About half of Europeans who need mental health services do not receive any kind of formal mental health care (
1). Even individuals with access to services do not necessarily utilize what evidence-based treatments are available. It has been suggested that aside from variables such as accessibility and quality of services (
2), low rates of help seeking can be explained by two factors—poor knowledge about mental illness and mental illness stigma.
Poor knowledge reduces care seeking presumably because individuals who do not recognize symptoms of mental illness and are unaware of available treatments are less likely to seek help (
3). On the other hand, individuals who develop a mental illness may decline to seek help to avoid the stigma commonly associated with mental illness (
4). There is growing evidence that stigma affects service use among people with mental illness (
5,
6). Survey studies of largely healthy individuals, on the other hand, found more mixed evidence. More perceived stigma was associated with less perceived need for help among younger, not older, U.S. university students (
7). In a German survey, desire for social distance from people with mental illness as well as anticipation of shame about treatment predicted lower help-seeking intentions (
8).
Instead of seeking treatment, many individuals decide to keep their mental illness a secret, a coping strategy that may avoid labeling and discrimination on some occasions but that is associated with poor long-term outcomes and social isolation (
9). Disclosure or “coming out,” on the other hand, though carrying the risk of discrimination, can be a successful strategy to cope with stigma (
10). Building on this body of research, we aimed to test the hypothesis that stronger intentions to seek help for and to disclose a mental illness are predicted by more positive attitudes and better knowledge about mental illness. We controlled for the level of contact with people with mental illness as a predictor of help seeking and disclosure because contact with people with mental illnesses typically reduces stigmatizing attitudes (
11).
Methods
Survey data from 1,751 adults across England were obtained in January 2009 from the Department of Health, U.K. (
www.dh.gov.uk/en/publicationsandstatistics/publications/publicationsstatistics/dh_100345). The data were based on answers to a set of survey questions about attitudes toward mental illness that were inserted by the department into an omnibus, that is, multipurpose, survey. The questions have been added periodically since 1993 and annually since 2007. The survey was carried out using a quota sample, with sample points selected by a random-location methodology. Census small area statistics and the postcode address file were used to define sample points, which were stratified by government office region and social grade, a demographic classification based on the occupation of the highest income earner in a household. Interviews were carried out in participants' homes by fully trained personnel using computer-assisted personal interviewing, and demographic information was collected at the end of the interview. Data were weighted for gender and social grade to match the general population, and sampling weights were used in the regression analyses. All the measures described below were completed during this survey.
One item assessed intention to seek help for a mental illness: “If you felt that you had a mental health problem, how likely would you be to go to your general practitioner for help?” Responses are rated on a Likert scale of 1 to 5, with higher scores indicating greater likelihood of seeking help. Help seeking from general practitioners was assessed because in the United Kingdom they are typically responsible for primary care of mental illnesses and act as gatekeepers to specialty care. The mean±SD score for the 1,751 adults was 4.2±1.1.
Whether participants felt comfortable disclosing a mental illness to friends or relatives was measured by another item: “In general, how comfortable would you feel talking to a friend or family member about your mental health, for example, telling them you have a mental health diagnosis and how it affects you?” Scores range from 1 to 7, with higher scores reflecting greater comfort to disclose. The mean±SD score for the 1,751 adults was 5.1±1.9.
The Department of Health Attitudes to Mental Illness Questionnaire was developed in 1993 based on previous research in Toronto and the West Midlands. It includes 26 items from the 40-item Community Attitudes toward the Mentally Ill (CAMI) (
12) scale and an added item on employment-related attitudes. [A table listing the 27 items is available in an online appendix to this report at ps.psychiatryonline.org.] Items refer to attitudes about social exclusion and feelings of benevolence, tolerance, and support toward community mental health care. Participants rate the 27 statements from 1, strongly disagree, to 5, strongly agree.
Knowledge about mental illness, available treatments, and recovery was assessed using the Mental Health Knowledge Schedule (MAKS) (
13). It includes six statements, such as “Medication can be an effective treatment for people with mental health problems.” Participants rate each statement from 1, strongly disagree, to 5, strongly agree, with higher scores indicating better knowledge. The mean±SD score for the 1,751 adults was 3.9±1.6 (Cronbach's
α=.61).
The extent to which individuals currently were in contact with people with mental illness as well as to what extent they had had contact in the past or intended to have contact in the future was measured with the Reported and Intended Behaviour Scale, or RIBS (
14). Its first subscale, past or present contact, includes four questions about having lived with or worked with someone with a mental illness or having had a neighbor or friend with a mental illness, either currently or in the past. Each item receives a score of 1, if the answer is “yes,” or 0, if the answer is “no” or “don't know.” Sum scores range from 0 to 4, with higher scores indicating more past or present contact. The mean±SD score was 1.0±1.2 (Kuder-Richardson formula 20=.60) for the 1,751 adults.
The RIBS second subscale uses four statements to measure intentions to have contact with someone with a mental illness (for example, “In the future, I would be willing to live with someone with a mental health problem”). Items are rated on a Likert scale, with 1 indicating strong disagreement and 5 indicating strong agreement. Higher average scores reflect stronger agreement. The mean±SD score for the 1,751 adults was 4.0±.9 (Cronbach's α=.83).
Results
A two-step factor analysis was used to identify internally consistent and replicable underlying attitude factors (see the online appendix at ps.psychiatryonline.org). First, we performed an exploratory factor analysis of the 27 attitude items in the 2009 Department of Health survey data and computed subscale scores for each factor, averaging those items that loaded highest on the respective factor. Only the two-factor solution yielded subscale scores with acceptable internal consistency, whereas three- and four-factor solutions produced subscale scores with poor consistency (Cronbach's α<.60). In the two-factor solution 14 items loaded on factor 1, prejudice and exclusion (mean±SD=2.2±.7, Cronbach's α=.83), and 13 items loaded on factor 2, tolerance and support for community care (mean±SD=4.0±.6, Cronbach's α=.77). Both subscales were conceptually meaningful and negatively correlated (r=−.51), accounting for a cumulative variance of 32.4%.
In a second step, we tested this two-factor model by conducting a confirmatory factor analysis of data from a 2008 Department of Health survey of 1,703 English adults who had responded to the same 27-item attitude questionnaire. For all items, critical ratios for regression weights were greater than 5 and significant (p<.001). Goodness of fit for the model (χ2=2,242.6, df=323, p<.001) was evaluated by the root mean square error of approximation (.059, 90% confidence interval=.057–.061). Again, both factors were negatively correlated (r=−.56). Thus the two-factor model derived from the 2009 survey data was confirmed in the independent 2008 data.
We examined correlations between the independent predictor variables knowledge (as determined by the MAKS), contact (as determined by the RIBS) and factors 1 (prejudice and exclusion), and 2 (tolerance and support for community care) (see table in the online appendix at
ps.psychiatryonline.org). Consistent moderate correlations were found between stronger attitudes of tolerance and support for community care and better knowledge about mental illness, more past and present contact with people with mental illness, and stronger intentions to have contact in the future. Similarly, attitudes of prejudice and exclusion were related to poorer knowledge and less current and past contact with an individual with a mental illness and less intention to have contact in the future. Better knowledge about mental illness was associated with more past and present contact and intended contact.
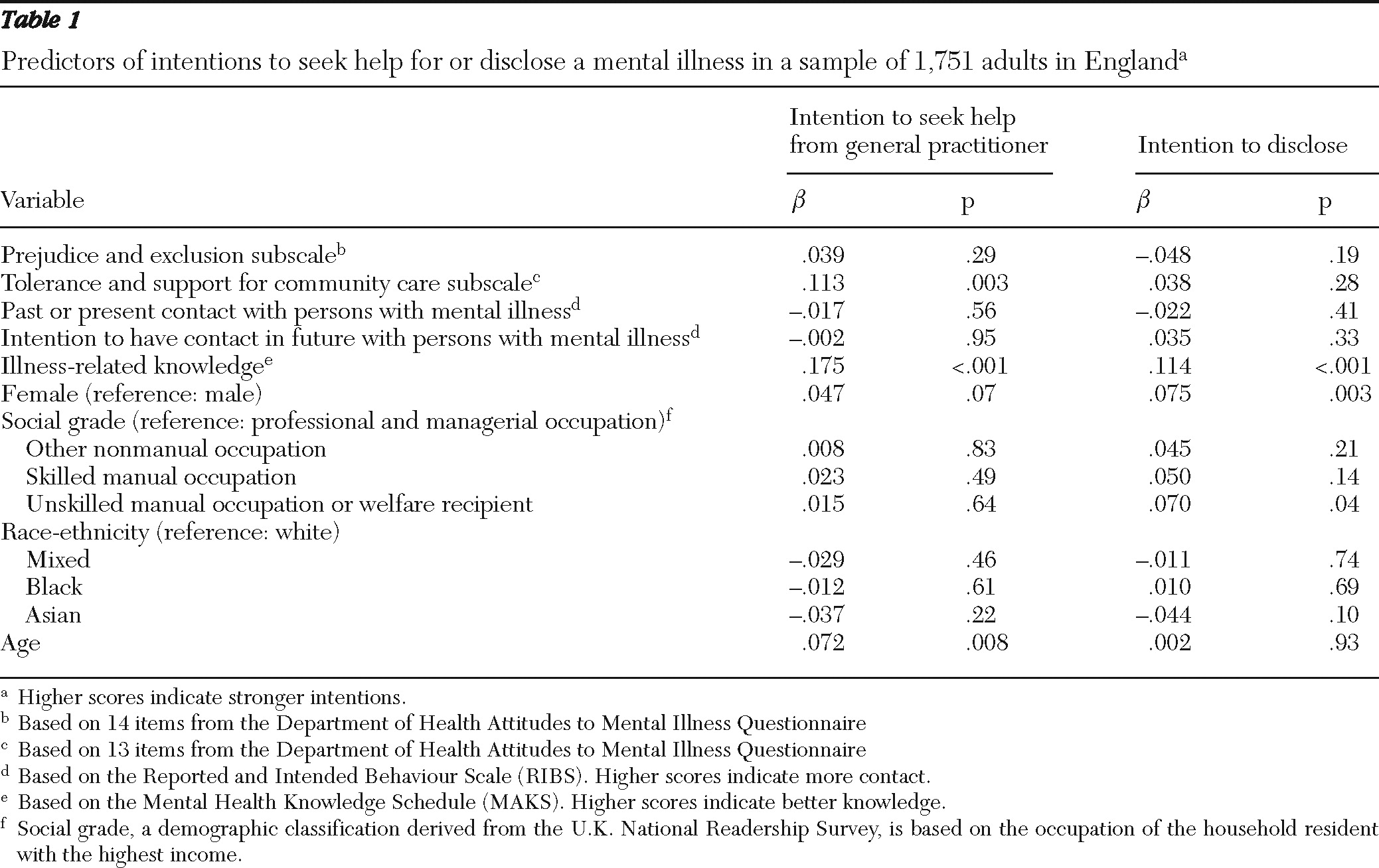
We ran linear regressions with sampling weights using Stata 10.1 to examine predictors of intentions to seek help for or disclose a mental illness (
Table 1). A stronger intention to seek help for a mental illness from a general practitioner was predicted by stronger attitudes of tolerance and support for community care, better knowledge about mental illness and available treatments, and older age (R
2=.07). The association between female gender and help seeking was nearly significant. Greater comfort with disclosing a mental illness to friends or relatives, on the other hand, was predicted by better knowledge but not by an attitude of tolerance and support for community care (R
2=.04). Disclosure was also associated with female gender and lower social grade. Asian ethnicity was related to decreased comfort with disclosure, but the trend was not statistically significant. Past or present contact with individuals with mental illness or intention to have future contact was not associated either with help-seeking intention or with comfort with disclosure.
Discussion
Based on a large representative survey of English adults, our study provides evidence that better knowledge about mental illness and available treatments as well as more positive attitudes of tolerance and support for community care predict stronger intentions to seek help and to disclose a mental illness to friends and relatives. It is a strength of this study that two important reactions to having a mental illness—help seeking and disclosure of one's mental health status—were examined in the same survey alongside the potential predictor variables of knowledge about mental illness, attitudes toward others with a mental illness, and the level of contact with other individuals with a mental illness.
Knowledge of mental illness and treatments was the strongest predictor of both help seeking and disclosure, a finding that underlines the role of mental health literacy in influencing reactions to developing a mental illness (
15). Longitudinal studies suggest that mental health literacy may be improved by public campaigns and that improved knowledge about antidepressants could lead to their increased use (
3,
4). Thus efforts to improve mental health literacy should be incorporated into future initiatives to increase care seeking, and their link with changes in behaviors such as help seeking and disclosure should be examined in greater depth.
Interestingly, the intention to seek help was associated with attitudes of tolerance and support for community care but not with stigmatizing attitudes of prejudice and exclusion. Previous research has focused on whether negative attitudes present barriers to service use, but our findings suggest that the presence of strong positive attitudes may be more relevant to help seeking and disclosure than the absence of negative attitudes. Current initiatives meant to reduce the impact of stigma might be better off focusing on strengthening positive attitudes, particularly support for community care.
We did not find evidence that the level of past or present contact with or expected contact with persons with mental illness was associated with intentions to seek help for or to disclose a mental illness. The impact of such contact on illness-related behaviors such as help seeking, however, could be mediated by stronger attitudes of tolerance and support for community care, as suggested by the positive correlation between the two in our study. Therefore, contact may not independently predict help seeking beyond the variance explained by positive attitudes.
Limitations of our study need to be considered. First, information on the level of psychopathology or distress among the survey participants as well as their previous contact with health services was unavailable. Second, only one example of help seeking was measured—consulting a general practitioner— and future studies should distinguish between various types of service use; likewise, the disclosure item did not differentiate between disclosure to friends versus disclosure to family. Future studies should also look at whether intentions to seek help for and to disclose a mental illness differ depending on whether the study asks about specific conditions such as depression or schizophrenia or uses the generic term “mental illness.” Fourth, it is unclear how closely intentions to seek help for or to disclose a mental illness are related to actual behavior. Finally, the variance explained by our regression models in the entire sample was small. It is therefore likely that other predictors of help seeking and disclosure, such as psychopathology, perceived quality and accessibility of services, experiences with health care, and—particularly as predictors of disclosure—personality variables such as rejection sensitivity and motivational goals, were not accounted for and should be studied further.
Conclusions
Our findings underline the role of knowledge and positive attitudes in help seeking and disclosure. Efforts to reduce stigma of mental illness, therefore, may wish to target these variables. Enhanced mental health literacy and positive attitudes toward seeking help in the community in society generally may lead to increased service use and less secrecy. Ultimately, the impact of mental illness stigma could be reduced and the situation of individuals with mental illness improved.
Acknowledgments and disclosures
Dr. Rüsch was supported by a Marie Curie Outgoing International Fellowship of the European Union. Dr. Evans-Lacko, Dr. Henderson, and Ms. Flach are supported by a grant to Time to Change from Big Lottery and Comic Relief and a grant from SHIFT. Dr. Henderson, Ms. Flach, and Dr. Thornicroft are funded by a National Institute for Health Research (NIHR) Applied Program grant awarded to the South London and Maudsley NHS Foundation Trust. Dr. Thornicroft is supported by the NIHR Specialist Mental Health Biomedical Research Centre at the Institute of Psychiatry, King's College London, and the South London and Maudsley NHS Foundation Trust. He has received grants for stigma-related research in the past five years from Lundbeck U.K. and from NIHR and has acted as a consultant to the U.K. Office of the Chief Scientist.