There is less information about general medical disorders among youths with psychiatric problems than among adults with psychiatric problems, but studies suggest that physical problems are common (
1,
2). The most prevalent chronic condition among youths is excessive body weight (
3), termed overweight or obesity, depending on the degree of overweight and choice of terminology. It also is well known that numerous medications to treat psychiatric problems among youths contribute to weight gain and obesity, which are associated with the onset of diabetes, dyslipedemia, hypertension, and metabolic syndrome (
4,
5).
Because of concerns about the health status of youths with mental disorders, the New York State Office of Mental Health (OMH) developed a health and wellness monitoring and promotion program for a large group of youths with psychiatric disorders treated in 48 outpatient and day treatment settings operated by OMH.
OMH operates six children's psychiatric centers devoted entirely to the treatment of youths and eight psychiatric centers that serve both youths and adults. The 13 centers with both inpatient and outpatient (clinic or day treatment) programs for youths were selected to participate in the wellness program. Approximately 2,000 youths are treated at the outpatient clinics and day-treatment settings at a given time.
Each of the 13 sites designated a site coordinator to oversee the program. The site coordinator worked under the direction of the executive director and clinical (medical) director of the facility to implement the program. The OMH Division of Children and Family Services provided training and orientation to executive directors, clinical directors, and site coordinators through discussions at leadership meetings, written protocols, and conference calls. A Health Indicators Record Form was created to record the wellness indicators. This information was entered into the OMH Mental Health Automated Record System (MHARS), a digital electronic medical record. All youths were screened at the beginning of an episode of service at these outpatient settings and quarterly thereafter if they remained in care.
This article describes implementation of the monitoring program during its first year and screenings results for youths in care at the last time point, ten months after the program began. We hypothesized that the population of youths treated in these outpatient psychiatric settings differ from their peers in the general population on all wellness indicators evaluated. We expected to find a higher BMI percentile, a lower activity level, and more cigarette smoking and alcohol and drug use among youths in this population compared with population norms.
Methods
Health screening indicators
All youths were screened for BMI percentile and activity level. Youths ages 13 to 22 were also screened for cigarette smoking and alcohol and drug use. Screening was conducted beginning in July 2009 and continued on a quarterly basis for youths who remained in care through April 2010.
BMI percentile was chosen because of the high prevalence of obesity among youths in our society (
3,
9,
10), its deleterious effects on health (
11), and its association with the use of certain psychotropic medications, notably, but not exclusively, atypical antipsychotic medications (
4). Height and weight were obtained by clinic personnel and converted to BMI percentiles electronically by using a standard conversion formula. Consistent with Centers for Disease Control (CDC) guidelines (
11), youths with BMI percentiles at or above the 85th percentile for age were considered overweight, and those with BMI percentiles at or above the 95th percentile were considered obese. In this article, the term overweight is used more broadly to encompass the obese category so that all youths at or above the 85th percentile for BMI are considered to be overweight.
Activity level was chosen as a screening indicator because of its association with obesity and its importance in overall growth and development (
12,
13). A minimum of 60 minutes per day of activity was chosen as the screening criterion on the basis of recommendations for children and adolescents contained in the
2008 Physical Activity Guidelines for Americans (
14). Information about activity level was provided by parents or guardians and by youths' self-reports, sometimes with the assistance of clinic staff. The Health Indicators Record Form provided examples of various activities that were suitable for inclusion as an activity under CDC guidelines (
14).
Cigarette smoking was chosen because of its known deleterious effects on health and the association of early tobacco use with progression to use of other substances of abuse (
15). To determine smoking behavior, youths were asked if they had had one or more puffs of a cigarette in the past month, a question similar to an item on the Youth Risk Behavior Survey that asks about the use of cigarettes on one or more days in the past 30 days (
16). DiFranza and others (
17) found that within the first few days of use, susceptible youths may lose autonomy over tobacco use. In addition to youths' self-report, sometimes assisted by clinic staff, information about cigarette smoking was also obtained from parents and guardians.
Alcohol and drug use was chosen because of its association with adverse health outcomes (
8), the recognized comorbidity of substance use disorders and mental disorders (
18), and the increased likelihood of conduct disorder and illicit social behaviors among youths with substance use disorders. Alcohol and drug use were screened at baseline and at one year with the CRAFFT, an instrument developed for this purpose by the Center for Adolescent Substance Abuse Research at Children's Hospital, Boston (
19). The six-item CRAFFT has been found to be a reliable and valid instrument for screening youths attending a number of adolescent clinics (
20,
21). Respondents who answer yes to two or more questions or who report having driven while high on drugs or alcohol or having been a passenger in a car driven by someone who was high are considered at high risk for alcohol and other drug use.
At quarterly intervals between CRAFFT assessments, adolescents were screened with the single question, “Have you used alcohol or street drugs or any substance in the last month to make yourself feel better or to get high?” They were also asked about cigarette use. The cigarette smoking and alcohol and drug use questions were asked only of youths ages 13 and older, in part because the CRAFFT had been developed for use with adolescents.
Data retrieval and analysis
Data were extracted from the MHARS and compiled quarterly according to psychiatric facility and program type (clinic or day treatment). Demographic data related to age and gender of the youths screened were also extracted. Reports of these descriptive data were shared with site coordinators, executive directors, and clinical directors approximately every two or three months during conference calls that included the first author and other OMH Division of Children and Family Services personnel. Problems in program implementation, data retrieval, data entry, and missing data were discussed and remediated through this process.
Statistical comparisons of the four health risk indicators by demographic data (age and gender) and program type (clinic or day treatment) were done by using chi square analysis. Strength of association between the screening indicators was determined by using the chi square test with Cramer's statistic.
Six separate multivariable logistic regression models were created to examine the associations between demographic factors and health risk status. Health risk indicators were used as dependent variables and were constructed as follows: activity level of at least 60 minutes daily (yes or no), obesity (95th percentile or greater versus less than 95% percentile for BMI), smoking status (yes or no), substance use (yes or no), and positive CRAFFT score (answers of yes to two or more of the six items).
Independent variables in each model included the demographic factors of gender (male or female) and age group (13 and older or 12 and younger), program setting (clinic or day treatment), and the interaction term of age and gender. Age was constructed as a continuous independent variable for the smoking, substance use, and CRAFFT models because these measures were obtained only for youths aged 13 and older. Models controlled for specific health risk indicators where associations between the indicator and outcome of interest were statistically significant as determined by using chi square tests as detailed above. For example, the health screening indicator of smoking (yes or no) was controlled as an independent variable in both the models predicting substance use and CRAFFT risk for alcohol and drug use. Similarly, activity was included as an independent variable in the model predicting obesity and overweight. All models were tested at the 95% significance level.
Results
The rates of measurement of the four indicators varied among the sites, but by and large, they improved and stabilized over time. By the last time point, average retrieval rates were 84% for activity level, 86% for BMI, 85% for smoking, and 84% for alcohol and drug use. [A table summarizing statewide screening rates from July 2009 to April 2010 is available in an online appendix to this report at
ps.psychiatryonline.org.]
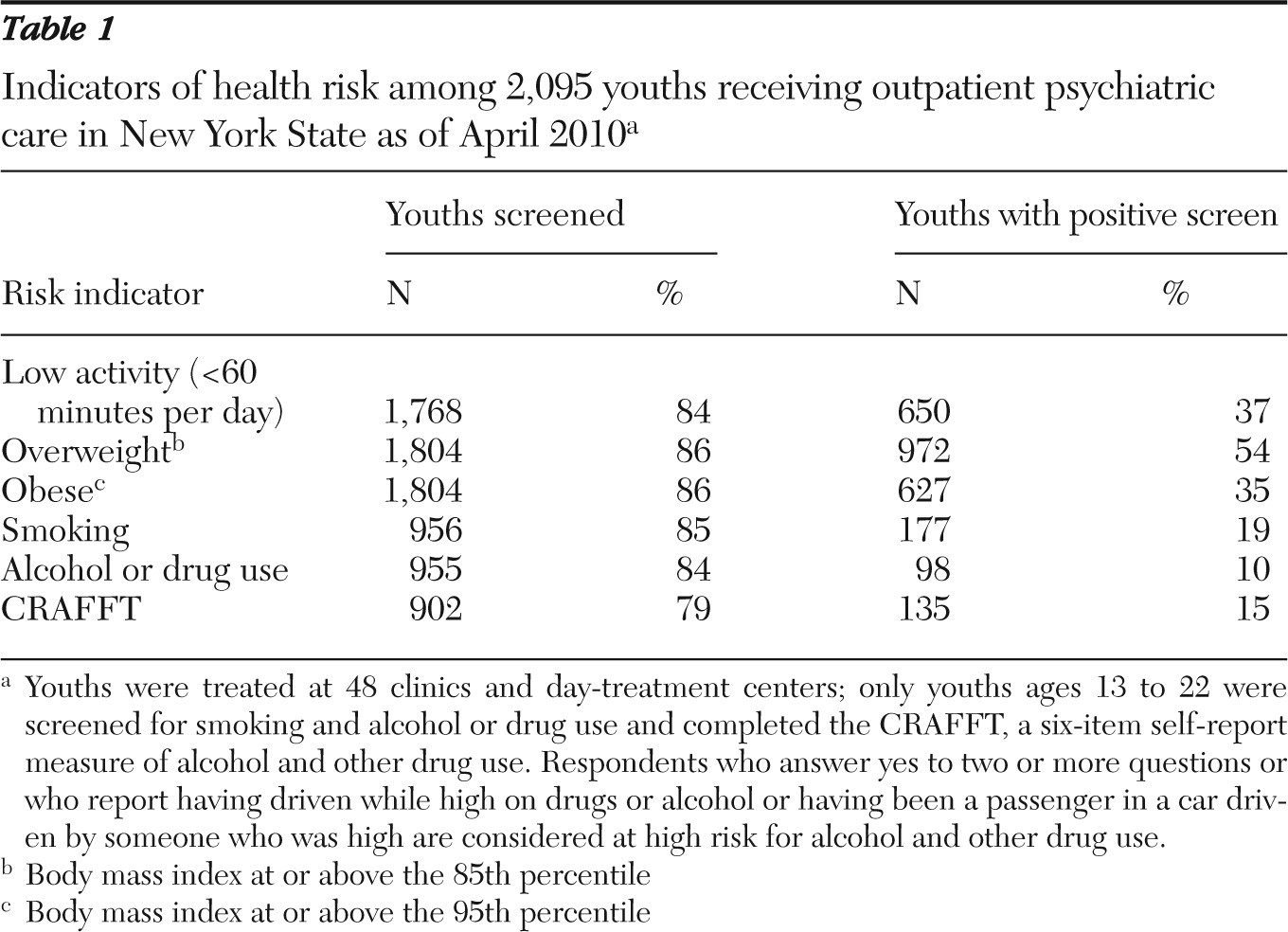
A total of 2,095 youths remained in care at the last time point; 1,377 (66%) were male and 718 (34%) were female. A total of 1,136 (54%) were adolescents 13 to 21 years of age, and 959 (46%) were 12 and younger. At the last time point, 54% of youths screened were in the overweight category; 35% were in the obese category, 37% screened positive for low activity level, 19% screened positive for cigarette smoking, 15% screened positive on the CRAFFT for alcohol or drug use, and 10% screened positive on the alcohol and drug use question (
Table 1).
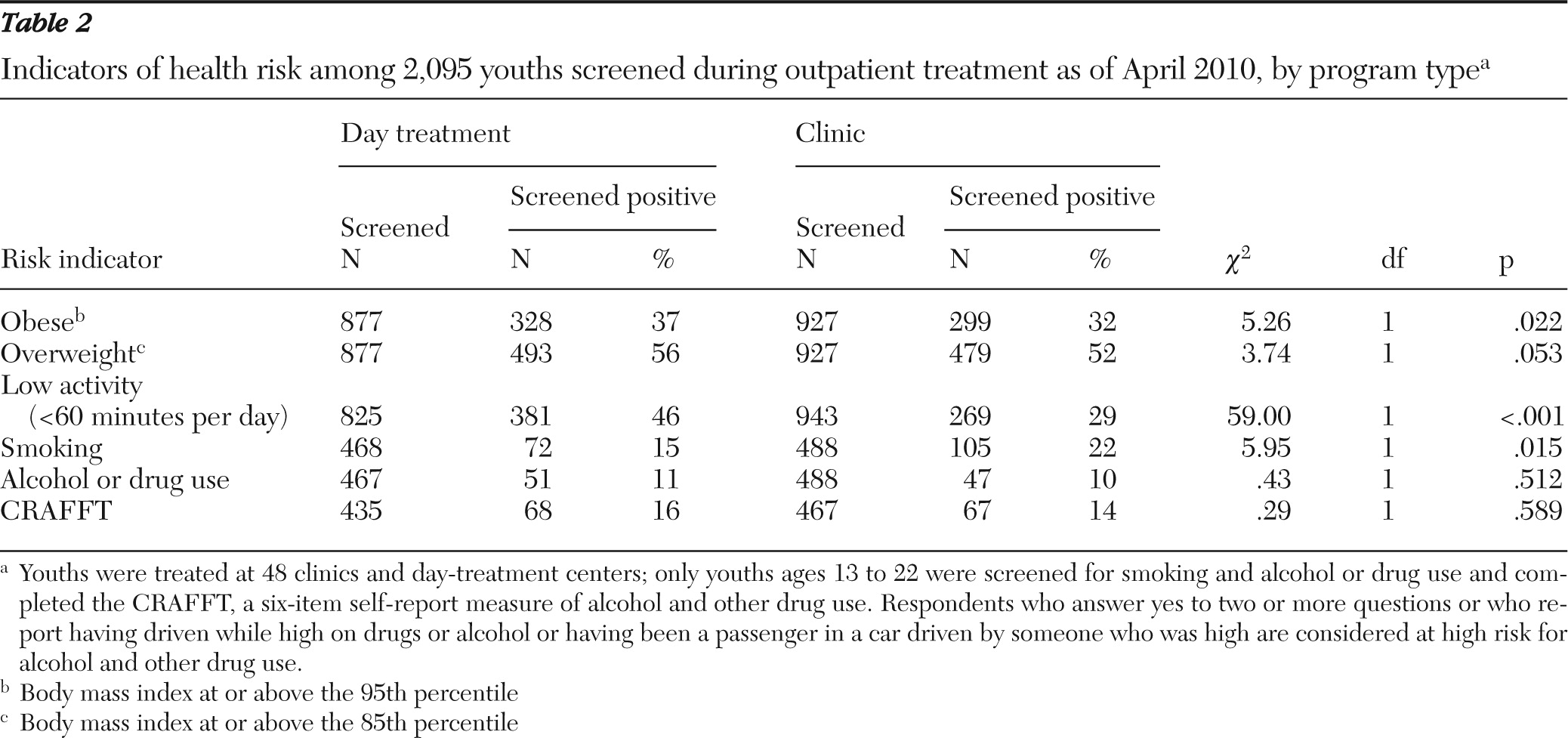
The associations between each of the screening indicators and program type or demographic data (age and gender) were examined by using chi square tests. The parameters of obese or overweight, activity level, and smoking (among adolescents) were significantly different depending on the treatment site. Compared with youths treated at clinics, youths served in day-treatment programs were more likely to have low activity levels (
χ2=59, df=1, p<.001) and increased rates of obesity (
χ2=5.26, df=1, p=.022), were more likely to be overweight (
χ2=3.74, df=1, p=.053), and were less likely to smoke (
χ2=5.95, df=1, p=.015) (
Table 2).
In terms of comparison by gender, boys were less likely than girls to be overweight (
χ2=12.07, df=1, p<.001) and to have low activity levels (
χ2=68.78, df=1, p<.001). Compared with adolescents, preadolescents were more active (
χ2=85.02, df=1, p<.001) and had less risk of being overweight (
χ2=13.56, df=1, p<.001) or obese (
χ2=5.22, df=1, p=.022) (
Table 3).
Post hoc comparisons of the strength of chi square associations between screening indicators by adding Cramér's statistic showed strong associations between particular risk indicators, particularly for overweight or obesity and low activity (v=.23), smoking and substance use (v=.42), and CRAFFT results and substance use (v=.44).
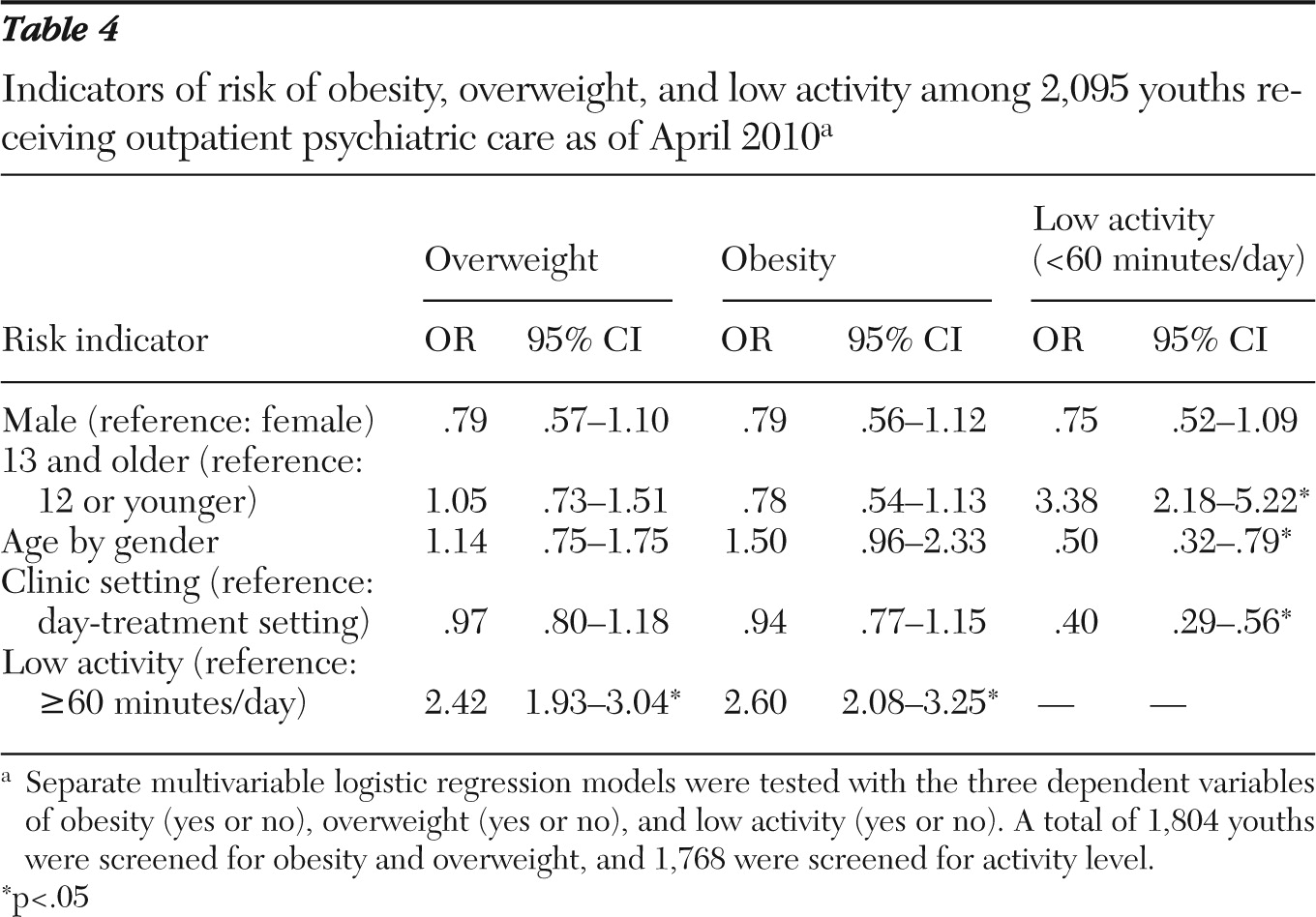
Table 4 displays the results of multivariable logistic regression models predicting obesity, overweight, and low activity. The only significant predictor in both the obesity (OR=2.60, p<.001) and overweight (OR=2.42, p<.001) models was low activity level. Low activity was predicted by older age (OR=3.38, p<.001), by the interaction of age and gender (OR=.50, p<.003), and by program setting (OR=.40, p<.001). The interaction of age group and gender was less robust for boys than girls. Older boys were 1.68 times more likely to display low activity compared to younger boys, and older girls were 3.38 times more likely to display low activity compared to younger girls.
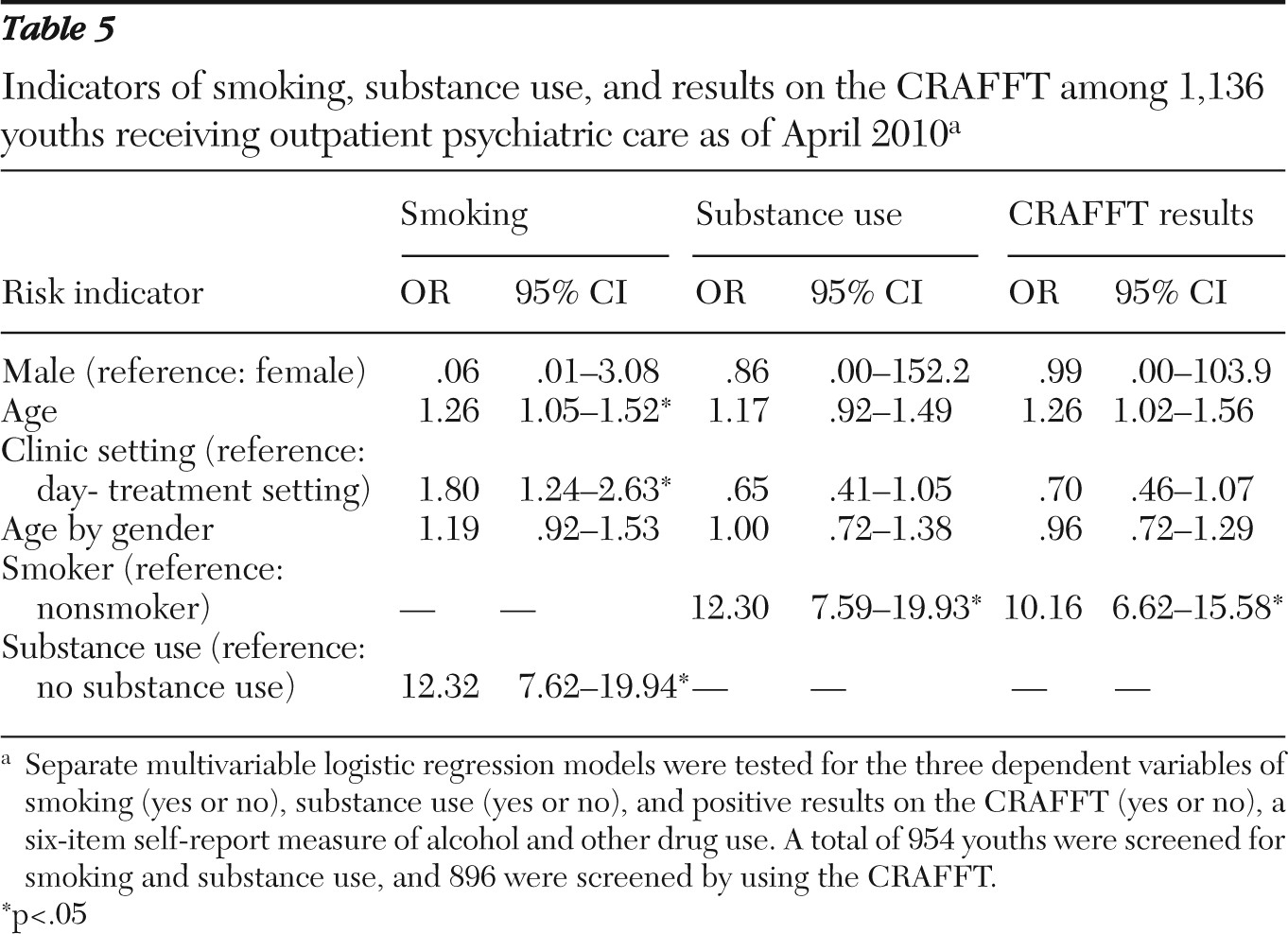
Table 5 displays the results of multivariable logistic regression models predicting smoking, substance use, and positive CRAFFT screen. Smoking was predicted by substance use (OR=12.32, p<.05), age (OR=1.26, p<.05, for each year increase in age), and program type (OR=1.80, p<.05). In the substance use model, smoking was the only predictor (OR=12.30, p<.05). Positive CRAFFT score was predicted by smoking status (OR=10.16, p<.05) and age (OR=1.26, p<.05, for each year increase in age).
Discussion
Youths in outpatient mental health programs have extremely high rates of overweight and obesity. Nearly 54% of youths in this study were in the overweight category, and nearly 35% were in the obese category. These figures were consistent with our hypotheses and were much higher than those found in the general population (
9,
10). The findings were more striking for girls and for those in the older (adolescent) age group.
For comparison purposes, a study by Ogden and others (
9,
10) of data from the National Health and Nutrition Examination Survey (NHANES) 2007–2008 found that 32% of youths aged two to 19 years were at or above the 85th percentile for BMI among youths their age and that 17% of youths were at or above the 95th percentile for their age. Among youths aged six to 11 years, 36% were at or above the 85th percentile for BMI for their age and 20% were at or above the 95th percentile. Among youths aged 12 to 19 years, 34% were at or above the 85th percentile for age, and 18% were at or above the 95th percentile for age.
The NHANES data (
9) allow a more fine-grained understanding of obesity among youths than in this study by providing data on the basis of age, sex, and race-ethnicity. Among boys aged six to 11 years, 20.5% of non-Hispanic whites, 17.7% of non-Hispanic blacks, 28.3% of Hispanics, and 27.1% of Mexican Americans were obese. Among girls aged six to 11 years, 17.4% of non-Hispanic whites, 21.1% of non-Hispanic blacks, 21.9% of Hispanics, and 22.3% of Mexican Americans were obese. Among boys aged 12 to 19 years, 16.7% of non-Hispanic whites, 19.8% of non-Hispanic blacks, 25.5% of Hispanics, and 26.8% of Mexican Americans were obese. Among girls aged 12 to 19 years, 14.5% of non-Hispanic whites, 29.2% of non-Hispanic blacks, 17.5% of Hispanics, and 17.4% of Mexican Americans were obese.
These data suggest that rates of obesity tend to be higher among youths from minority groups. Therefore, although higher than we had expected, the prevalence of overweight and obesity in the population we studied, which had high rates of youths from minority groups (
22), may not have been as striking as initially imagined.
Physical activity rates were found to be partially in accord with our hypothesis. They were surprisingly higher overall than would be expected and called into question the validity of the self-report measure. Nearly 64% of the group reported activity levels sufficient to satisfy recommendations of the 2008 Healthy America (
14) program. In comparison, the 2009 National Youth Risk Behavior Survey found that only 37% of high school youths met the physical activity criteria, defined as engaging in physical activity that increased their heart rate and made them breathe hard some of the time for at least 60 minutes for five of the days in the week preceding the survey (
23).
Notably, although rates of physical activity reported by youths and caregivers in this study seemed high, there were significant associations between low activity levels and increased overweight and obesity. One possible reason for this association was that the youths and caretakers generally may have overestimated activity levels until they dropped to such a low point that they were acknowledged. The fact that levels of physical activity are low among many of these youths is unfortunate given the benefits of physical activity for mental health (
24) and for overall health and fitness (
8). In this study rates of recommended activity levels were significantly lower among girls and adolescents than among boys and younger children.
Eighteen percent of the youths reported having had at least one puff of a cigarette in the past month. Using similar criteria, the 2006 National Youth Tobacco Survey (
25) indicated that 19.7% of high school youths reported using cigarettes on one or more of the preceding 30 days. In 2007, 20% of youths attending high school reported current use of cigarettes by the same criteria (
16). The rates reported here are similar and therefore not in accord with our initial hypotheses. Because these data were derived from reports by the youths or their parents or guardians, however, it is not clear if they were underreported, given that the prevalence of tobacco use among youths with mental disorders has been found to be increased (
26). Cigarette smoking is considered a gateway to other forms of substance use, and continued vigilance in efforts to limit smoking in this population is warranted. On the other hand, if these data are accurate, the fact that they are comparable to rates in a normative high school population is encouraging.
Alcohol and drug use rates reported by either standard measure (the CRAFFT) or single question were unexpectedly low and not in accord with our hypotheses. This is surprising given that comorbidity between mental and substance use disorders among youths has been recognized (
26). The National Institute on Drug Abuse Monitoring the Future Survey indicated that in 2009, 18% of tenth grade students used any illicit drug and 30% of tenth grade students used alcohol at least once in the month preceding the survey (
27).
The reasons for the discrepancies in the findings of alcohol and drug use between this population and a community sample are not clear. Underreporting because of concerns about staff disapproval or consequences certainly was likely. For many, cigarette smoking may not carry the degree of family and social criticism associated with alcohol and other substance use or abuse and therefore may be more easily revealed. It also should be recognized that many severely disturbed youths in day hospital or clinic settings are monitored carefully by program personnel and parents and guardians and may have limited access to drug-related activities found in some high school settings. Therefore, although the rates of alcohol and drug use found by this study may be unrealistically low, they may reflect the reality that use of alcohol and drugs among youths with mental illnesses treated at day-treatment centers and clinics may not be as high as imagined.
It should be recognized that although the findings presented here are noteworthy, a number of limitations require caution so as to not overstate the findings. Although the analyses in a number of cases indicated that there were significant relationships among the variables studied, information about other variables that are known to be associated with obesity were not collected for this project. As noted earlier, youths of minority status, as well as those raised in single-parent households and those having low socioeconomic status, for example, all tend to have higher rates of obesity than population samples from which they are drawn (
28,
29). Nonetheless, even among youths who share these demographic characteristics, rates of obesity are lower than those found here among youths with psychiatric disorders.
Psychotropic medications also may be associated with obesity (
4) and should be assessed in relation to these health indicators by future studies. Although all the risk factors assessed by this project are related to physical health, we did not study diagnosable general medical disorders except for obesity. A more comprehensive approach aimed at intervention to improve physical health should address other physical disorders more specifically.
Levels of activity and rates of overweight and obesity in this population were found to be consistent with the hypotheses, but variability in activity levels of youths at clinics or day-treatment programs suggested that some programs may have included or emphasized physical activity more than others. Overall screening rates were fairly good, given that more than 80% of youths were screened after the initial start-up period. Nonetheless, whether findings for those not screened would have altered the results is not known. Missing data may have been associated with particular characteristics, such as noncompliance, that may have affected the findings. This program has relied on self-report to assess cigarette smoking, alcohol and drug use, and activity levels. Reporting by parents and youths was not anonymous, and concerns about confidentiality may have biased the results.
Notwithstanding these concerns, this project has demonstrated the feasibility of creating and implementing a large-scale program to address public health and mental health for youths with psychiatric disorders. When implemented by dedicated staff at multiple locations, a health initiative of this type is able to enroll hundreds of youths and collect thousands of observations systematically. Mental health programs for youths need not—and probably should not—focus solely on mental health issues. Issues related to general medical health should be addressed as well, especially among youths with overlapping health and mental health concerns. Obesity, for example, so common in this population, is the most prevalent chronic health condition in the United States (
4).