Person-centered care has been endorsed by health care advocates as a means to improve health care encounters and health outcomes (
1–
4). Cultural competence has emerged as an important potential means to enhance person-centered care (
5). However, identification of the specific components of cultural competence remains a work in progress. Achieving organizational cultural competence has been cited to depend on several key components: establishing policies and procedures for language accommodations; modifying or creating new services to meet the specific needs of cultural groups; and bicultural staff, training, and community input (
6). Achieving cultural competence among clinicians has been cited to depend on cultural knowledge and skills, culturally sensitive attitudes, and culturally appropriate behaviors (
7). It is also recognized that evidence-based practices not tested among persons from specific cultural groups may need modification that is based on community input (
8,
9). However, there have been no guidelines for improving the cultural competence of a program—defined here as one or more interventions or services delivered within a specific milieu—at the locus of service delivery.
In this work, we use “cultural group” to refer to a racial-ethnic group, a recent immigrant group, or other underserved groups, such as the Deaf population or lesbian, gay, bisexual, transgender, queer, and intersex populations, that have had difficulty accessing and utilizing mainstream mental health services. Particularly for racial-ethnic groups, programs have been developed, adapted, or modified by community persons and professionals to better accommodate the needs and situations of group members. Program development draws on their firsthand knowledge of a group's strengths, values, and social experiences. In line with the modern view of culture as a distinctive but dynamically changing way of life whose continuity depends on its members' ability both to remember and to adapt (
10,
11), these programs utilize community leverage (
12) to keep services abreast of cultural change. Programs that achieve longevity have community approval, and positive results are called “community-defined evidence-based programs,” emphasizing their grounded evidence (
13). Systematic study of these has the potential for yielding information on how cultural competence might apply to any program serving cultural groups.
We report on a study of three programs—one developed for Latinos, one for Chinese, and one for a multicultural population. To a great extent, they could be considered “community-defined evidence-based programs.” Although they have some evidence of success, they have not yet fully documented their positive results. Our goal with this study was to identify components of these programs to serve as a guide to improve the cultural competence of any program serving persons from one or more cultural groups. Full documentation of the study and a video are available elsewhere (
14,
15).
Methods
Research approvals were received from the Nathan S. Kline Institute's institutional review board (IRB); approval for working with the Latino inpatient program was additionally provided by the New York University School of Medicine's IRB. Recruitment procedures and consent forms used language sensitive to persons from cultural groups and their potential suspicion of scientific research and reluctance to be identified as research subjects. Individual clinical sessions were not observed. Consent forms were translated into Chinese and Spanish.
A semistructured instrument was used to document program elements from four viewpoints: genealogy, structure, processes, and distinctive cultural elements (the instrument is available from the authors). Site research teams of at least two persons from a pool of nine, trained by a senior anthropologist (KH) recorded notes on field observations of program activities and staff interactions. Site program staff and developers were interviewed about the program's historical development. Seventeen discussion groups with site staff, program participants, and family members (N=104) were conducted to ascertain perceptions of cultural accommodation. Six of the groups were conducted in languages other than English. Data were collected in 2008 from June to December. At site research team meetings, field notes and focus group transcripts were reviewed and cultural elements evident in programs were identified in a content analysis consensus process. Site program staff reviewed the resulting syntheses and added clarifying comments. In an iterative process between researchers and site staff, elements were grouped into components.
Three New York State programs were purposefully selected. All had been in existence for more than ten years and carried strong endorsement from participants, community, or professional mental health stakeholders. The programs were Prevention, Access, Self-Empowerment and Support (PASS), a program for 13- to 17-year-old primarily African-American, Afro-Caribbean, and Latino youths experiencing behavioral and emotional challenges and their family members; the Latino Treatment Program, a 19-bed psychiatric inpatient unit in Bellevue Hospital Center, New York City (NYC), for adult Latinos (mixed nationalities) with limited English proficiency and in acute psychiatric distress; and a Chinese Continuing Day Treatment (CDT) program at Hamilton-Madison House Behavioral Health Services, an agency that provides clinical and support services to the diverse Asian populations in NYC.
PASS program
PASS was founded in 1997 by African-American and Afro-Caribbean mental health professionals, consumers, and community volunteers and received initial funding through the New York State Office of Mental Health Reinvestment Act. PASS is conceived as a prevention and empowerment program, rather than as a clinical treatment. Program goals are to improve psychosocial, educational, and community outcomes of the youths and to improve family communication styles. Staff members include senior adult mentors who are persons from the cultural groups of the youths served and are living productive lives in their communities and junior mentors who are graduates of the program. Referrals are made by community members, past PASS participants, schools, or agencies. Costs are covered by the program's funding.
The 12-month program runs over four three-day weekends in retreat-style hotel settings. Access to supports and community resources begins at application and continues over the year. To learn the tenets of the program and to meet staff, parents attend on a weekend before the youth sessions commence and then meet monthly for additional supports, including education to improve interpersonal communication styles in home life. At the first youth weekend, youths are paired with adult and junior mentors. A semistructured, multimodule curriculum is flexibly used in program delivery. Curriculum approaches resemble elements of established mental health treatments: specifically strength-based social work, resiliency training, family psychoeducation, cognitive reframing and behavioral therapy, and motivational interviewing. Other elements resemble those of classic self-help (such as affirmation statements). Skills training is given on how to apply for college, how to interview for a job, social amenities, and community advocacy. Activity sessions are used to reinforce curriculum material and include role playing, talent shows, and celebrations of achievements. A final weekend hosts a graduation ceremony.
Latino Treatment Program
The Latino Treatment Program was formed with Latino leadership at Bellevue Hospital in 1995. The unit evolved from a cultural inpatient unit for Latinos and Chinese patients with limited English proficiency; it was established in 1991 as part of a statewide initiative to develop services for cultural groups. Its cultural adaptations are aligned with the requirements for other inpatient units to stabilize illness through medication and other psychotherapeutic treatments and to return persons to their community as quickly as possible. The program provides psychiatric and psychosocial assessments, medication management and monitoring, individual and group therapy sessions, clinical social work services, and activities for learning, recreation, and social interaction. Cultural adaptations are largely accomplished by involving Latino staff members who are familiar with the problems that families encounter. Patients and their family members receive a cultural assessment, and family members are screened for expressed emotion. Illnesses are sometimes rediagnosed to draw on the staff's ability to distinguish idiomatic Latino cultural expressions from symptoms of more serious mental illness. Community meetings that include patients and staff are held twice daily rather than once a day. A spirituality group is run by a peer who is a nurse. Outreach to families and involvement of clergy are actively pursued. Family members receive culturally modified psychoeducation.
Chinese Continuing Day Treatment program
The parent organization of Hamilton-Madison House's Behavioral Health Care Services began as a settlement house for immigrant groups in lower Manhattan. Many of its current offerings began as storefront programs to meet the needs of Chinese immigrants. The first Chinese social worker in NYC was active in program development. State funding supported the conversion to certified community mental health programs. Staff members are bilingual, and recruitment extends beyond U.S. borders. In addition to the program studied, Hamilton-Madison House also offers individual and family counseling and depression screening for seniors. In the Chinese Continuing Day Treatment program most clients are 45 and older, referred from hospitals, and in need of a structured treatment environment. Attendance is daily for several hours. Almost all clients receive medications. Many are immigrants from China, Taiwan, or Hong Kong, but some are first-generation Chinese-Americans. Staff members, in the United States for an average of ten years, speak the dialects of the various populations seen. An informal curriculum is assembled in updatable binders covering health and hygiene, wellness management, group therapeutic activities, and arts and crafts activities. Primary programming is delivered in a formal classroom setting, with clients at desks arranged in orderly fashion. The room is decorated with art and crafts created by the clients. Recreational activities include karaoke, card and mahjong games, and Ping-Pong. Clients have access to Chinese-language newspapers, and some do Tai Chi exercises.
Results
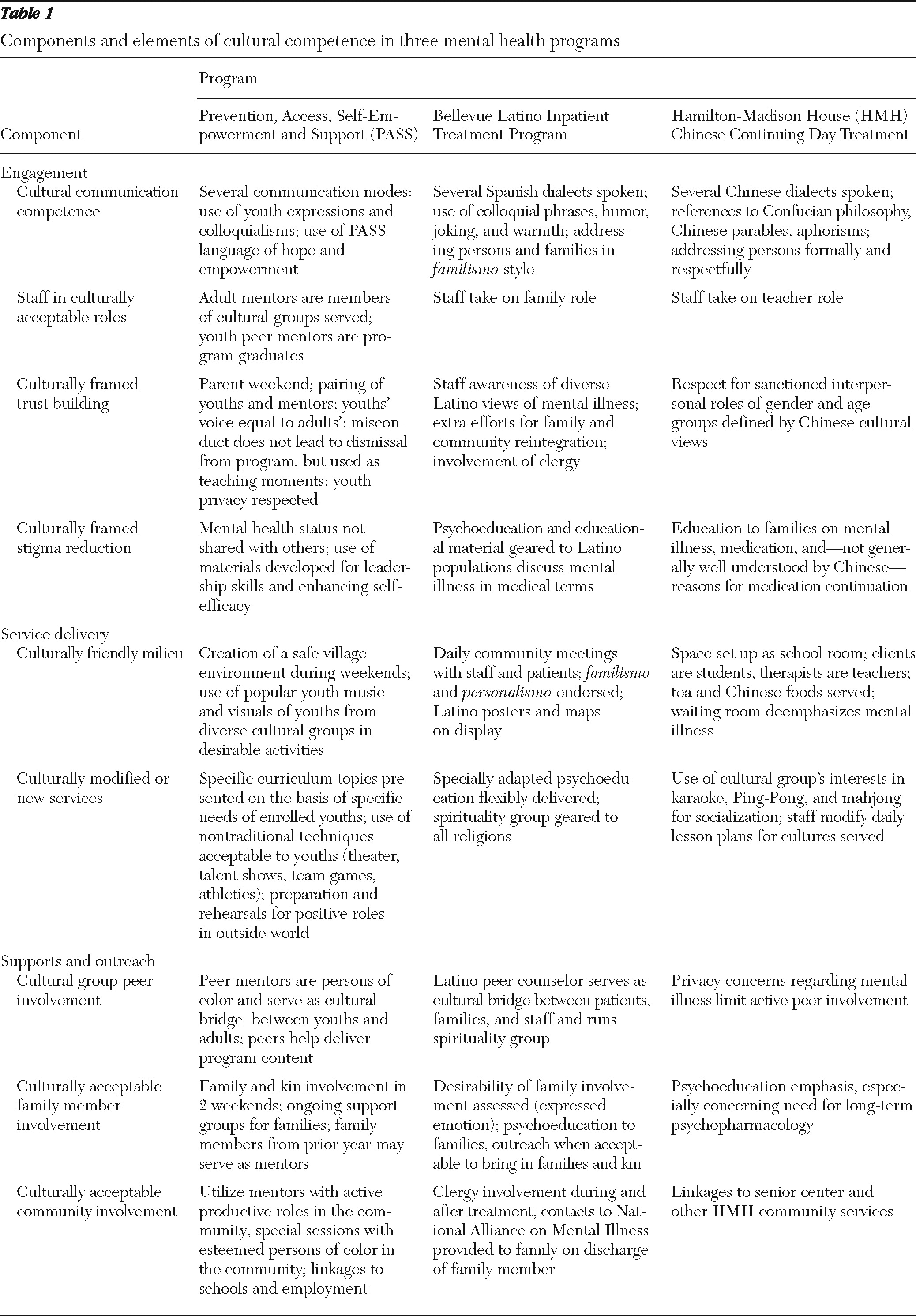
The observed cultural elements of these three programs were grouped into nine cultural competence components, listed with respect to the program activities of engagement, service delivery, and community outreach and supports (
Table 1).
Cultural elements
PASS.
In PASS meeting spaces, music popular among black and Latino youths (such as reggae) is played, and slide shows featuring cultural group members participating in pleasant events are projected. Participants sit at round tables, are given equal opportunity to express their opinions, and are treated respectfully. The colloquial language of youth is often used. The “Eight Keys of Excellence” (
16), a list of affirmation statements about personal values and achievement, are repeatedly invoked, which serves as a communication mode that reinforces the program goals, particularly emphasizing control over one's destiny. The curriculum is flexibly used in response to the needs of the current year's participants. It is written in easy-to-understand language and has age-appropriate illustrations and cartoons. Adult and junior mentors and community speakers all serve as acceptable role models and are easily accessible. Notably, no youth is expelled for behavior, and the basis of youths' daily discussions with junior mentors is not disclosed to other staff. Meals are served at family-sized tables that seat both mentors and youths. Families' questions regarding the program's purpose and their children's safety are addressed in a multifamily session. Family members receive personal supports from parents of former graduates and adult mentors throughout the year.
Latino Treatment Program.
At the Latino Treatment Program, forms, educational materials, magazines, and newspapers are available in Spanish and English. A mural-size map with flags of different Spanish-speaking nations dominates the activities room. There are two dayrooms, and the television in one is tuned to Spanish stations. Spanish music is used in dance movement therapy, and food of the various national Latino groups that make up the clientele is available on special occasions. The bilingual, bicultural staff is knowledgeable of formal and colloquial Spanish. Communication with patients is characterized by familismo, a familial style typical among Latinos. For example, staff members may refer affectionately to patients as “friend” or “daughter.” Patients tend to view doctors paternalistically. Staff members are familiar with the “old ways” of thinking about life, “the core” of a person, as well as culturally contextualized sources of mental distress, social stigma of mental disorders, and gender roles, such as machismo. Local humor or familiar Spanish expressions are proactively used to defuse sensitive situations or to relay information to clients that might be perceived as stigmatizing. The twice-daily community meetings of patients and staff are well attended and serve to enhance familismo.
Extended-family members are generally encouraged to visit and participate in treatment planning from the point of admission. Staff makes extra effort to contact family members, even those outside the United States. The Latina nurse peer counselor serves as a role model for recovery, addresses patient fears regarding medications, participates in discharge planning, provides knowledge on and linkages to community resources, and suggests culturally acceptable ways to navigate the mental health care system. With patients' agreement, clergy are involved in treatment early on.
Chinese Continuing Day Treatment program.
At Hamilton-Madison House, clients have a variety of language needs. Multidialect staff work to engage clients and their families in care by being respectful and welcoming and by taking into account culturally sanctioned age and gender roles. Chinese phrases are used in greetings by staff, including receptionists in waiting rooms. The Chinese Continuing Day Treatment milieu is a classroom setting, and sessions are conducted in an educational manner. Confucian phrases are used to illustrate points. Recreational activities and food served are geared to the Chinese clientele. Waiting areas are similar to those of medical offices, reinforcing the Chinese view of mental disorders as part of a medical spectrum. Western-style services are reviewed for their applicability with Chinese populations, specifically on a one-on-one basis. For example, for some Chinese, there is a reluctance to share potentially shameful information with strangers, and therefore, group therapy would not be recommended. The staff is highly aware of the stigma and shame clients are likely to experience and uses sensitive language in communications. The family is understood to include many generations, and all client-identified members are included in family psychoeducation. Because pharmacological treatments are generally not well understood by family members, extra efforts are made to explain the role of medication in recovery and to point out the dangers of tinkering with prescriptions and dosages.
Components of cultural competency
In addition to providing accurate translation for persons with limited English proficiency, communication competencies cover staff understanding of idioms, colloquial expressions, dialects, and even nonverbal cues, such as proper distancing between persons in oral communications. Culturally acceptable roles are exhibited by staff—as teachers in the Chinese Continuing Day Treatment program, as family members in the Latino Treatment Program, and as youth peers in PASS. Culturally framed trust building was accomplished in PASS by its deliberate efforts to give youths a voice equal to that of adults in light of the unique struggles that African-American and Latino youths can have with adults. Both trust building and culturally framed stigma reduction took place in the Latino Treatment Program through the promotion of familismo in the unit; at the Chinese Continuing Day Treatment program, this was accomplished through staff's use of respectful and nuanced modes of address.
Culturally friendly milieus were created by posters of persons from cultural groups, by magazines in cultural group languages, and by decorations familiar to the culture. In addition, subtle features also conveyed cultural acceptance. For example, the classroom-like setting of the Chinese Continuing Day Treatment program appeals to Chinese values that respect learning and teachers; the pairing of youths with adult and junior mentors and family-style arrangements for meals and accommodations appeal to youths in PASS by creating a community village.
Examples of culturally modified or new services flexibly delivered include the modified psychoeducation programs of both the Latino and Chinese treatment programs, the spirituality group of the Latino program, the lesson-learning skits of PASS, and the recreational activities of all programs. Cultural group peer involvement was a key part of service delivery of PASS; at the Latino Treatment Program a peer nurse ran the spirituality group and participated in team and family meetings. Culturally acceptable family involvement was seen at the Chinese Continuing Day Treatment program, where elders often were participants; at the Latino Treatment Program with its strong family outreach; and at PASS, as an actual service of the program. Community involvement was facilitated at the Chinese Continuing Day Treatment program, through its linkages to its parent organization, a community-based multiservice agency; at the Latino program by the engagement of clergy throughout the program and in community reentry; and at PASS by its program design to have community persons deliver parts of the program, participate in support groups, and facilitate connections for the youths with desirable community resources.
Discussion
A common set of components could be identified from the wide range of specific cultural elements found in the three community-defined evidence-based mental health programs for cultural groups. Any program serving multicultural populations might benefit from an assessment of the extent to which these components are attended to in their daily work. Programs aiming to improve cultural competence could specify, with program staff working in concert with bicultural staff, consumers, cultural peers, and family members, the cultural elements of the components relevant to the populations served. Several of the identified components clearly are markers of a clinically competent program but take on added significance for cultural groups. For example, whereas any program should deal with stigma reduction, stigma concerns are pronounced in cultural groups that see mental illness as shameful to family lineage, as punishment for wrongdoings, and as a deterrent to normal community relations (
17). Trust building, in addition to clinically recommended establishment of therapeutic alliances, needs to address a client's mistrust of having a provider from a different culture and insecurities about revealing personal information, such as status, in mainstream society. Family and community involvement, important to all persons receiving services, takes on added importance for less acculturated members of racial-ethnic groups who require supports from cultural group members who define their worlds.
Other components that were identified broaden established constructs. For example, communication competencies extend the notion of linguistic competencies, which require bilingual staff and use of interpreters (
18,
19), to a larger construct that covers styles of communication relevant to both non-English-speaking and English-speaking persons. Absent bilingual and bicultural staff, programs might consider using cultural brokers (
20), who speak a group's language and also understand its style of communication. Friendly milieus often cited in lists of cultural competence elements, in addition to objects in rooms and types of materials displayed, include physical space, furniture layout, and music—all features that can easily and inexpensively be put into place. The use of peers is widely endorsed, but here the emphasis is on peers from cultural groups because they can provide compassion and hope for recovery through the lens of the culture. Training materials can enhance cultural competence of staff, fostering compassion through sensitivity training, role playing with reversal of cultural roles, and analysis of situational scenarios and providing specific knowledge about the cultural groups served (
21).
As in most qualitative studies, conclusions drawn are limited by the small number of programs observed and may be biased by researchers' views. The study was not intended to provide evidence of the effectiveness of the studied programs or to examine organizational practices of the site as they affect consumers and programs. Both endeavors have different goals and would require different study designs.
Conclusions
The components we identified might serve as a starting point for administrators and staff seeking to evaluate and enhance programmatic cultural competence. Endorsement of these is in line with emerging views on mental health service delivery. By accounting for cultural influences, services are person centered; by stressing community integration, they are potentially recovery focused; and by promoting cultural strengths, they support the natural resiliencies within a cultural group. Use of these components in research studies is also suggested as a way of clarifying and making specific the action items of cultural competence. Further study is required to see whether the identified features when enacted in programs help to reduce disparities in the delivery of mental health care.
Acknowledgments and disclosures
The authors thank key facilitators at the sites, who, as well as making the study possible, provided guidance and insightful comments: at PASS, Neville Morris, M.B.A., Colin Dublin, M.B.A., and Nancy Sung Shelton, M.A.; at the Latino Treatment Program, Antonio Abad, M.D., and Annika Sweetland, L.M.S.W.; and at Hamilton-Madison House, Peter Yee, L.M.S.W., and Pei-Chen Hsu, Ph.D. The authors also thank Rachel Levenson for providing excellent editorial assistance. Ethel Davis Chambers, R.N., M.S., Jennifer Hernandez, M.P.A., and Brady Case, M.D., provided critical review of and commentary on the manuscript, which were much appreciated.
The authors report no competing interests.