by vocational rehabilitation staff or in transitional work in which the VA secures work contracts and then places clients in available positions while serving as an intermediary between the employer and the patient (
4,
5). Instead, supported employment's principles include clients' self-determination of their eligibility to work in a competitive setting, a rapid search for employment fitting a client's preferences, integration between supported employment and mental health teams, ongoing and time-unlimited support from the vocational and treatment teams, and no exclusion from participating in supported employment services (
6,
7). Guidelines, recommendations, and toolkits for implementing and sustaining evidence-based practices (
8,
9) for individuals with serious mental illness, such as supported employment (
3), are well established. In randomized studies, adherence to supported employment principles was associated with higher employment rates compared with other vocational programs (
10–
12).
Adopting, implementing, and ultimately sustaining a new model of vocational rehabilitation and recovery can be impeded by a number of individual and organizational factors. For example, some believe that individuals with serious mental illness cannot live productive lives, are dangerous, and can perform only low-level jobs (
13). Programs to help people with serious mental illness can be stigmatizing to participants when employees hold onto these negative perceptions rather than working with accurate and specific knowledge of program and client activities (
14,
15). Providers or leaders in mental health organizations may resist recovery efforts (
16) for reasons that include paternalistic needs to protect patients whom they view as disabled, (
17,
18), misunderstandings about recovery, doubts about whether patients can be successful, protection of limited financial and human resources, challenges to the status quo of management and treatment, and potential provider liability (
19).
In 2004 the VA began to disseminate and implement supported employment nationally, with additional resources at 21 selected sites (
5,
20), which included funding for staff and resources, on-site technical assistance, and biannual review of program fidelity to supported employment principles. Concurrently, our research team conducted interviews with VA employees to better understand the implementation process. Our research focused on identifying successes and challenges that arose out of introducing an innovation that required organizational transformation to be successful. Specifically, supported employment is a recovery program that is a departure from traditional vocational services for individuals with serious mental illness (
21).
We used the organizational transformation model (
22) as a framework through which to examine how the supported employment model was introduced and implemented at the sites. This model identifies five key drivers of change that interact to help organizations develop sustained, organizationwide patient care improvements: impetus to change, leadership commitment, improvement initiatives, alignment of organizational goals and resources, and integration across intraorganizational boundaries. Greater evidence of these drivers in health care systems is associated with better transformation (
22). In this study we focused on perceived barriers to supported employment implementation as described by VA medical center (VAMC) employees and described them in the context of the organizational transformation model by identifying organizational characteristics that existed or changed during implementation.
Methods
Site and respondent selection
In February 2006 the national implementation coordinating center selected six sites to be interviewed among the 21 VAMCs that were receiving additional resources. Two sites each were on the East and West coasts, one was in the South, and one was in the Midwest. At the time of selection, two sites each were among the top and bottom performers on a biannual review of fidelity to supported employment principles, and two were the first and last to begin implementation. The lead interviewers were blind to site status and selection criteria during the study's data collection and analysis phases. Interviews for year 1 began in July 2006 and were repeated approximately one year later.
We targeted interviews to VAMC senior and middle leadership, mental health leaders and clinicians, and supported employment program staff. We e-mailed potential interviewees an invitation to participate and scheduled individual interviews after recipients agreed. After complete description of the study, informed consent was obtained from all participants. Institutional review boards from all participating sites approved this research. In year 1, a total of 74 of 87 (85%) employees who were contacted participated; in year 2, 63 of 104 (61%) participated. Overall, there were 84 unique respondents. Across both years, proportionally more supported employment staff who were invited to be interviewed (93%) participated compared with mental health employees (71%) and VAMC leadership (69%) (χ2=6.63, df=2, p<.04; N=110). We found this difference in response to be acceptable given the study's focus on supported employment program implementation.
Data collection
We used a semistructured interview guide that had an organizational focus on development of the supported employment program and facilitators and barriers to implementation. [The guide is available in an online supplement at
ps.psychiatryonline.org.] The second author primarily conducted the interviews, and the first author took notes and asked follow-up questions as needed. With participant permission, all interviews were audio-recorded and transcribed.
Data analysis
Interview transcripts were analyzed by using NVivo 2.0 and Microsoft Word XP software programs that allow for qualitative data analysis and categorization. Both a priori (deductive) (
23) and data-driven (inductive) (
24)approaches to thematic analysis (
25) were employed. Identification of coding categories was guided primarily by a focus on organizational transformation and the associated successes of and barriers to supported employment program implementation. Additional themes that emerged from the data were related to “paternalism” and “being uninformed.” The first two authors independently coded ten transcripts and cross-checked their results to ensure consistency. Discussion of discrepancies led to consensus. The first two authors then independently coded the remaining transcripts before discussing their findings. Transcripts were rereviewed to ensure that themes were fully captured.
Results
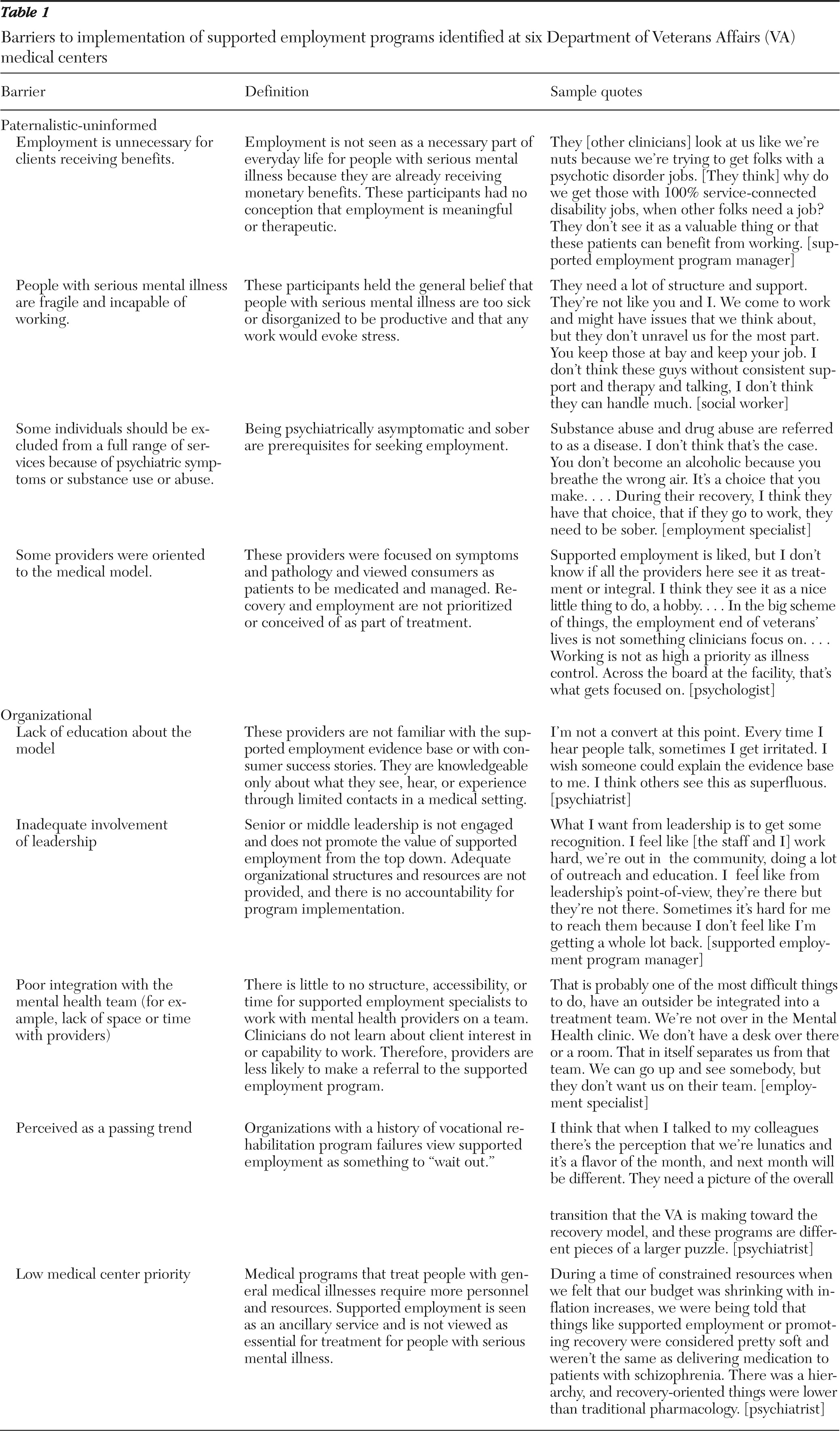
There was strong agreement in identifying organizational strengths, changes, barriers, and facilitators during implementation. The first two authors developed tables that reflected the data's themes and associated evidence by site before determining that there were nine relevant barrier-related categories. The nine barriers to supported employment implementation were classified into paternalistic-uninformed and organizational challenges (
Table 1).
Paternalistic-uninformed
Employment is unnecessary for clients receiving benefits.
Some interviewees reported that staff did not understand why clients with serious mental illness would need additional income and instead believed that employment services should be aimed at those deemed more capable of work and who were not already receiving benefits. Unaware that clients of the supported employment program could receive benefits when working, some providers were hesitant to make referrals for fear that patients would lose necessary financial support. Consultation with benefits specialists was helpful for educating providers.
Individuals with serious mental illness are fragile and incapable of working.
There were mixed beliefs about clients' abilities to function in a work setting, and therefore the foundation of the supported employment model and its goals were sometimes questioned. Many sites struggled with mental health providers' refusal to refer patients to the supported employment program. Because providers work with patients in time-limited office visits, some providers based their judgment of patients' ability to work on limited knowledge. Some primary care and mental health providers were protective of their patients and did not believe they were ready to participate in vocational services.
Marketing the program to providers and discussing success stories helped counter negative beliefs. Focusing on clients' behaviors, abilities, and functional limitations rather than on pathology was productive when talking with providers or potential employers.
Some individuals should be excluded from a full range of services because of psychiatric symptoms or substance use or abuse.
A core supported employment principle is that clients are eligible for program services regardless of active substance use or abuse or psychiatric symptoms. Some clinicians and employment specialists were doubtful of clients' ability to work when they were actively symptomatic; there was more compassion toward psychiatric illness than toward substance use and abuse. Some clinicians saw substance abuse as a barrier to referring a client to supported employment and would not make a referral until the client completed a substance abuse treatment program and demonstrated sobriety.
Employment specialists voiced “greater-good” reasons to scale back job development efforts when clients were actively abusing substances. Concerns were related to safety and liability and protection of the reputation of the supported employment program. Providing full supported employment services was the expectation; however, informally and at their discretion, some employment specialists reduced job development efforts for clients who were actively symptomatic or abusing substances.
Some providers were oriented to the medical model.
Interviewees noted that providers using 15-minute office visits typically focused on medication and symptom management; employment was not considered part of the treatment plan. At one site, employment specialists met clients in waiting rooms and offered them brochures about supported employment. Clients took the brochures to their psychiatrist, so that it was clear that interest was coming from them.
Organizational barriers
Lack of education about the model.
One barrier to implementation, which reflected weak organizational alignment, was an organizationwide lack of knowledge about the supported employment model. Middle- and senior leadership at some sites were proactive and effective in introducing the supported employment program to mental health treatment teams, either by itself or in the context of larger recovery efforts. However, implementation sometimes preceded centerwide informational sessions about supported employment and the recovery model, thereby giving the program limited visibility or credibility in its early stages. At some sites, when clinicians were not given follow-up educational booster sessions about the program, they sometimes forgot its principles. At one site there was no organizationwide education, and the piecemeal education efforts by supported employment staff resulted in clinicians' continued adherence to traditional practices (for example, not referring patients for vocational rehabilitation if patients were not sober). Some believed that supported employment was a form of case management, and others did not understand the recovery model. Without knowledge of the evidence base or the spread of success stories, clinicians did not see the benefits of making referrals to the program.
Inadequate involvement of leadership.
The directive to implement supported employment services came from the highest levels of national VA leadership. However, the way it was implemented locally varied. Some senior leadership focused on other priorities and relied on middle- and lower-level leaders to manage and promote the program, which reflected the limited engagement of senior leadership. By year 2, five of the six sites reported moderate to strong support from local senior leadership, but one site continued to struggle. The supported employment manager did not have previous program training. Feeling that there was minimal guidance for program start-up, he had to self-learn its principles and consult with other supported employment programs. The manager noted that leadership was aware of the program, but the manager wanted leaders to be involved more in obtaining equipment for program staff and clients and in facilitating integration and colocation of the program with the mental health service. Senior and middle leadership at this VAMC were in transition during supported employment implementation, which likely impeded the program's ability to gain attention and become fully integrated into operations.
Two sites had very strong supported employment managers and mental health leaders who embraced recovery and supported employment principles and encouraged team efforts. Some leaders had already been practicing elements of the supported employment model before it was formally implemented locally. One psychologist described how he had become “infected” with the recovery model and realized that the pessimistic messages that he and other mental health providers were giving patients previously were wrong. In turn, he began conducting his own presentations about recovery, and he proudly stated, “I got infected with the religion of recovery before I saw successes. … I infected my boss and staff, and I want to infect the layers in between.”
Poor integration with the mental health team.
Many supported employment programs had difficulty developing linkages with providers during initial implementation. Poor integration was attributed to such logistical issues as restricted physical space for team meetings, high caseloads, limited time for meetings and informal discussion, and confusion among clinicians and employment specialists about roles. For some mental health providers, without the structure and processes of integration, it was difficult to understand the value of the supported employment program. This sometimes led to tension when employment specialists wanted to be involved in discussions of patient treatment plans.
Perceived as a passing trend.
Noting the history of other failed vocational programs within local VAMCs, interviewees reported that skepticism about the viability of the supported employment program decreased buy-in. Some employees believed that enthusiasm for the program would eventually decline, and they needed to be certain of VA Central Office's commitment to its continued funding.
Low medical center priority.
On the basis of competing priorities to allocate resources to care related to more general medical conditions, some interviewees were concerned about beliefs that supported employment was not integral to treatment. Several noted that budget restrictions usually resulted in prioritization of medically oriented services.
Discussion
On the basis of perspectives from frontline staff to senior leadership, we identified nine barriers to supported employment implementation related to paternalism or being uninformed and organizational challenges and considered them in the context of organizational transformation. Regardless of previous organizational experience with vocational programs or degree of preparation for implementing recovery-based programs, individuals at each of the sites expressed or encountered similar negative beliefs about or experiences with implementing the supported employment program during the early phases.
Paternalistic-uninformed
Barriers classified as paternalistic-uninformed tended to be nonsystemic, and interventions to overcome these barriers could have included targeted education during early implementation. Some sites successfully countered such issues by having counselors discuss the impact of earned income on existing benefits and having credible stakeholders continually spread employment success stories that refuted perceptions of patient disability. Some providers who were trained in the medical model, which focuses on patient pathology and limitations rather than on personal strengths (
18,
26), considered themselves “converts” to the supported employment model after seeing positive results. Others' resistance to fully accepting it may have been a natural consequence of introducing a framework that deviated from traditional care. Finally, better team oversight may have prevented limiting supported employment services to clients who were actively drinking or using illegal substances. Some employment specialists noted that consequences for using and abusing substances (for example, getting fired) had served as valuable learning experiences and motivators for clients to regulate or discontinue their use. The barriers classified as paternalistic-uninformed represent the need for supported employment and mental health team integration and engagement in education and problem solving.
Organizational barriers and organizational transformation
The organizational barriers identified in this study each touched on an aspect of the organizational transformation model, but deficits in leadership support and integration across teams were the most pronounced. All study sites were mandated to implement supported employment (key driver: impetus to transform), but the way in which this was actualized varied across VAMCs. Having knowledgeable, engaged, and committed leadership at all levels (
27) was perceived to be important to successful implementation. At the level of the supported employment team, these leaders practiced the ideals of the program, which included respecting the value and ability of clients to be self-determined and gainfully employed, hiring employment specialists who were educated both formally and on the job, facilitating team cohesion, and employing effective hands-on management (
28). Middle- and senior-level leaders demonstrated support by introducing supported employment in the context of other recovery programs (key driver: alignment) and educating other providers about its successes. Engaging leadership early and relying on leadership with strong experience were strong contributors to successful program implementation. A top-down approach that reinforced the supported employment initiative and ensured that structures were in place to promote the integration of the supported employment team with other programs (
4,
29) facilitated education and marketing of the program. Such practices served to bring more visibility to supported employment, and these efforts may have helped to protect against or change negative and misinformed perceptions of the program and its clients (
8,
30,
31).
The site that had foundered most in its implementation did not have a strong history of vocational rehabilitation or leadership support. The program lacked integration and was physically and conceptually isolated from the mental health teams; it also underwent staff turnover and experienced middle- and senior-leadership changes in the VAMC. In addition, the program manager was new to the principles of supported employment, team members were more experienced in traditional CWT programs, and other mental health providers did not understand the program's evidence base. Because of this “perfect storm” of challenges, the program may have benefited from intensive intervention and education at multiple levels.
Limitations
Although respondents ranging from leadership to frontline staff reported experiencing or hearing negative attitudes about the supported employment program or the seriously mentally ill population, the semistructured interviews did not specifically include any questions pertaining to paternalism or being uninformed. We identified these themes during the qualitative analysis. However, we believe that the information we heard was reliable and substantial and that any targeted questions would have yielded similar—and perhaps more elaborate—information. Because our research model did not include data collection from clients of supported employment programs, we do not know whether our findings were associated with clients' perceptions of bias or with lower-quality services. Future studies would benefit from concurrent interviews with supported employment staff and their clients.
Conclusions
Nonsystemic paternalistic-uninformed concerns about the ability of individuals with serious mental illness to be gainfully employed and a lack of structure and leadership to educate providers and facilitate team integration are common challenges to transforming organizations during implementation of supported employment. During implementation, organizations would likely benefit from leadership buy-in and from promotion of these programs and education of mental health teams by knowledgeable and influential stakeholders. Such education should address negative beliefs, focus on the evidence base, and continuously reinforce the technical aspects and merits of supported employment.
Acknowledgments and disclosures
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Health Services Research and Development grant MNT 05-098. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
The authors report no competing interests.