Recent epidemiologic investigations have documented that more than two-thirds of American children and adolescents are exposed to at least one traumatic life event by the age of 16 (
1). Traumatic physical injury is a leading cause of death, disability, medical costs, and health service utilization among youths in the United States (
2–
7). Each year more than nine million children and adolescents visit emergency departments and other general medical settings after incurring traumatic physical injuries (
8).
A series of investigations has established that exposure of children and adolescents to traumatic injury is associated with the development of posttraumatic stress disorder (PTSD) symptoms (
9–
26). One recent large-scale epidemiologic investigation found that beyond its association with PTSD, exposure to trauma is associated with the development of other anxiety, depressive, substance use, and disruptive behavior disorders among children and adolescents (
1). Smaller-scale investigations in subgroups of injured youths have also suggested that the symptoms of other anxiety, depressive, substance-related, and behavioral disturbances can occur in the wake of traumatic physical injury (
27–
34).
A review of the literature also indicates that it is unclear whether children and adolescents who incur traumatic brain injury (TBI) are particularly vulnerable to developing postinjury psychiatric disorders (
32,
34–
40). A better understanding of the full spectrum of psychiatric disorders that may develop in the wake of childhood injury is important given that studies focusing on postinjury functional limitations suggest that higher initial emotional distress is associated with enduring functional impairments (
41,
42). Also, recent commentary and investigation suggest that late childhood and early adolescence may be an optimal window in which to focus preventive interventions for many anxiety, mood, substance use, and disruptive behavior disorders (
43,
44).
In reviewing the literature, we found few population-based clinical epidemiologic investigations that have examined the full spectrum of provider-recognized psychiatric disorders that have affected children and adolescents exposed to a traumatic injury; prior investigation has predominantly focused on PTSD. Also, few population-based investigations have assessed the postinjury prescription of psychotropic medication to children. Therefore, in this investigation we aimed to compare rates of provider-diagnosed psychiatric disorders and psychotropic medication prescription in a population-based sample of injured and noninjured children and adolescents aged ten to 19. We hypothesized that compared with noninjured youths, those exposed to traumatic injury would demonstrate clinically and statistically significant elevations in a full spectrum of provider-diagnosed anxiety, depressive, substance-related, and behavioral disorders and in frequency of receipt of prescriptions for psychotropic medication. In this investigation we also hypothesized that any elevations in disorders or prescriptions observed among injured youths would persist even after adjustments for relevant demographic and clinical characteristics. The investigation also aimed to explore variations in the diagnosis of postinjury psychiatric disorders and psychotropic medication prescriptions for youths exposed to TBI.
Methods
Overview
The investigation was a population-based prospective cohort study of youths enrolled in the Group Health Cooperative, a large integrated delivery system and health plan in the Pacific Northwest. All youths aged ten to 19 in 2001 who were continuously enrolled in the health plan for a seven-year period from 1998 to 2004 were included in the investigation. Their automated, deidentified medical records documented inpatient, emergency department, and outpatient visits; pharmacy prescription records; and demographic characteristics. The Group Health Cooperative and University of Washington institutional review boards approved all study procedures; a waiver of informed consent was obtained in this secondary data-analytic investigation of deidentified medical records.
Injury visits and severity
All adolescent inpatient, emergency department, and outpatient visits between 1998 and 2004 were reviewed for
ICD-9-CM codes indicative of traumatic injury. Injuries included in the investigation were fractures (codes 800–829); dislocations (codes 830–839); sprains and strains of joints and adjacent muscles (codes 840–848); intracranial injury (codes 850–854); internal injury of the chest, abdomen, and pelvis (codes 860–869); open wound of the head, neck, and trunk (codes 870–879); open wound of the upper and lower limbs (codes 880–897); injury to the blood vessels (900–904); late injury effects (codes 905–909); superficial injury (codes 910–919); contusions (codes 920–924); crushing injury (925–929); foreign-body injuries (codes 930–939); burns (codes 940–949); injury to nerves and spinal cord (950–957); and other injury complications (codes 958–959). Specific
ICD-9-CM codes used to identify TBI included 800.0–801.9, 803.0–804.9, 850.0–854.1, and 959.01 (
45,
46).
Injury severity and maximum Abbreviated Injury Scale score
Severity of injury by body region was coded with the Abbreviated Injury Scale (AIS) in order to determine each person's maximum AIS score (MAXAIS) (
47,
48). The AIS was designed 30 years ago and is the most accepted anatomic measure of injury severity. It has been shown to be highly correlated with threat to life as well as postinjury disability and quality of life (
47,
48). The MAXAIS, calculated as the highest AIS score for a single injury received, performs well as a single measure of injury severity; it has an area under the receiver operating characteristic curve of .88 for mortality in a national database of over 75,000 patients (
49).
Psychiatric diagnoses
For all youths aged ten to 19 in the index year (2001), we reviewed the automated records to identify one or more
ICD-9-CM psychiatric diagnoses made by a Group Health Cooperative provider over the seven-year study period. On the basis of a recent epidemiologic investigation (
1) as well as prior studies of traumatically injured children and adolescents (
29–
31,
50), we derived the following combined categories of psychiatric disorders from
ICD-9-CM codes: anxiety and acute stress (including PTSD, 309.81; acute stress disorders, 308.0–308.9; adjustment disorders, 309.0–309.9; panic disorder, 300.01, 300.21, and 300.22; phobia, 300.29; social anxiety, 300.23; obsessive-compulsive disorder, 300.3; generalized anxiety disorder, 300.02; other anxiety, 293.84, 300.00, 300.09, and 300.2; and other childhood anxiety, 313.0), depressive disorders (including major depressive disorder, 296.2–296.99; dysthymia, 300.4; and other depressive disorders, 309.1 and 311.0), substance use disorders (including alcohol use disorders, 291.0–291.3, 291.5, 291.8, 291.9, 303.0, 303.9, and 305.0 and drug use disorders, 292.0, 304.0, and 305.2–305.9), and disruptive behavior disorders (including attention-deficit hyperactivity disorder [ADHD], 314.0–314.9; conduct disorder, 312.0–312.4, 312.8, and 312.9; and oppositional defiant disorder, 313.81).
Psychotropic medication prescription
Group Health Cooperative pharmacy records were reviewed to identify psychotropic medication prescriptions. Psychotropic medication prescriptions from the following classes of medication were included: antidepressants (bupropion, citalopram, desipramine, doxepin, escitalopram, fluoxetine, fluvoxamine, imipramine, mirtazapine, nefazadone, nortriptyline, paroxetine, sertraline, trazodone, and venlafaxine), anxiolytics (alprazolam, buspirone, chlordiazepoxide, clonazepam, diazepam, oxazepam, and triazolam), antipsychotics (aripiprazole, fluphenazine, haloperidol, molindone, olanzapine, perphenazine, pimozide, quetiapine, risperidone, thioridazine, and ziprasidone), and mood stabilizers (lithium). Stimulant medications were unavailable from pharmacy records and therefore were not included in the investigation.
Data analyses
We first described the demographic, clinical, and injury characteristics of the cohort and divided the cohort into two groups, youths with and without any ICD-9-CM-documented injury visits in 2001. Next, the frequencies of documented anxiety or acute stress, depressive, substance use, and disruptive behavior disorders as well as psychotropic medication prescription were ascertained for members of the two groups over the course of the three subsequent years (2002–2004).
The unadjusted associations between injury in 2001 (yes or no) and the four categories of psychiatric disorders (yes or no) and psychotropic medication prescription (yes or no) were assessed for the 2002–2004 period. We constructed longitudinal regression models for 2002 to 2004 to ascertain the association between youth injury in 2001 and any psychiatric diagnosis or psychotropic medication prescription alone or in combination. While adjusting for other clinical and demographic characteristics, five models using generalized estimating equations longitudinally assessed for an independent association between injury in 2001 and anxiety and acute stress, depressive, substance use, and disruptive behavior disorders as well as psychotropic prescriptions. Repeated measurements of the four categories of psychiatric disorders or psychotropic medication prescription in 2002, 2003, and 2004 were the dependent variables. The primary independent variable included in each model was injury visit in 2001 (yes or no). Covariates included in each of the five models were age, gender, one or more psychiatric diagnoses in 1998–2000, one or more psychotropic medication prescriptions in 1998–2000, the presence of one or more TBIs or any other injury in 1998–2000, and injury severity (MAXAIS) for injuries incurred in 1998–2000 and in the index year of 2001. Exploratory analyses assessed whether youths who incurred a TBI in 2001 had increased odds of receiving psychiatric diagnoses or a psychotropic medication prescription relative to both noninjured youths and youths who had incurred any other type of injury (non-TBI) in 2001.
Outcomes for all unadjusted and adjusted associations were expressed as odds ratios (ORs) and 95% confidence intervals (CIs) (
51–
53). Odds ratios are commonly used in cohort studies because they allow for a quantitative comparison of the outcome of interest in the exposed versus unexposed groups (in this investigation, youths exposed to an injury in 2001 compared with youths not exposed to an injury in 2001).
Finally we performed sensitivity analyses for the multivariate regressions using, first, individual preinjury psychiatric diagnoses (including anxiety and acute stress, depressive, substance use, and disruptive behavior disorders in 1998–2000) in place of a combined category of one or more psychiatric diagnoses in 1998–2000, and second, the MAXAIS for each of seven body regions (head, thorax, abdomen, spine, upper extremity, lower extremity, and integument) in addition to the overall injury severity score (the MAXAIS from multiple regions). Analyses were conducted with SAS, version 9.2, data-analytic software.
Results
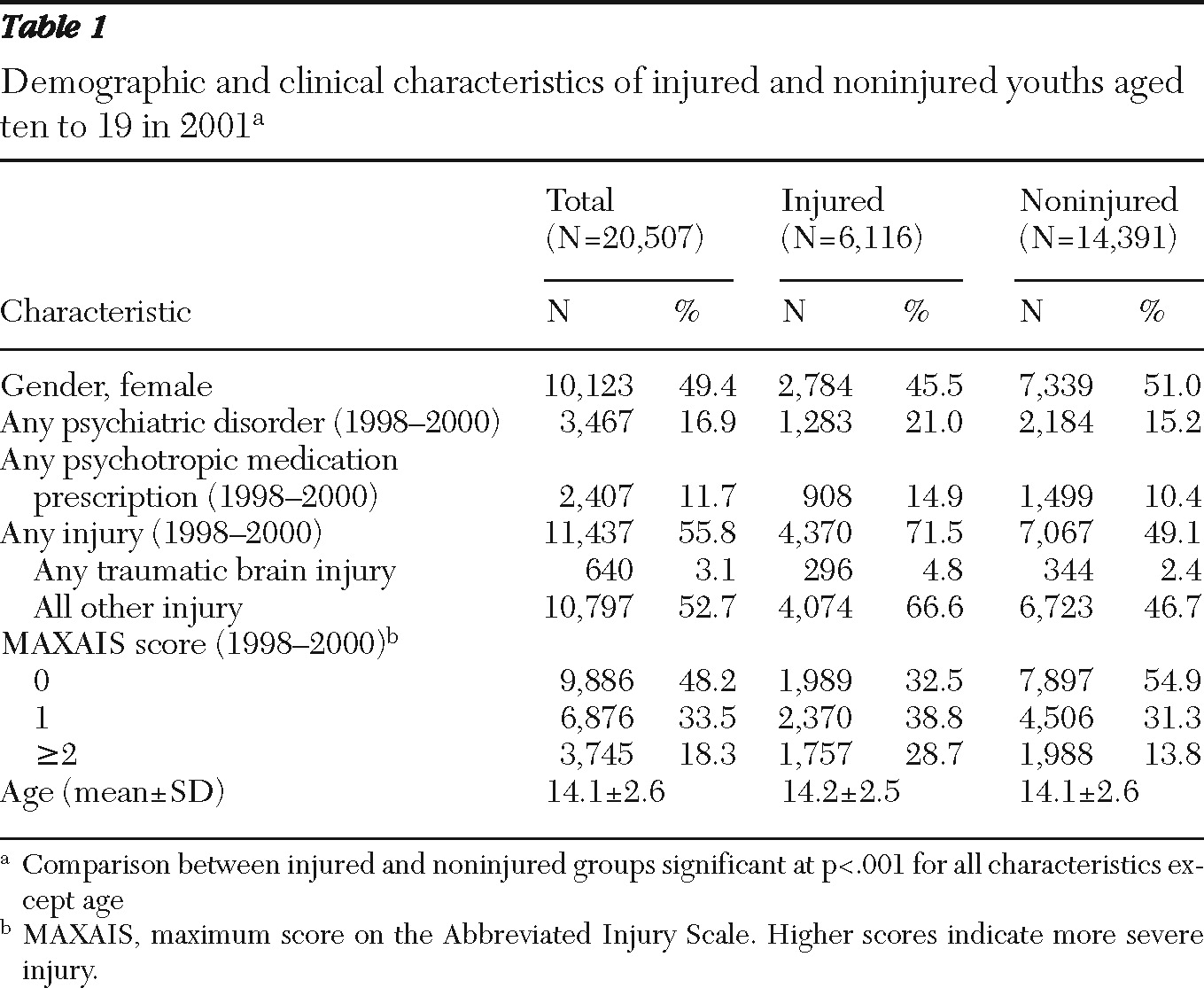
In 2001 there were 20,507 youths aged ten to 19 who were continuously enrolled in the Group Health Cooperative (
Table 1). The mean±SD age of youths in the cohort was 14.1±2.6, and 49.4% were female. Approximately 30% of these youths had one or more injury visits in 2001. Two hundred fifty-two individuals (1.2%) had an injury visit secondary to a TBI. Among the 6,116 adolescents with an injury visit in 2001, 142 (2.3%) required hospitalization, 738 (12.1%) had one or more emergency department visits, and 5,949 (97.3%) had one or more ambulatory care or outpatient visits. With regard to injury severity, 3,794 adolescent injury visits were associated with a MAXAIS of 1, 1,674 visits were associated with a MAXAIS of 2, and 63 visits were associated with a MAXAIS ≥3. Children and adolescents injured in 2001 were more likely to be male; injured youths also were more likely than those not injured to have one or more prior psychiatric diagnoses, prescriptions for psychotropics, or injuries in 1998–2000 (
Table 1).
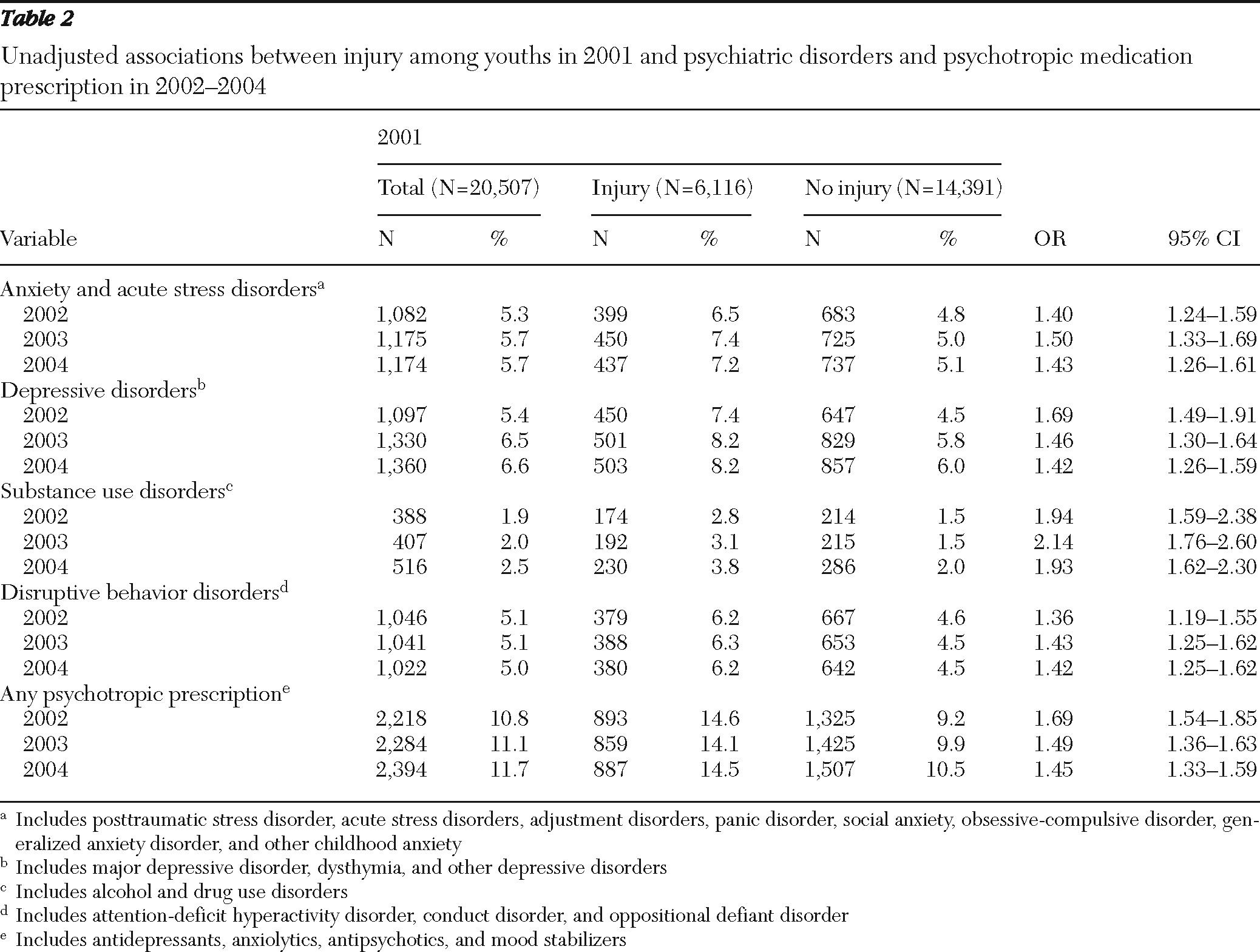
Youths with one or more psychiatric diagnoses constituted 13.0% of the cohort in 2002, 14.2% in 2003, and 14.5% in 2004. Between 10.8% and 11.7% of youths received one or more psychotropic medication prescriptions in the 2002–2004 period. Over the course of the three years after the index injury, a pattern of elevated odds for individual ICD-9-CM diagnoses was observed. In unadjusted analyses, youths exposed to injury had significantly greater odds of having a diagnosis of acute stress disorder, PTSD, an adjustment disorder, anxiety disorder, major depressive disorder, dysthymia, an alcohol or drug use disorder, ADHD, conduct disorder, and oppositional defiant disorder compared with youths unexposed to injury. As an example, .3% of all youths had a diagnosis of PTSD in 2002, 2003, and 2004. In unadjusted analyses, youths injured in 2001 demonstrated significantly elevated odds of receiving a PTSD diagnosis over the course of the three years after injury (2002, OR=2.78, CI=1.68–4.61; 2003, OR=1.90, CI=1.16–3.10; 2004, OR=2.43, CI=1.51–3.93).
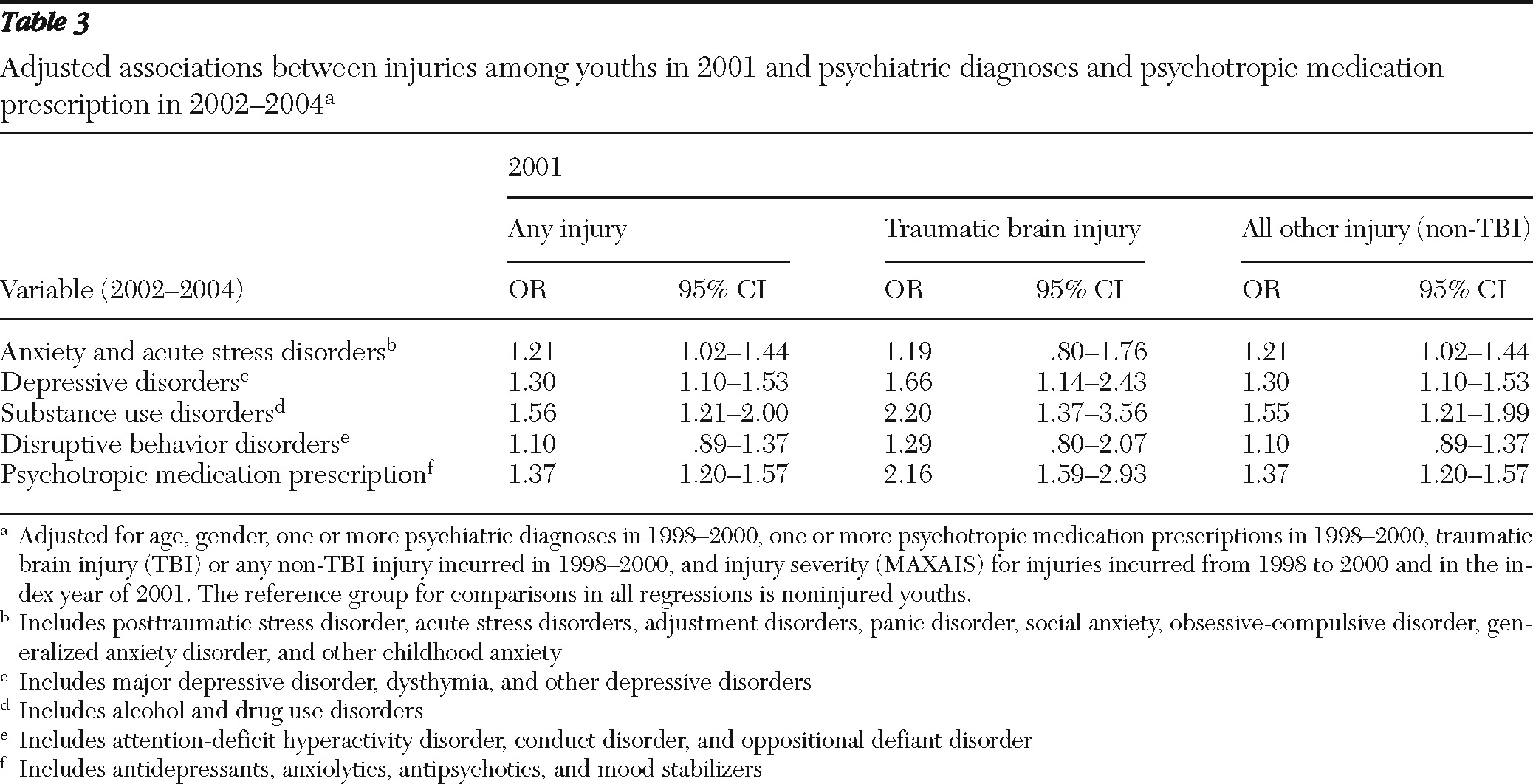
Youths injured in 2001 were more likely than noninjured youths to receive one or more diagnoses of anxiety or acute stress, depressive, substance use, and disruptive behavior disorders in the subsequent three-year period (
Table 2). Youths injured in 2001 were also more likely to have received prescriptions for one or more psychotropic medications in 2002–2004 (
Table 2). In regression models that adjusted for clinical and demographic characteristics, adolescents injured in 2001 had significantly elevated odds of receiving diagnoses of anxiety or acute stress, depressive, and substance use disorders over the three years after injury (
Table 3). Adjusted regression models also revealed a significant association between injury in 2001 and the prescription of psychotropic medication in 2002–2004 (
Table 3). Compared with noninjured youths, those who incurred a TBI had significantly higher odds of receiving depressive and substance use diagnoses as well as psychotropic medication prescriptions (
Table 3). Youths with TBI also had significantly elevated odds of receiving psychotropic medication prescriptions compared with injured youths without TBIs (OR=1.58, CI=1.19–2.08). Compared with youths with non-TBI injuries, youths with a TBI did not show significantly higher odds of having a diagnosis from any combined category of psychiatric disorder.
One or more preinjury psychiatric disorders in 1998–2000 demonstrated the strongest independent associations with psychiatric disorders and psychotropic medication prescription from 2002 to 2004 (OR range 2.96–15.13). Psychotropic medication prescriptions for the period 1998–2000 also demonstrated strong independent associations with 2002–2004 psychiatric disorders and prescriptions (OR range 1.21–3.01). Female gender was associated with increased odds of receiving a diagnosis of anxiety or acute stress disorder (OR=1.37, CI=1.31–1.43) or a depressive disorder (OR=1.50, CI=1.44–1.58) and receiving a prescription for psychotropic medications (OR=1.36, CI=1.32–1.41). However, being female was associated with diminished odds of receiving a diagnosis of a substance use disorder (OR=.76, CI=.71–.82) or a disruptive behavior disorder (OR=.71, CI=.67–.75). Having one or more non-TBI injuries between 1998 and 2000 was significantly associated with increased odds of having a diagnosis of any psychiatric disorder and a psychotropic prescription within 2002–2004 (OR range 1.16–1.32). In contrast, receiving one or more TBIs between 1998 and 2000 was associated only with significantly increased odds of a diagnosis of a substance use disorder (OR=1.63, CI=1.11–2.41) and psychotropic medication prescription (OR=1.44, CI=1.16–1.81) in 2002–2004.
Sensitivity analyses that incorporated individual preinjury psychiatric diagnoses and MAXAIS for individual body regions did not substantially alter the magnitude, pattern, or significance of the vast majority of associations between an injury in 2001 and diagnosis of psychiatric disorders in 2002–2004 (
Table 3).
Discussion
This population-based, prospective investigation identified an increased risk of receiving a broad spectrum of psychiatric diagnoses, including anxiety or acute stress, depressive, and substance use disorders, among youths aged ten to 19 who were exposed to a single traumatic injury. Consistent with prior reports, 30% of youths aged ten to 19 had at least one injury visit in the index year (
5,
54). Prior study of more severely injured youths who required hospitalization also suggests that a full spectrum of anxiety, depressive, and substance use symptoms may be prominent in the months after exposure to traumatic injury (
29). In this study, the observed independent association between exposure to a single injury and the subsequent increased risk of receiving psychiatric diagnoses is particularly relevant given that the vast majority of injuries were relatively minor (MAXAIS of 1 or 2). In contrast to prior reports, this investigation did not find a significantly elevated risk of disruptive behavior disorder diagnoses for youths exposed to traumatic injury after analyses adjusted for demographic and preinjury clinical characteristics (
1,
30).
PTSD was infrequently diagnosed among youths over the course of the three years after injury exposure; however, youths incurring injuries frequently received other anxiety, depressive, and substance-related diagnoses. The investigation also observed that injury-exposed children and adolescents were more likely to receive psychotropic medication prescriptions. These findings corroborate and extend observations from previous child and adolescent epidemiologic studies (
1,
44) and suggest that postinjury mental health services may need to address the full spectrum of psychiatric presentations among injured children and adolescents.
Preinjury psychiatric history was strongly associated with receiving postinjury psychiatric diagnoses and psychotropic medication prescription. Also of note, traumatic injuries incurred before 2001 were independently associated with an increased risk of postinjury psychiatric diagnoses and psychotropic medication prescription. Prior reports suggest that pre-event psychopathology and recurrent trauma among youths and their family members are associated with an increased risk of developing PTSD and related psychiatric disorders (
1,
21,
22,
30,
55). These collective findings suggest that postinjury screening and intervention protocols in acute care and pediatric practice settings may need to target high-risk children and adolescents who have been exposed to multiple injury events or who have a history of psychiatric disturbances.
Consistent with prior reports, approximately 1% of youths in the cohort had sustained a TBI in 2001 (
56). Youths with a TBI had a significantly increased risk of receiving psychotropic medication prescriptions but not of having psychiatric disorders compared with youths incurring non-TBI injuries. However, the relatively small number of youths with a TBI may have limited the investigation's ability to detect significant associations. Some (
57,
58) but not all (
34) prior investigations have found equivalent rates of psychiatric symptoms among children with TBI and other kinds of injury. Anatomic differences in TBI symptom presentations may explain some of the observed variations in findings across investigations (
59).
This investigation has a number of limitations predominantly related to the use of large administrative databases to ascertain psychiatric diagnoses (
60,
61). Assignment of diagnoses relied on diagnostic codes that frequently derived from assessments by general medical providers rather than mental health specialty providers. This may have affected the accuracy of specific
ICD-9-CM diagnostic categories in the investigation.
Diagnostic inaccuracies could in part explain the low observed rates of postinjury PTSD in the cohort. Also, the increased rate of diagnoses observed after the index injury could be explained in part by the increased likelihood of detecting a disorder related to an injury visit. Thus an alternative explanation for the observed increased rates of diagnoses and medication prescription could be that preexisting psychiatric disorders were detected when youths were injured and happened to visit their provider.
The investigation was also limited by the arbitrary annual categorization of injury visits; it is quite possible that visits for a single injury extended across years (for example, an initial injury in December of 2000 would likely have had a follow-up in January 2001). Furthermore, because of the diversity of postinjury visit types (including visits to the emergency department, physical therapy, and primary care), it was difficult to directly control for number of these visits in multivariate analyses. Also, several demographic and clinical characteristics, such as ethnicity, family income, and social support, were not assessed. Thus we cannot rule out the possibility that other unmeasured characteristics related to both the occurrence of childhood injury and psychiatric disorders partially explain the observed association between injury and increased risk of psychiatric disorders.
An important limitation of the investigation is that no information is provided on children with undiagnosed disorders. An additional limitation is the lack of automated data from the Group Health Cooperative regarding the stimulant class of psychotropic medication prescriptions. Finally, the current investigation did not fully explore the effects of individual preinjury psychiatric diagnoses or injuries to specific body regions on the development of postinjury psychiatric disorders; these issues could be productively addressed in subsequent investigations.
Conclusions
Beyond these considerations this investigation has important implications for the detection and treatment of child and adolescent emotional disturbances in general medical settings (
62). Prior investigations suggest that there are deficits in the quality of postinjury psychiatric care such that even when adolescent posttraumatic psychiatric symptoms are detected by primary care providers, difficulties may arise in service coordination and initiation of evidence-based mental health treatment (
29,
63). Our investigation suggests at a population level that injury is associated with an increased risk of having a broad spectrum of psychiatric disturbances. Future research should corroborate and extend the finding of an association between childhood injury and the development of psychiatric disorders before population-based screening efforts are implemented. Although psychiatric disorders appear to be detected by general medical providers at postinjury visits, it is unclear whether high-quality evidence-based mental health treatments are being initiated.
Future stepped-care investigations could test relatively simple screening algorithms and computerized intervention strategies that link primary care providers' detection of postinjury psychiatric disturbances with collaborative care consultation (
64). Computerized notification linking pediatric primary care with stepped-up mental health consultation within integrated health plan populations, such as the Group Health Cooperative, may be a key method of enhancing the quality of mental health care for injured youths. Ultimately, population-based surveillance procedures that integrate screening, detection, and stepped-care interventions targeting the full spectrum of postinjury psychiatric disorders could be developed and tested (
64). Future research efforts could be linked to changes in policy surrounding the delivery of high-quality, sustainable mental health care for injured children and adolescents treated in general medical settings (
65,
66).
Acknowledgments and disclosures
This work was supported by grants R01-MH073613 and K24-MH086914 from the National Institute of Mental Health and by grant R49-CCR316840 from the National Center for Injury Prevention and Control and the Centers for Disease Control and Prevention.
The authors report no competing interests.