Studies have shown a gradual increase over the past decade in the number of children and adolescents with emotional and behavioral problems. Evidence pertaining to long-term safety and efficacy of psychotropic medication use by children is extremely limited, and age-appropriate dosing parameters still need to be established (
1,
2). However, there is little disagreement that use and cost of psychotropic medications among youths aged 18 and under have been steadily escalating (
3–
8). Health professionals and the public have raised concerns over a host of collateral problems associated with pediatric use of psychotropic medications, in particular use of medication combinations (concomitant use), long-term use, overprescription, and possible harm to development (
9–
13).
Prescription of benzodiazepines to children and adolescents is not as common as prescription to adults or elderly persons. However, community treatment data from Medicaid beneficiaries in U.S. health maintenance organizations indicated that an estimated 4.5–5.5 per 1,000 youths under age 20 received a prescription for an anxiolytic agent in 1996, a rate roughly two to three times higher than that in 1987; the increased rate was attributed largely to the growth in the prevalence of benzodiazepine use (
7). In France, analyses of 2004 national health insurance data indicated an annual prevalence of benzodiazepine use of roughly 6% among boys aged 15 to 18; the estimate for girls was 12% (
14). In the pediatric population, benzodiazepines are often considered a first-line agent in the treatment of epileptic seizures. In addition, benzodiazepines have been used for years to treat anxiety disorders and sleep problems and as adjuvant medications with neuroleptics for the treatment of psychosis (
15–
18). Accumulating clinical evidence suggests that potential adverse side effects of benzodiazepine use among pediatric patients include paradoxical reactions in acute treatment (such as agitation and talkativeness) as well as withdrawal symptoms and increased tolerance in long-term treatment (
19–
21).
Many studies have investigated problems associated with long-term benzodiazepine use. However, results have been derived from specific populations, such as elderly persons or individuals with substance use disorders (
22–
25). Studies of long-term use of benzodiazepines have virtually ignored patterns of use and associated factors among young people (
17). We used national medical and pharmacy claims data to examine the increasing prescription of benzodiazepines in the pediatric population in Taiwan. The study reported here used a retrospective design to identify the five-year trajectory of the pattern of benzodiazepine use among incident long-term benzodiazepine users aged 12 to 19 and to understand the extent to which factors at the level of the individual, service provider, and pharmacological agent may account for the emergence of trajectory patterns of benzodiazepine utilization from adolescence into young adulthood.
Methods
Data source
Our data came from the 1999–2005 National Health Insurance Research Database. The database was derived from the National Health Insurance Program—a universal health care program that was implemented in 1995 to provide medical care, dental services, preventive services, and prescription drugs to eligible residents in Taiwan. In this study, we used the unique encrypted identification number to link multiple data files, including the registry for beneficiaries, registry for contracted medical facilities, registry for drug prescriptions, ambulatory care expenditures by visits, and details of ambulatory care orders. The study was approved by the National Health Research Institutes Institutional Review Board.
Measures
Enrollee's category (EC), a proxy measure for socioeconomic status, was organized mostly by the job types of young enrollees' parents or primary caregivers. EC I indicates employment in government, government-run businesses, and public educational institutions; EC II indicates employment mainly in private enterprises; EC III indicates employment in agriculture, fishing, mining, or private educational institutions; and EC IV indicates employment in the military or persons with low incomes (
26). The country was divided into four regions to reflect different health care resources (northern, central, southern, and eastern), and the locations of enrollees' employment and residence were assigned accordingly. An urbanization index derived from five factors (population density, percentage of residents with a higher education [that is, polytechnic, junior college, college, university degree, or above], percentage over 65 years old, percentage employed in agriculture, and quality of health care resources) (
27) was used to regroup enrollees into three categories: urban, suburban, and rural areas. Enrollees' history of neurological and mental disorders in calendar year 2000 were retrieved from the primary and secondary diagnoses in outpatient service records and defined according to
ICD-9-CM categories (psychoses, codes 295.XX–298.XX; neurotic disorders, codes 300.XX; and epilepsy, codes 345.XX).
Medical institutions where young enrollees received benzodiazepine prescriptions in 2000 were categorized into medical centers only, district hospitals only, local hospitals or clinics only, and “mixed” on the basis of the classification of Hospital Accreditation in Taiwan (
28,
29). The classification of specialties prescribing benzodiazepines included neurology only, pediatrics only, psychiatry only, either two or three of these specialties (“mixed”), and specialties other than neurology, pediatrics, and psychiatry (“others”).
A total of 26 pharmacological agents were included in the broad category of benzodiazepines: alprazolam, bromazepam, brotizolam, chlordiazepoxide, clobazam, clonazepam, clorazepate, cloxazolam, diazepam, estazolam, fludiazepam, flunitrazepam, flurazepam, lorazepam, lormetazepam, medazepam, midazolam, nimetazepam, nitrazepam, nordazepam, oxazepam, oxazolam, prazepam, triazolam, and two Z-hypnotics (zolpidem and zopiclone). According to regulations of Taiwan's Food and Drug Administration (FDA), benzodiazepine use for a period exceeding four weeks is generally not recommended; therefore, the definition used in this study for long-term benzodiazepine use was receipt of a benzodiazepine prescription for 31 or more cumulative days in any given calendar year (
30). Moreover, as indicated by the Anatomical Therapeutic Chemical (ATC) classification system, the 26 benzodiazepine agents were further classified on the basis of their half-life (short, less than 20 hours; long, 20 hours or more) and indications (anxiolytics and hypnotics) (
31). Benzodiazepine dose was indexed by the average daily dose, which was calculated as total doses divided by number of prescription days in 2000.
In 1999 the benzodiazepine use rate for youths aged 11 to 18 was 6.7%. To reduce possible reverse causation between long-term benzodiazepine use and factors at the prescriber- and pharmacological agent-levels, we restricted the analyses to youths who had not received any benzodiazepines in calendar year 1999 (1,292,929 youths aged 11 to 14 and 1,660,568 aged 15 to 18) and identified so-called incident benzodiazepine cases in 2000.
Analyses
Chi square tests were used to examine the distribution of benzodiazepine prescriptions in 2000 by individual characteristics, attributes of the service provider, and attributes of the pharmacological agent, with stratification by age group. Initial inspection of the variable number of benzodiazepine prescription days among the incident long-term benzodiazepine users suggested an asymmetric distribution that was skewed to the left (that is, a nonnormal distribution); thus for subsequent analyses we regrouped number of benzodiazepine prescription days in any given year from 2001 to 2005 into eight groups defined by event numbers: 0 (no days), 1 (1–30 days), 2 (31–60 days), 3 (61–90 days), 4 (91–120 days), 5 (121–150 days), 6 (151–180 days), and 7 (≥181 days).
Group-based trajectory analyses with a general quasi-Newton method in the zero-inflated Poisson (ZIP) distribution were then performed to identify possible trajectory groups of long-term benzodiazepine use. The probabilities of event number (that is, 0, 1, 2, … 7) in each calendar year during the five-year period were estimated with ZIP distribution. The optimal number of groups and the best model were selected via model fit indices (Bayesian information criterion) and the size of the smallest group to summarize distinctive features of benzodiazepine prescription (
32–
34). [A description of how the four-group model was selected is available in an online appendix to this article at
ps.psychiatryonline.org.]
Building on the trajectory groups assigned by the posterior probability derived from the best trajectory model, polytomous logistic regression analyses were performed to estimate the risk associations, indexed by adjusted odds ratio (AORs) and 95% confidence intervals (CIs). All analyses were performed with the SAS Proc traj and Proc logistic procedures (SAS, version 9.2).
Results
Incidence rates were estimated for 2000 in the two groups of nonusers of benzodiazepines in 1999. For the 1,292,929 youths aged 11 to 14, the rate was 4.3%, and for the 1,660,568 youths aged 15 to 18 the rate was 6.3%.
Table 1 presents data on selected characteristics of incident short- and long-term benzodiazepine users aged 12 to 19 in calendar year 2000. Only 3.2% of the incident users aged 12 to 15 (N=1,758) and 5% of those aged 16 to 19 (N=5,265) received a benzodiazepine prescription for more than 30 days (long-term use).
As
Table 1 shows, the short- and long-term user groups differed significantly on several variables related to patient, service provider, and medication characteristics. For example, in both age groups a greater proportion of long-term users than short-term users received a prescription from the psychiatry only specialty (ages 12–15, 21.1% versus 1.4%; ages 16–19, 24.3% versus 2.2%) and from the mixed specialty group (ages 12–15, 27.2% versus 1.4%; ages 16–19, 26.8% versus 1.8%). Similarly, a greater proportion of the long-term users had received prescriptions for benzodiazepines in mixed forms (half-life variable) (ages 12–15, 30.9% versus 5.2%; ages 16–19, 34.6% versus 7.1%) and for mixed indications (ages 12–15, 27.2% versus 1.2%; ages 16–19, 35.3% versus 2.5%) and had taken multiple agents (three or more) (ages 12–15, 29.3% versus 1.0%; ages 16–19, 35.8% versus 1.8%)
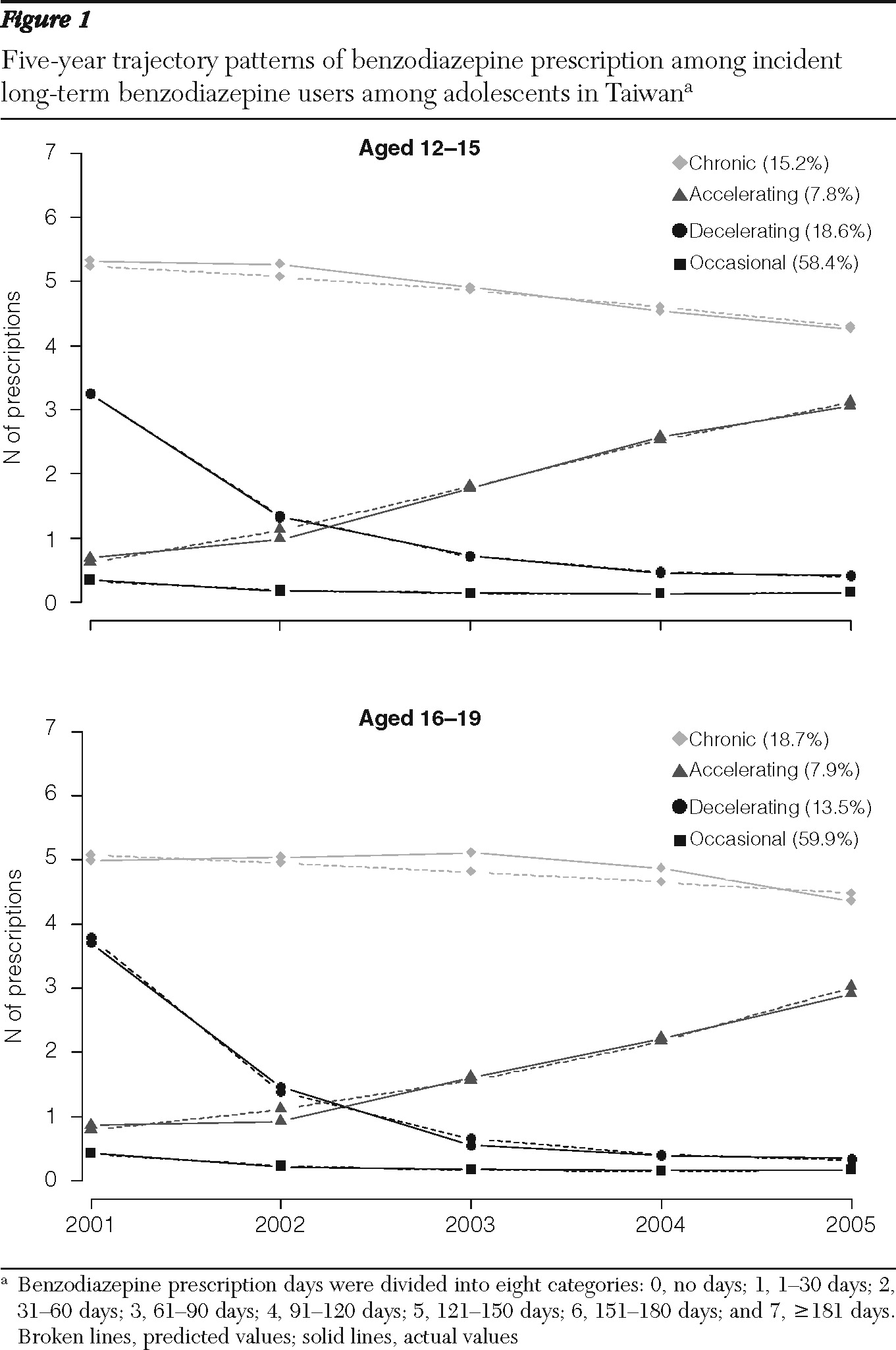
Among the 1,758 long-term users aged 12–15, four trajectory groups of benzodiazepine prescription utilization were identified (
Figure 1, upper panel): occasional users, 58.4% (received less than 30 days of benzodiazepine prescription annually for the five-year period); decelerating users, 18.6% (average prescription days declined gradually from 120 to 30 days); accelerating users, 7.8% (average prescription days increased gradually from 30 to 120 days); and chronic users, 15.2% (annual receipt of benzodiazepines was consistently for 120 to 150 days for the five-year period). Four trajectory groups also emerged among the 5,265 long-term users aged 16–19 (
Figure 1, lower panel). However, the proportions were significantly different from those observed in the younger group (p<.001). For example, the proportion of chronic users was higher in the older group (18.7% versus 15.2%).
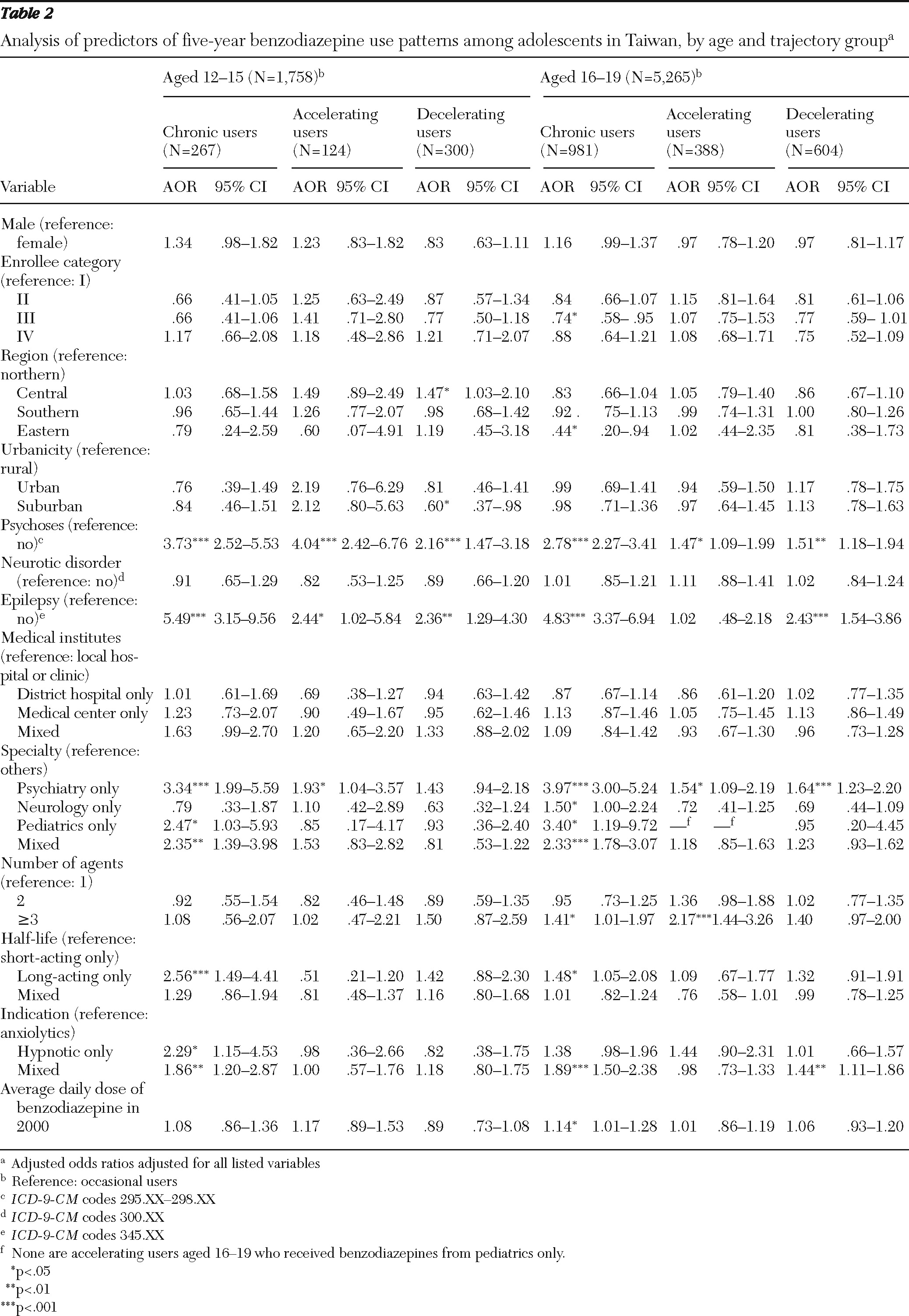
Analyses of baseline variables as predictors of five-year trajectories of benzodiazepine use are shown in
Table 2. After adjusting for all listed factors, we found that youths with epileptic disorders were five times more likely than those without these disorders to become chronic users as they grew older. In early adolescence, a diagnosis of psychosis was associated with a fourfold greater risk of increased benzodiazepine prescription days (accelerating use) (p<.001); in late adolescence, this diagnosis was associated with a 1.5-fold higher risk of accelerating use (p<.05).
In both age groups, receipt of a benzodiazepine prescription from a psychiatrist was associated with a three- to fourfold increased risk of developing chronic use over the five-year period; receipt of a benzodiazepine prescription from a professional in the mixed specialty group was associated with an approximate twofold higher risk of developing chronic use. Youths who received prescriptions for only long-acting benzodiazepines at baseline had a consistently two to three times greater likelihood of developing chronic benzodiazepine use in early adolescence than those who did not receive such prescriptions. A higher average dose at baseline was associated with an increased risk of chronic use in late adolescence.
Preliminary cross-tabulation analyses of benzodiazepine half-life and medical specialty found that long-term users tended to receive benzodiazepines with a long half-life from pediatricians only, especially among youths aged 12 to 15. Because of the potential correlation between specialty and the prescription of long- and short-acting half-life benzodiazepines, we repeated the analyses in
Table 2 with stratification by specialty (data not shown). In these analyses, the excess risk of chronic use associated with receipt of long-acting benzodiazepines only compared with receipt of short-acting only remained significant only for the specialties of pediatrics (12–15 years, AOR=23.27, CI=2.68–202.05; 16–19 years, AOR=20.0, CI=1.42–282.45) and neurology (12–15 years, AOR=9.71, CI=1.90–49.62; 16–19 years, AOR=3.93, CI=1.97–7.82). For the psychiatry specialty, the AORs were 1.48 (CI=.57–3.83) for chronic use by the younger group and 1.45 (CI=.85–2.46) for chronic use by the older group.
Discussion
This analysis of medical claims data for individuals aged 12–19 in Taiwan had several important findings. First, long-term benzodiazepine use was not uncommon in this age group—from 3% to 5% of these youths developed long-term benzodiazepine use within a year of the initial prescription. Second, among long-term users, four distinct trajectory groups emerged over five years: occasional, decelerating, accelerating, and chronic users (120–150 days annually for five consecutive years). Roughly a quarter of the long-term users became accelerating or chronic users over the course of adolescence. Third, among the patient characteristics that predicted patterns of long-term use, having a history of certain health problems (namely, psychosis or epilepsy) was the most salient. Among service provider attributes, the type of medical specialty, but not the type of medical institution, had significant differential affects on youths' subsequent benzodiazepine use. Among factors at the level of the pharmacological agent, receipt of benzodiazepines with a long half-life or with mixed indications appeared to be associated with a two- to threefold increase risk of developing chronic benzodiazepine use.
Some limitations should be considered in interpreting the results. First, the analyses relied primarily on data from use of pharmacological services reimbursed by Taiwan's National Health Insurance program. Therefore, benzodiazepines obtained from illegal sources or paid for out of pocket were not included. Thus the analysis may have underestimated the actual number of prescription days for any calendar year between 1999 and 2005. However, we expect that this underestimation is minimal because most of the study population was under age 18, with limited dispensable income. In addition, the definition of long-term benzodiazepine use focused exclusively on prescription days (the sum of prescription days for each benzodiazepine dispensed in the same calendar year). Therefore, among adolescents with the same number of prescription days, we may not have been able to distinguish between intensive long-term users who were receiving multiple benzodiazepine prescriptions within a short period of time and those who used benzodiazepines periodically across a one-year span. Moreover, our data provided limited information about illness severity, clinical decision making, choice of agents, and frequency of administration (that is, regular versus PRN use). Finally, our findings may not generalize to other populations for which health insurance policies, health care systems, or benzodiazepine indication profiles differ from those in Taiwan. Future work that integrates measures of continuity and overlap for each prescription may help us to overcome this issue and to examine in more detail the role of overprescription in youths' subsequent risk of long-term benzodiazepine use.
Notwithstanding these limitations, the study has strengths, most of which are attributable to the robust nature of the national health insurance data on pharmacological service use, without which this type of investigation would be impossible. To our knowledge, no previous research has longitudinally investigated the trajectory patterns of benzodiazepine use in a pediatric population. In addition, the large sample of young benzodiazepine users provided an important opportunity to evaluate the effects of a wide range of factors at the level of the individual, service provider, and pharmacological agent on the stability of or change in benzodiazepine use.
Consistent with previous research (
23,
35), we found that incident long-term benzodiazepine use was disproportionately greater among youths with medical conditions or mental illness. Furthermore, a diagnosis of psychosis or epilepsy was a modest predictor of subsequent chronic or accelerating benzodiazepine use. For years, clinical practitioners and researchers have raised concerns about negative consequences associated with long-term benzodiazepine use among persons with serious mental illness or neurological problems. For instance, a study of patients with epilepsy attending university hospitals in Greece indicated that use of benzodiazepines was significantly associated with reduced quality of life and that the reduction was particularly salient in the domains of social and cognitive functioning (
36). Given the high prevalence of concomitant medication use among persons with epilepsy (
17,
37), regular monitoring of benzodiazepine-related behavioral side effects and possible drug-drug interactions is especially essential for youths (
9).
Previous research has suggested an association between the specialty of psychiatry and a greater likelihood of chronic use of benzodiazepines. A cross-sectional study of pharmacy records from health maintenance organizations in Washington State showed that patients who received prescriptions of benzodiazepines from psychiatrists had a twofold higher risk than those whose prescriptions were from primary care providers of daily benzodiazepine use for 60 days or more (
38). Our finding that receipt of a benzodiazepine prescription from the psychiatry specialty at baseline was associated with accelerating or chronic benzodiazepine use may suggest variations in the health conditions and disease profiles of youths seen by psychiatrists. Patients who receive prescriptions for benzodiazepines should be monitored on a regular basis for adverse effects, treatment adherence, and possible drug-drug interactions (
9); the need for repeat (or refill) prescriptions, particularly for long-acting benzodiazepines and benzodiazepine-like drugs, should be reassessed at regular intervals.
The study also found that more than a quarter of long-term users had benzodiazepine prescriptions from two or more specialties, and 40% received prescriptions from specialties other than psychiatry, neurology, or pediatrics, suggesting that the risk of long-term benzodiazepine use and associated problems may arise for young patients who seek medical care from multiple specialties and from other sources. Clinicians prescribing psychotropic medications to adolescents should guard against long-term use and polypharmacy by checking whether patients have received benzodiazepines from multiple doctors for various medical conditions. Research that provides a better understanding of youths who are long-term benzodiazepine users may lead to the development of strategies to reduce long-term use and related negative consequences, such as prescription shopping (
39).
Pharmacological attributes have often been linked to differential risk of chronic or long-term use (
23,
38,
40). One such study of 13,500 community-dwelling residents over eight years in the Netherlands showed that initial benzodiazepine use with a hypnotic indication was associated with a two- to threefold greater risk of subsequent prolonged use compared with use of an agent with an anxiolytic indication (
25). Also, in contrast to previous studies of medication half-life in adult and elderly populations (
23,
41), our study found that among long-term pediatric users of benzodiazepines, initial receipt of long-acting agents was associated with a two- to threefold increase in subsequent risk of chronic use. The observed differences may partly be explained by possible heterogeneity in definitions of long-term use, age composition of study samples, attributes of long-term benzodiazepine users (such as disease profiles), and length of follow-up (
40). Further research is needed to delineate the complex relationship between individual characteristics (such as age and gender) and pharmacological attributes (such as half-life and indication) on change in and stability of benzodiazepine use.
Finally, although the direction and magnitude of associations linking factors at the individual, service provider, and pharmacological agent levels with the trajectory patterns were similar across the two age groups, some features in the risk profile warrant greater attention. For instance, the increased risk of chronic or accelerating benzodiazepine use associated with receipt of multiple benzodiazepines appeared to apply only to older adolescents in the transition to young adulthood. In contrast, the psychosis-related excess risk of chronic or accelerating benzodiazepine use was more salient among young adolescents. Taken together, our findings illustrate the importance of recognizing possible developmental variation when creating a pharmacological treatment plan for pediatric patients. Larger longitudinal studies can also help to elucidate possible complex interactions over the life course between having a medical condition and mental illness and use of psychotropic medications and associated adverse effects.