The research literature describes mental illness stigma in two forms. Public stigma pertains to negative social behaviors, reactions, and beliefs directed toward people with mental illness; self-stigma pertains to individuals with mental illness who accept prejudicial notions and internalize negative images that lower self-esteem (
1). Models of mental illness self-stigma have been developed from empirical investigations of adults. When adults experience self-stigma, the literature contends, the person with the mental illness accepts notions of stigmatizing images, which diminishes his or her self-esteem and reduces confidence in the future (
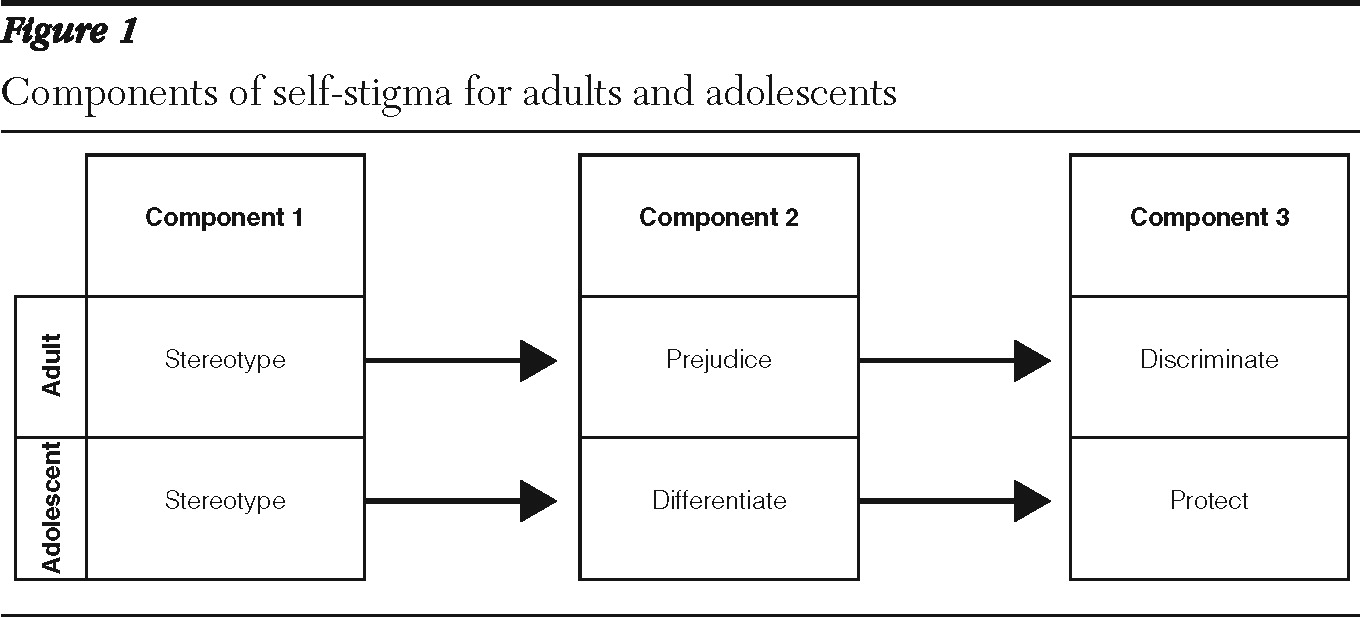
2). In particular, the most recognized adult self-stigma model suggests three components (
3). The first component is stereotype, wherein people with mental illness are exposed to negative beliefs about the self. The second component is prejudice; here the stigmatized individual agrees with the stereotype and emotionally internalizes it as a negative insult. The third component is discrimination and refers to the way the individual behaves in response to the prejudice (
3). These discriminatory acts could include isolation or social withdrawal.
Moreover, individuals who self-stigmatize have difficulty accepting a mental illness diagnosis (
1). For instance, through stereotyping, people with mental illness come to believe that their psychiatric disability makes them less valued. People who self-stigmatize react to the stereotype emotionally, by agreeing with the prejudice: “I am weak and unable to care for myself.” This agreement can cause low self-efficacy and low self-esteem (
1). In addition, internalized self-prejudice may lead to a decline in independent living or work behaviors. Disengagement can significantly affect a person's quality of life and career goals. Self-stigmatization, it is argued, makes individuals less willing to access services because of fears of prejudice and public discrimination (
1,
4).
The research on adult stigma documents its effects, which include secrecy, shame, and limiting interaction (
5). These effects negatively influence opportunities in employment, living situations, and intimate relationships (
1). Recent research (
6–
8) indicates that adolescents experience stigma's effects similarly to adults, with feelings of secrecy and shame and by limiting interaction. However, we do not know whether the self-stigma process for adolescents is similar to that of adults. There are plausible developmental reasons why youths might experience self-stigma differently. For example, adolescence is a nascent period of identity formation, engagement in peer relations, and use of the school environment as a site for developing a sense of self-esteem, independence, and self-efficacy (
9). In comparison, adults have variously mastered developmental tasks from infancy through adulthood, and therefore they can draw upon more refined developmental strengths than adolescents can; adults have realized some kind of identity integration and some kind of resolution among the various developmental conflicts (
10,
11). In contrast, youths have limited life experience with integration and identity resolutions, and because self-stigma processes affect core identity processes—attitudes and beliefs about the self—it is likely that, compared with adults, adolescents have a less consolidated identity to protect against, buffer, or neutralize stereotypes and prejudice.
The self-stigma models that exist explicate self-stigma among adults (
3). Minimal research has been conducted with adolescents (
12), and although one study found that youths did not report self-stigma effects (
13), no model has been constructed that represents self-stigma among adolescents with mental illness. Mental illness labels and medication use (
6) can assign an undesirable social status (
14) such as differentness (
15). Consequently, social exclusion may negatively affect identity formation for adolescents (
16,
17). Researchers found that most parents worried that diagnostic labels and medication use would cause others to view their children negatively (
18). And because peer acceptance is often adolescents' biggest concern (
16), youths emphatically do not want to feel different from others (
9,
15,
18,
19).
Furthermore, minimal work has examined how stigma affects utilization of mental health services among teens from minority groups (
7). Research shows that African-American adults can be reluctant to utilize mental health services because of mistrust of the system (
20), and these negative perceptions are often passed down to younger generations (
21). Compared with white adolescents, mistrust among African-American adolescents could intensify the effects of self-stigma.
Because self-stigma among adults has been shown to affect access and use of services (
1,
4), it is likely that it also affects adolescent access, engagement, and adherence to treatment (
22). Indeed, developing a self-stigma model could inform service providers of core issues that affect youth engagement and adherence to treatment. Qualitative studies of the experience of mental illness and medication use among adolescents can provide a close investigation of the processes of self-stigma (
23). Qualitative analysis of first-person narratives is invaluable, because it provides real lived experiences of how stigma affects individuals' lives, and these experiences can be used to develop interventions that are likely to be more efficacious and long lasting than previous interventions (
24).
Thus the primary aim of this qualitative study was to develop a model that can be useful to future research on the self-stigma process of adolescents, a critical and understudied area of research. How do youths construct self-stigma narratives? Are there differences by race? And is the self-stigma model for adolescents different from the self-stigma model for adults?
Methods
Through convenience sampling, the study recruited participants from an outpatient child and adolescent psychiatry unit of a university, from community mental health centers, and from an alternative high school for youths with social and emotional difficulties in a midsized Midwestern city. The protocol was reviewed and approved by the Institutional Review Board for Human Investigation. The sample (N=27) was drawn from a secondary data set (
25). The original data set included 40 participants; however, 13 narratives did not include sufficient data for the analytic plan used in this study.
Recruitment and interview procedures
Adolescents 12 to 17 years old who currently met DSM-IV criteria for a psychiatric illness and who had recently received a prescription for a psychotropic medication were eligible. The study focused on adolescents who were taking medications; thus adolescents were excluded from participation when their parents reported that their child had not taken psychiatric medication at least once in the past 30 days. Moreover, adolescents with a developmental disability (IQ lower than 70), a pervasive developmental disorder, a seizure disorder, or an organic brain disorder were not enrolled. Before study participation, the parents or guardians of the research participants provided written informed consent, and all adolescents provided written informed assent. The interviews were conducted in 2006–2007 and took approximately six hours each. Parents received $50 and adolescents $65 for their participation. Although guardians and parents were interviewed, this article reports on only the youths' data.
Interview instrument
A semistructured interview instrument, the Teen Subjective Experience Medication Interview (TeenSEMI), was used. The TeenSEMI was created by adapting an instrument designed to obtain medication and stigma data from adults with a diagnosis of schizophrenia (
25). The interview comprises 150 open-ended questions and contains questions in nine areas: diagnosis, illness, medication treatment, school, family, stigma, race-ethnicity, religion, and access to services. Two researchers pilot tested the TeenSEMI by observing one another's initial interviews, listening to the recordings, and then modifying questions to make them developmentally appropriate, more conversational, and less leading.
Data analytic strategy
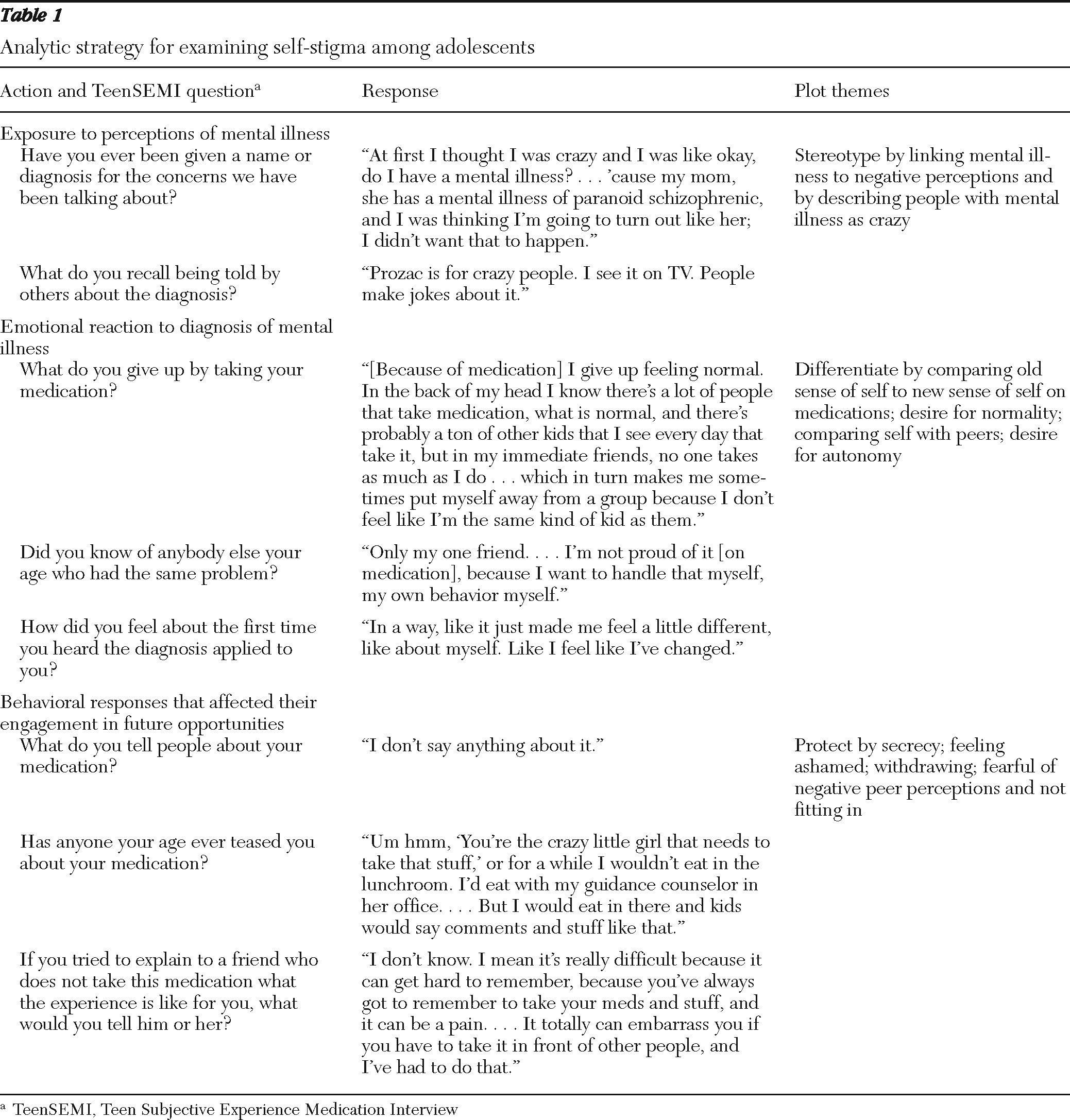
One objective of a qualitative narrative analysis is to focus on the plot components of a story (
26). A narrative structural analysis (
26) pays particular attention to how the narrator structures plot content—that is, how the story forms a whole and the specific plot components of the story. Here, plot is theorized to be the engine that pushes the story forward to some conclusion, much like in a murder mystery where clues motivate the reader to turn the page. Thus the illness and treatment narratives generated by the TeenSEMI were analyzed to identify the presence or absence of plot components that could be representative of self-stigma processes.
First, we conducted a thorough reading of each transcribed interview and used Atlas.ti software to select and code quotations that referred to stigma. The codes were created a priori by adopting from adult studies three stigma categories: exposure to perceptions of mental illness, emotional reaction to association with mental illness, and behavioral responses that affect engagement in future opportunities (
1). After coding the 27 narratives, we used the Atlas.ti hyperlink tool to connect the codes and quotations of each respondent to his or her stigma story. The result provided 27 condensed stories of self-stigma.
Each of the condensed stories was then read and coded for themes related to the three stigma categories: exposure, emotional reaction, and behavioral response. The themes were then grouped under a larger umbrella category, and this step led to three plot components: stereotype, differentiate, and protect. In addition, self-stigma stories were compared by race, gender, age, and type of disorder. To establish reliability, the second and third authors examined each narrative and used the constant comparative method (
27) to confirm that the plot components were consistently applied across the narratives (
27).
Results
The mean±SD age of the adolescents was 14.4±1.8. Females (N=18) constituted 67% of the sample, and males, 33% (N=9). Fifty-six percent of the participants were white (N=15), 37% were African American (N=10), and 7% were of other races and ethnicities. Twenty-six adolescents (96%) had received prescriptions for three or fewer medications, and only one adolescent had received a prescription for more than three. Over 74% (N=20) of the participants were diagnosed as having a mood disorder, and 56% (N=15) had a diagnosis of attention-deficit hyperactivity disorder; some participants had more than one mental condition.
The analytic strategy resulted in a self-stigma model that had three potential plot components: stereotype, differentiate, and protect (
Figure 1). Adolescents responded to their illness or use of medications by linking their personal meanings to stereotypes (
Table 1). For example, respondents said that people often refer to individuals with bipolar disorder as “crazy,” or they indicated that medications are for people who are “psycho.” In many cases, “crazy” and “psycho” people were described as acting bizarre or not fitting in because of their behavior or looks, consistent with stereotypes. Adolescents indicated in their narratives that statements about people with mental illness were often similar to ideas that they heard from family, peers, or the popular media.
In the second plot component, differentiate, adolescents acknowledged that the act of taking medication made them feel different from their peers: “I do not feel normal because of the medication.” By comparing themselves with peers who were not taking medication, they were focused on fitting in with their social environment. Concurrently, these adolescents became cognizant of how the medications and illness transformation affected their sense of self. Medications created, for some youths, a sense that their independent functioning was not of their own making. Furthermore, they wondered how their autonomy might be dependent on the medication (
16). Adolescents were reluctant to accept the “medicated” self-image, because it induced shame, especially when they perceived themselves to be different from peers, calling themselves “mental” or “cuckoo.”
Third, adolescents protected themselves from feelings of differentness by censoring their need for psychiatric medication; when socially interacting, they reported not wanting to be ostracized or humiliated for taking medication. Adolescents protected their self-image and reputation by covering up evidence or details that linked them to a mental illness. Some fabricated a nonpsychiatric use of medication, and others hid their medications. Overall, this plot component was about protecting a social connection with peers and holding onto hope for a bright future in school and beyond.
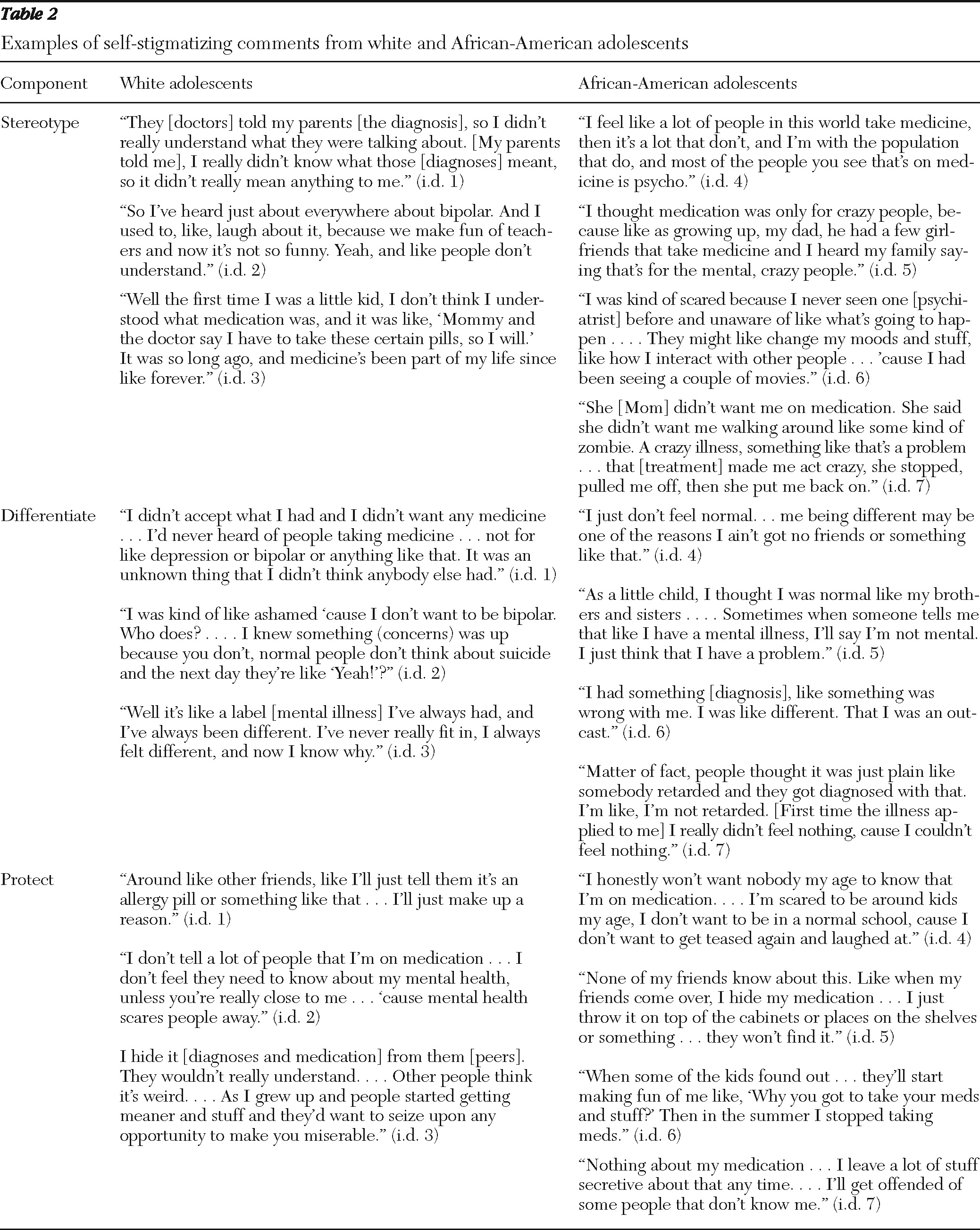
Comparison by race revealed that the African-American adolescents' differentiate and protect stigma plots contained responses very similar to those of white adolescents. As shown in
Table 2 both groups responded in ways that differentiated and protected them from negative views of medication and illness. “It was an unknown thing that I didn't think anybody else had” (white) and “I just didn't feel normal” (African American). And both groups protected themselves by keeping their medication secret: “Sometimes … I'll just tell them it's an allergy pill” (white) or “I honestly won't want nobody my age to know that I'm on medication” (African American).
However, African-American stereotypes were more negative than those of whites: “Most of the people you see that's on medicine is psycho,” “I heard my family saying that's for the mental, crazy people,” and, “She said she [Mom] didn't want me walking around like some kind of zombie.” In comparison, whites were less negative in tone: “I really didn't know what those [diagnoses] meant,” “And I used to, like, laugh about it [bipolar diagnosis] because we make fun of teachers and now it's not so funny,” and, “I don't think I understood what medication was.” Further, the statements suggest that African-American adolescents learn familial social norms that are passed down as they grow up that people who take medication are “psycho,” “mental,” or “crazy.” These messages from familial influences may play a key role in the mistrust discussed above.
In addition to a comparison by race, we also compared our sample on early, mid-, and later adolescence; type of disorder; and gender. Results are not shown because there were no differences. This may be due to the sample size and the exploratory nature of the research.
Some participants endorsed all three self-stigma plots (N=9), and some reported one (N=7) or two (N=8). For the analytic strategy of modeling self-stigma, it was not necessary for respondents to endorse all three. It is likely that individual and social circumstances mitigated one or more of the stigma plots. Instead of differentiate, for example, some adolescents reported that medication returned normalcy to their lives, and it helped them to function like peers. Or, some disclosed to others because their reserves of self-esteem protected them from feeling socially different.
Finally, we could delineate a process of self-stigma that had similarities to and differences from the self-stigma process (
3) that has been elucidated among adults (
Figure 1).
Discussion
This study provides several new findings that have implications related to stigma research. In contrast to previous research (
13), this study found several adolescent indicators of self-stigma: stereotype, differentiate, and protect. In addition, the findings suggest a stigma model that is different from the one for adults.
Peers, family, society, and the media often represent mental illness with negative stereotypes (
1). Exposure to negative images is like that in the adult model, yet the likely difference is the way an adolescent responds. For adolescents in general, peer acceptance is negotiated daily, and by late adolescence it should result in mastering feelings of loneliness, ostracism, and self-doubt. Arguably, where adolescents confront negative stereotypes, extra resilience may be necessary to neutralize internalized stereotypes that diminish their growing sense of identity. Thus illness onset in adulthood does not have this additional developmental context, and it therefore makes the self-stigma experience different from that of adolescents.
A second potential difference between adolescent and adult self-stigma is differentness and devaluation. In the emotional reaction to the association with mental illness, adults report feeling devalued (
3) (as a consequence of prejudice), whereas adolescents worry about being different. The model differences are likely a result of developmental issues. Adolescents, unlike adults, are not expected to have achieved a career objective, marriage, and home ownership, for example. Adults are less concerned about differentness from peers and more concerned about specific achievements; when socially acceptable goals have not been realized, adults can devalue themselves. Related is the possibility that medication poses unique challenges to adolescents; they might wonder, “Is it me or my meds?” (
16). The latter is more an identity concern, whereas for adults the concern is less about identity and more about how medication helps them acquire or achieve valued objects and social status.
In comparing adult and adolescent experiences of self-stigma, secrecy and limiting interaction were self-discriminating or protective mechanisms against feeling rejection and ostracism. However, it is likely that adults and adolescents have different beliefs about what they keep secret because they are at different stages in their lives and have different values about what constitutes achievement. Adults are secretive in order to keep jobs, social status, and perhaps significant relationships. Adolescents are protecting a developing sense of self, and, although psychologically their experience is similar to that of adults, there is a qualitative difference as to what is at stake. Keeping medications secret in order to protect oneself from social teasing and taunting is developmentally different from being secretive for fear of losing one's job.
Finally, the self-stigma comparisons by race led to findings worthy of discussion. Statements from African-American adolescents revealed greater negativity in stereotypes of people with mental illness, and many of these stereotypes were perpetuated by important relational figures, such as parents. Family norms such as these may lead African-American youths to use secrecy to a greater degree than whites to protect themselves.
Conclusions
A limitation of this study is that it excluded youths who had not taken medication in the past 30 days, which may have affected the findings. In addition, this qualitative study was not representative of all youths with diagnosed mental illness or of all youths taking psychiatric medications. Furthermore, comparing youths with mental illness who do and do not take medications would enable assessment of how medication might have an additive effect on stigma, particularly the feeling of differentness. Future studies with African-American adolescents and adolescents from other minority groups would help clarify how self-stigma stereotypes add to more intensive negative self-stigma processes and possibly contribute to nonadherence to psychiatric services. To validate the findings, longitudinal, mixed-methods designs are needed; such studies would include representative samples and repeated measures of development, quality of life, stigma from early to late adolescence, and effects of stigma on services.
Self-stigma is affected by developmental life experience. Adult self-stigma experience (
3) is associated with tasks of caring for the next generation (housing, career, and intimacy), and adolescent self-stigma is associated with autonomy (
9), peer perceptions (
16), and integration of various aspects of identity (
11). These developmental differences are the likely reasons that adult and adolescent self-stigma models differed. The strength of this study is the initial findings that identified how self-stigma among adolescents was related to development. These youths were already concerned with how their illness makes them different, and the impact of stigma on development could intensify the situation. Indeed, interventions targeted at developmental milestones are necessary to help youths with mental illnesses access psychiatric services and thrive.
Acknowledgments and disclosures
This project was supported by grant KMH068584A1 from the National Institute of Mental Health. The authors thank Jennifer Teller, Ph.D., for her comments on the manuscript.
The authors report no competing interests.