Economically disadvantaged women with major depression and childhood sexual abuse histories constitute a substantial segment of the patient population in publicly funded community mental health centers (CMHCs) (
1). The mental health burden of co-occurring major depression and childhood sexual abuse includes elevated risk of chronic and recurrent depression, comorbid posttraumatic stress disorder (PTSD), borderline personality disorder, suicidal behavior, and heightened shame (
2–
8). Research is needed to examine the transportability and effectiveness of evidence-based therapies in CMHCs, where a large percentage of low-income women and those with a history of trauma receive care (
9).
Epidemiological studies have shown that a sexual abuse history significantly increases risk of adult major depression and that more severe forms of abuse increase the odds more than threefold (
6). One prospective study reported higher rates of treatment seeking among women with documented sexual abuse compared with women in the general population (
10). In mental health settings, estimates of reported childhood sexual abuse range from 35% to 75% (
11). Depression and childhood sexual abuse co-occurred among approximately 25% of treatment-seeking women in a CMHC (
1). Women who have been sexually abused are more likely to experience difficulties maintaining stable intimate relationships, poor communication with intimate partners (
4), and relationship dissatisfaction (
4). They are at increased risk of adult sexual assault and intimate partner violence (
3,
8,
12) and intergenerational transmission of sexual abuse (
13). Psychotherapeutic interventions, to be effective, must respond to these interpersonal patterns and challenges and accommodate resulting disruptions to treatment engagement.
The aim of this randomized controlled trial was to examine whether interpersonal psychotherapy (
14) would produce greater mental health gains than usual care for women with major depression and sexual abuse histories who were seeking treatment at a CMHC. In a previous uncontrolled pilot study, we found that interpersonal psychotherapy was well suited to the concerns of depressed women with sexual abuse histories and well received by staff therapists (
1). Interpersonal psychotherapy has demonstrated efficacy in improving severe and recurrent depression (
15), shown promise for treating PTSD (
16,
17), and improved clinical outcomes among women with low income and from racial-ethnic minority groups (
1,
16,
18).
Here, we report on the effectiveness of interpersonal psychotherapy compared with usual care individual psychotherapy, delivered by staff therapists serving a primarily low-income, racially and ethnically diverse, urban patient population. To maximize representativeness and the application of findings to public-sector mental health care, we included women prescribed psychotropic medications before study entry as well as those with comorbid conditions, such as PTSD and borderline personality disorder, and current severe stressors, such as intimate partner violence. The primary hypothesis was that interpersonal psychotherapy would lead to lower levels of depressive symptoms than usual care at 36 weeks postrandomization. Secondary hypotheses were that interpersonal psychotherapy would lead to greater reductions in PTSD symptoms and shame and better social and mental health-related functioning.
Methods
Participants
The trial was conducted from September 2004 to August 2007 in a CMHC at the University of Rochester Medical Center and was approved by the university's institutional review board. In total, 1,100 women seeking treatment in the clinic were screened by intake clinicians for study eligibility on the basis of presence of depressive symptoms and self-report of sexual abuse before age 18 and absence of exclusion criteria.
Inclusion criteria were 18 years or older, English speaking, current major depression, and childhood sexual abuse. Major depression was established through the Structured Clinical Interview for Axis I DSM-IV Disorders (
19), and sexual abuse history was established through a structured clinical interview on life events (
1). Sexual abuse was defined as before age 18 having any unwanted sexual contact or any sexual contact with a family member who was five or more years older. Sexual contact was defined as physical contact of a sexual nature, ranging from fondling to sexual intercourse. Exclusion criteria were active psychosis, history of schizophrenia or bipolar disorder, intellectual disability, substance abuse or dependence within the previous three months, and current involvement in psychotherapy.
A total of 230 (21%) had depressive symptoms and reported sexual abuse. Of these, 125 (11%) met eligibility criteria and were given a letter describing the study and requesting their agreement for study personnel to contact them; 105 patients agreed to be contacted, five women decided not to participate, and ten were lost to contact.
After a complete description of the study was provided, the 90 participants gave written informed consent during the baseline assessment. Of these, 20 were excluded because of active substance abuse or dependence (N=8), active psychosis (N=5), not meeting criteria for major depression (N=4) or childhood sexual abuse (N=1), and not completing the baseline assessment (N=2).
Procedures
Seventy patients were randomly assigned to interpersonal psychotherapy (N=37) or to usual care (N=33). Usual care was referred to as individual psychotherapy in pamphlets distributed to patients; both treatments were presented as credible interventions for depression. Consistent with prior CMHC-based effectiveness research (
20), changes in psychotropic prescriptions during the trial were permitted. Assessments were conducted at pretreatment and at ten, 24, and 36 weeks after randomization. One master's-level research assistant, who was aware of patients' treatment assignments, conducted all assessments. Instruments were sometimes administered aloud to accommodate patients' reading level or preference.
Meetings including study investigators and the research assessor were held to establish consensus on clinical diagnoses. The Structured Clinical Interview for DSM-IV Personality Disorders (
21) was used to assess borderline personality disorder.
Assessments
Trauma history was assessed with the Childhood Trauma Questionnaire-Short Form (
22), a self-report measure of the perceived frequency of physical and emotional abuse, sexual abuse, and physical and emotional neglect, and with the Traumatic Life Events Questionnaire (
23), a self-report measure of lifetime trauma experiences.
Depressive symptom change was assessed with the Beck Depression Inventory-II (BDI-II) (
24), a well-validated self-report measure, and the 17-item Hamilton Rating Scale for Depression (HRSD) (
25), a well-validated interviewer-administered measure.
PTSD symptoms were measured with the Modified PTSD Symptom Scale-Self Report (
26), which produces a score reflecting the frequency and severity of PTSD symptoms. Mental health-related functioning was assessed with the Medical Outcomes Study 36-Item Short-Form Health Survey summary score (
27). Social functioning was measured by the Social Adjustment Scale-Self Report (
28), which examines social role performance in six domains. Finally, shame was assessed with the corresponding subscale of the Differential Emotions Scale (
29), wherein respondents report the frequency of experiences of shame in their daily lives.
Study therapists
CMHC staff clinicians (ten master's level, three doctorate level) delivered the treatments. Half of the therapists identified availability during a common group supervision time and were assigned to interpersonal psychotherapy training. The training consisted of 30 hours of group didactic training, intensive review of a treatment manual (
30), and supervision by the principal investigator for two to three training cases. All interpersonal psychotherapy sessions were audiotaped or videotaped. The principal investigator reviewed 20% of taped sessions for treatment fidelity and addressed deviations from the model with the therapist. Therapists were required to complete at least one full 16-session treatment that demonstrated their adherence to and competence in interpersonal psychotherapy. All of the interpersonal psychotherapists successfully completed the training and reported a high level of satisfaction with the treatment. The two therapist groups had comparable professional experience and degrees, equivalent weekly clinical supervision, and equivalent caseloads. To accommodate the competing demands on time and resources in this patient population and an anticipated no-show and cancellation rate of 33%, the expected 16 sessions could be conducted over the 36-week trial.
Interpersonal psychotherapy
Interpersonal psychotherapy for major depression is a time-limited, manualized treatment that aims to improve patients' symptoms by effecting change in their interpersonal functioning and quality of social supports (
15,
30). Interpersonal psychotherapy has theoretical roots in attachment theory (
30) and emphasizes the formative influences of early interpersonal relationships. Three problem foci (grief and loss, role transitions, and interpersonal conflict) emphasize current interpersonal problems, and a fourth reflects an enduring interpersonal style (
30). The therapist and patient together select the problem focus.
On the basis of pilot work with this population (
1,
31), we recast the fourth interpersonal problem area as “interpersonal patterns” to reflect the persistent interpersonal difficulties often associated with interpersonal trauma. This modification is described elsewhere (
31). The interpersonal patterns problem area was designed to help women recognize long-standing, trauma-related patterns of behavior and emotion in relating to others that undermined relationship satisfaction. Preliminary work demonstrated that most women readily perceived interpersonal patterns that hampered their interpersonal effectiveness (
1). Abuse and trauma histories were obtained during initial treatment sessions as part of the psychosocial assessment. Although current interpersonal difficulties were the focus, the influence of abuse and trauma on current interpersonal functioning was included in the interpersonal formulation and therapy narrative.
Usual care psychotherapy
Usual care therapists were not proscribed from reasonable therapeutic activities and interventions, excepting use of interpersonal psychotherapy. To maintain ecological validity, the only requirement was that participants receive individual psychotherapy. In posttreatment questionnaires, usual care therapists described therapeutic approaches with study participants as supportive (53%), cognitive-behavioral or dialectical-behavioral (27%), integrated and eclectic (13%), and client centered (7%).
Data analysis
Power was .80 to detect a between-groups, unadjusted effect size of d=.38 for the HRSD and BDI-II outcomes. For all analyses, p<.05 was considered significant. In intention-to-treat analyses, change over time was assessed with generalized linear models with inference based on generalized estimating equations (GEEs) (
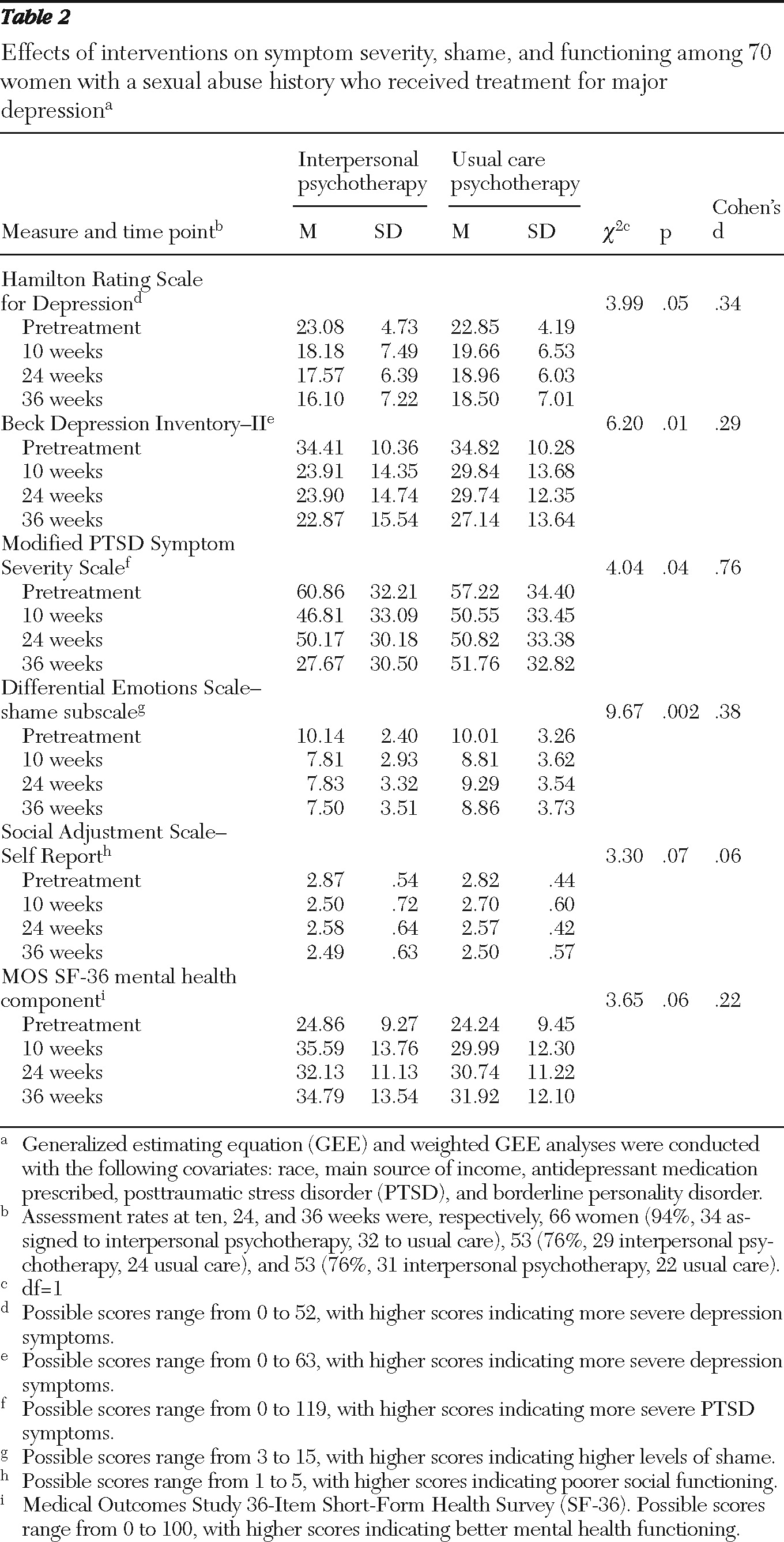
32). To test the assumption that data were missing completely at random (MCAR), logistic modeling was performed to determine whether missing assessment data depended on individual patients' observed responses in previous assessments (Table 2). When the probability of missing values was modeled for each outcome, we found that the shame subscale of the Differential Emotions Scale had informative dropout (p=.04) and violated the MCAR assumption. In that case, weighted GEEs were applied with individual weights estimated from the logistic model for missing data. Women with lower shame scores in earlier assessments were more likely to have missing data in later assessments.
Covariates in all analyses included baseline antidepressant medication prescription (no-yes), race (white or black), main income source (private versus public assistance), active PTSD (no-yes), and borderline personality disorder (no-yes).
Results
Sample characteristics
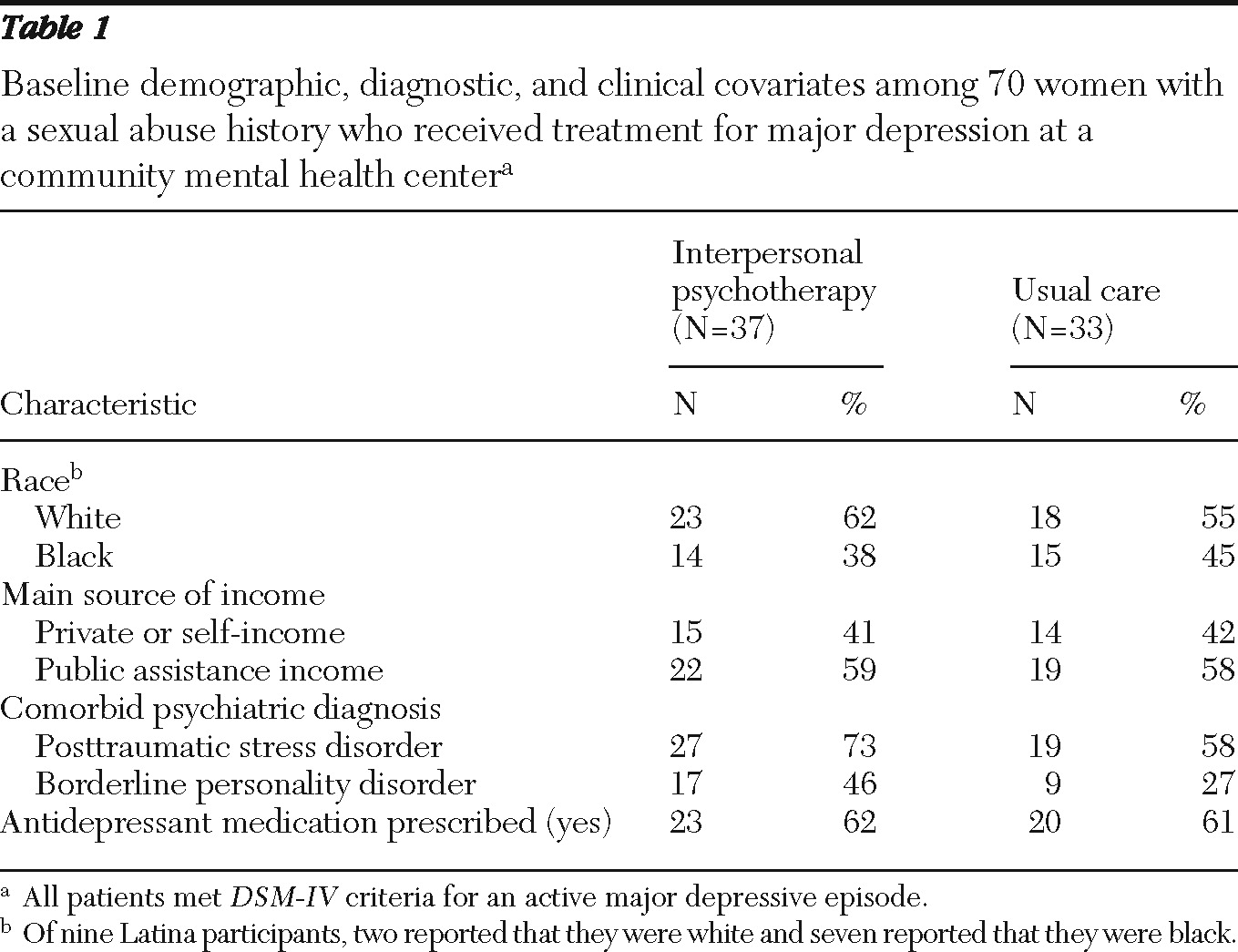
Table 1 shows that randomization was effective: the two groups did not significantly differ on demographic characteristics or diagnostic covariates. Mean±SD age was 36±10 years. Fifty-one women (73%) were living without a spouse or partner, and 33 (47%) had minor-age children living in the home. Most women were unemployed and were Medicaid beneficiaries: 48 (69%) and 46 (66%), respectively.
Trauma histories were extensive. Sixty-seven (96%) women reported moderate to severe levels of sexual abuse on the Childhood Trauma Questionnaire. Most reported moderate to severe childhood physical and emotional abuse: 48 (69%) and 52 (74%), respectively. A majority of women (N=48, 69%) reported current or past intimate partner violence, and 28 (40%) reported sexual assault in adulthood on the Traumatic Life Events Questionnaire.
Diagnostic data collected at the baseline assessment indicated that 51 women (73%) had chronic depression: nine (13%) had had current major depression for at least two years, 29 (41%) had current major depression along with a preexisting dysthymic disorder, and 13 (19%) had recurrent major depression with incomplete remission between episodes over a minimum two-year duration.
Naturalistic interventions
The 36-week assessment and the self-report data showed that 38 of the 53 women assessed (72%) had antidepressant prescriptions: 26 of 30 (87%) in interpersonal psychotherapy and 12 of 23 (52%) in usual care, constituting a significant between-group difference (p=.01, Yates correction). Participants were asked whether they were taking an antidepressant as prescribed, with responses including no prescription, not adherent, partial adherence, or full adherence. Full adherence to medications was reported by 26 of 53 women (49%) at 36 weeks: 18 of 30 (60%) in interpersonal psychotherapy and eight of 23 (35%) in usual care, a nonsignificant difference. Chart review indicated that 11 of the total sample of 70 (16%) used case management services, which was comparable in interpersonal psychotherapy and usual care (19% and 12% respectively).
Session attendance
Interpersonal psychotherapy participants attended approximately twice as many sessions (12.9±6.5) as those in usual care (6.3±4.2), a significant between-group difference (p<.001). A greater proportion of those in interpersonal psychotherapy (17 of 37, 46%) than in usual care (two of 33, 6%) attended 16 sessions in 36 weeks (p<.001).
Clinical outcomes between groups
Table 2 shows the results of GEE analyses comparing the effects of each treatment on clinical outcomes. The results indicate that depressive symptoms, PTSD symptoms, and shame improved more over time in interpersonal psychotherapy than in usual care. Between-group differences in social adjustment and mental health-related functioning were not statistically significant. On the family unit subscale of the Social Adjustment Scale-Self Report (data not displayed), there was a significant treatment advantage for interpersonal psychotherapy (
χ2=3.93, df=1, p=.05). Covariate-adjusted effect sizes ranged from small to large, based on Cohen's (
33) guidelines, and all showed an advantage for interpersonal psychotherapy over usual care at 36 weeks.
Associations between covariates and primary outcomes
Higher depression symptom scores over 36 weeks on the HRSD and the BDI-II were noted for black women versus white women (HRSD, χ2=7.05, df=1, p=.008; BDI-II, χ2=6.94, df=1, p=.008), women receiving public assistance versus not (HRSD, χ2=7.89, df=1, p=.005; BDI-II, χ2=6.96, df=1, p=.008), and those with borderline personality disorder versus those without the disorder (HRSD, χ2=8.88, df=1, p=.003; BDI-II, χ2=8.95, df=1, p=.003). Also, women with PTSD had significantly higher depression symptom scores over time on the HRSD only compared with women without that diagnosis (χ2=3.71, df=1, p=.05).
Secondary analyses
The advantage with interpersonal psychotherapy could not be explained by differences in session attendance for any outcome (data not shown). Session attendance was not significantly associated with any outcome, and inclusion of session attendance as a covariate did not substantially change the overall findings. The inclusion of case management services (yes-no) as a covariate did not alter reported outcomes (data not shown).
Discussion
Approximately 21% of 1,100 women seeking treatment in a CMHC had co-occurring depressive symptoms and childhood sexual abuse histories. Given that this trial recruited from a naturally occurring treatment sample rather than recruiting a sample referred for study participation, the 21% rate is likely representative of this type of clinical setting. Depressed women with sexual abuse histories treated with interpersonal psychotherapy showed more reduction in depressive symptoms, PTSD symptoms, and shame than women who were treated with usual care. Given the 66% rate of comorbid PTSD, it is encouraging that PTSD symptoms were not reactivated and that they improved with interpersonal psychotherapy. Overall, these results suggest that interpersonal psychotherapy was beneficial and had advantages over the usual psychotherapy delivered in a CMHC in producing better treatment engagement and retention, a greater improvement in psychiatric symptoms, and better functioning within the family.
Despite marked improvement, mean depression scores remained elevated after active treatment. Possible contributors to incomplete treatment response include predominance of chronic depression (73% of the sample), high rate of comorbid disorders, interpersonal sequelae of extensive trauma exposure, and socioeconomic disadvantage. Comorbid disorders, including PTSD and borderline personality disorder, are associated with worse treatment outcomes (
34–
37). The interpersonal resources of many women were extremely limited and marked by conflictual family relationships, responsibilities of single parenthood, and social isolation. Practical resource limitations, such as difficulties with transportation, can interfere with women's ability to maintain treatment involvement (
38).
Studies of interpersonal psychotherapy for treating depression in predominantly low-income, racially diverse adult samples are scarce, but a recent report by Grote and colleagues (
18) serves as an interesting comparison. In that study of perinatal depression, pregnant women receiving culturally relevant, brief interpersonal psychotherapy had significantly more improved depressive symptoms than those in enhanced usual care. In that study (
18), BDI score improved from 24.3±10.2 pretreatment to 6.0±4.7 six months postpartum. Our study had relatively higher posttreatment scores (22.9±15.5), with participants more severely depressed at study entry (34.4±10.4). What could account for the different outcomes in these two studies? One plausible explanation concerns the effects of comorbid conditions. In our study sample, rates of comorbid PTSD (66% in ours versus 28% in the perinatal study) and borderline personality disorder (37% in ours; not reported in the perinatal study) accounted for significant variability in depression outcomes. In our sample, 86% of participants had at least one comorbid anxiety disorder (versus 56% in the perinatal sample), which could suppress treatment response (
34). Furthermore, depression chronicity in our sample may explain the less robust treatment gains, as was found in a recent meta-analysis of treatments for chronic depression (
39).
In considering findings from this trial, several limitations should be noted. Our primary aim in this small-scale effectiveness trial of interpersonal psychotherapy was to evaluate whether an evidence-based treatment, when compared with usual care, would improve outcomes. This approach enhances ecological validity, which could increase the likelihood of interpersonal psychotherapy's adoption in community mental health settings if found to be effective (
40). Results suggest that interpersonal psychotherapy enhanced treatment outcomes, but specific contributory mechanisms could not be discerned. For example, the relative contributions of specific components of interpersonal psychotherapy versus general factors, such as working alliance or therapist enthusiasm, are unknown. It is also possible that antidepressant effects contributed differentially to outcomes: at the 36-week assessment, more interpersonal psychotherapy than usual care participants had antidepressant prescriptions, and self-reported adherence was not significantly different between groups. Given this initial finding in favor of interpersonal psychotherapy, further research should investigate possible contributors to change.
Another factor to consider is that the assessor was aware of treatment assignment, which could have introduced bias. We note, however, that depression outcomes were substantially similar on self-report and interviewer-rated measures. Finally, although participants received $30 compensation for completing each research assessment, some types of assistance that could improve treatment engagement in a low-income population (
38), such as transportation and child care, were not available. Although these “real-world” limitations may have interfered with treatment engagement and completion, this clinical trial was representative of usual care in community mental health.
Conclusions
With acknowledgment of these limitations, this study offers new information about the effects of an evidence-based depression treatment when delivered by CMHC therapists for disadvantaged women with sexual abuse histories. Interpersonal psychotherapy relieved the severity of depressive symptoms, PTSD symptoms, and shame and improved functioning within the family to a greater degree than usual care psychotherapy. Overall social functioning and mental health-related functioning were not significantly different between groups. In light of the high dropout rates that are typical in community mental health, it is noteworthy that treatment engagement and retention were stronger in interpersonal psychotherapy than in usual care. Despite the advantages for interpersonal psychotherapy, there was substantial variation in depression outcomes. Multiple factors, independent and converging, may be implicated in suboptimal treatment outcomes. Research is needed to strengthen treatments for women with severe trauma histories and complex psychiatric conditions in community mental health care.
Acknowledgments and disclosures
This work was supported by grant K23-MH064528 from the National Institute of Mental Health.
The authors report no competing interests.