Despite schizophrenia's low prevalence in the general population (
1), its overall impact on society is staggering when one considers its economic burden (
2–
4) and the human suffering it inflicts on patients and their families. There is no cure, at present, for this brain disorder, but a number of treatment options are available, aimed at managing symptoms, improving quality of life, and preventing relapse and rehospitalization (
5).
Pharmacotherapy using antipsychotic medications is an important part of today's treatment programs for individuals with schizophrenia. Treatment guidelines clearly identify these drugs, particularly the newer second-generation antipsychotics, as first-line therapy for schizophrenic disorders and bipolar disorders (
5–
11). Antipsychotics are also used to treat other conditions, including the behavioral and psychological symptoms associated with dementia and depression (
12). Overall use of these drugs in many countries has markedly increased, fueled largely by the use of second-generation antipsychotics (
13,
14).
Evidence of ethnic disparities in the utilization of antipsychotic medications was first reported in the 1990s, a few years after the introduction of second-generation antipsychotics on the market. A study from that period showed that although no significant differences in treatment rates were observed, African Americans were found to be more likely than their non-Latino white counterparts to be given higher doses of first-generation antipsychotics (
15). More recent studies show that further disparities have emerged with the introduction of more expensive but widely used second-generation antipsychotics. These later studies showed that African Americans were less likely to receive second-generation antipsychotics (
16–
24) but more likely to receive first-generation antipsychotics (
16,
17) compared with non-Latino whites. Similarly, some studies reported that compared with non-Latino whites, Latinos have a lower likelihood of using second-generation antipsychotics (
18,
25).
Although evidence of ethnic disparities in the use of antipsychotic medication has grown over the past few years, there remains a paucity of information regarding differences in use across other ethnic groups, including East Asian, South Asian, and Southeast Asian populations. This lack of understanding could pose challenges to mental health systems that plan and provide services for these fast-growing ethnocultural groups, which now account for 5% and 11% of the U.S. and Canadian populations, respectively (
26,
27).
To help address this gap we conducted this study of ethnic disparities in the use of antipsychotic drugs in British Columbia, Canada. Using linked survey and administrative data, we examined whether the likelihood of using antipsychotic drugs differed significantly across ethnic groups and whether these differences persisted after analyses controlled for some observable patient characteristics, including possible indications for treatment. Because of the composition of its population, British Columbia is an ideal location to study the use of antipsychotic medications by persons of Asian heritage in a North American setting.
In many instances, disparities in the use of antipsychotic medications are indicative of poor-quality care because the mismatch between need and appropriate care often leads to important differences in mental health outcomes. Findings from this study should prompt planners and providers of mental health care to closely examine current practices and structures that may contribute to disparities in use.
Methods
Study sample
We performed a cross-sectional retrospective study using both survey and administrative data. We created our study sample by pooling samples from the 2001, 2003, and 2005 cycles of the Canadian Community Health Survey (CCHS). These interviewer-administered surveys collect health-related data from individuals ages 12 years and older from community-dwelling households selected by Statistics Canada based on complex multistage sampling designs (
28). All linkable CCHS respondents from British Columbia (N=30,062) were included in the study sample.
We linked individual ethnicity data from CCHS to administrative health databases that include all residents of British Columbia except those whose health care is under federal jurisdiction (approximately 4% of the total population): registered status Indians (aboriginals), veterans, federal penitentiary inmates, and members of the Royal Canadian Mounted Police. To minimize bias arising from the use of incomplete administrative data, we excluded individuals who self-identified as aboriginal and those who identified as white and aboriginal as well as those who did not reside in the province for at least 275 days (
29). We also excluded individuals who were less than 12 years old at the beginning of 2005 and those with missing data on ethnicity, sex, place of residence, or income. [A figure showing the sample selection process is available as an online supplement to this article at
ps.psychiatryonline.org.] Analysis of missing data showed no disproportionate concentration of cases with missing data on sex, place of residence, or income across ethnicities.
All health and sociodemographic data except income were obtained from administrative data sets from 2005; for income, we used 2004 data sets. Data were provided from Population Data BC (
30) with the permission of the British Columbia Ministry of Health Services (BC-MoHS) and the British Columbia College of Pharmacists. Ethics approval was obtained from the Behavioral Research Ethics Board at the University of British Columbia.
Measures and data sources
Our outcome measure was a dichotomous variable indicating whether or not an individual filled at least one prescription for any antipsychotic drug in calendar year 2005. Prescription data were obtained from PharmaNet, a centralized database maintained by the BC-MoHS that records every prescription filled in community pharmacies throughout the province regardless of patient age or insurance status. We used the World Health Organization's Anatomical Therapeutic Chemical (ATC) classification system (
31) to identify the first- and second-generation antipsychotics filled by individuals included in the study.
We derived our ethnicity variable from responses to the CCHS question “People living in Canada come from many different cultural and racial backgrounds. Are you?” We coded respondents who self-identified with more than one of the 13 ethnic categories as persons of mixed ethnicity. Respondents who identified with just one ethnic group were coded into the following categories according to their response: white, Chinese, other Asian, and nonwhite non-Asian. We originally intended to derive a number of Asian ethnic groups, but our sample yielded only two that were statistically viable: Chinese and other Asians. We included in the category of other Asians those who self-identified as Filipino, Japanese, Korean, East Indian, Pakistani, Sri Lankan, Cambodian, Indonesian, Laotian, and Vietnamese. The nonwhite non-Asian category included Arabs, blacks, Latinos, Afghanis, and Iranians. We also used CCHS data to flag as recent immigrants those who immigrated to Canada in 1996 or later. Ethnicity and recent immigration status were the only two variables we derived from pooled CCHS data.
Using the 2005 diagnostic codes available in the administrative records of physician and hospital visits (obtained from the British Columbia Medical Services Plan database, where one physician visit equals one diagnosis, and from the British Columbia Discharge Abstract Database, where a recorded hospital stay can have up to 25 diagnoses), we constructed aggregated diagnostic groups (ADGs) according to the Johns Hopkins Adjusted Clinical Groups Case-Mix system (
32). We used a count of ADGs as our general health status covariate. A higher count of ADGs is associated with a greater degree of overall clinical complexity and increased likelihood of prescription drug use (
33).
Similarly, we used physician and hospital records to construct indicators of schizophrenia, bipolar disorders, depression, and dementia diagnoses. These variables were binary measures that indicated whether individuals received at least one diagnosis of a mental disorder or dementia (
34) in 2005. The specific
ICD-9 diagnostic codes we looked for in the records of physician visits were 295 for schizophrenic disorders; 296 (excluding 296.2, 296.3 and 296.9) for bipolar disorders; 311, 296.2, 296.3, 296.9, and 50B (a British Columbia-specific diagnostic code used for “anxiety/depression”) for depressive disorders; and, 290, 294, 298, 331, and 348 for dementia. In hospital visit records, we looked for the following
ICD-10 diagnostic codes: F20 for schizophrenia, F30 and F31 for bipolar disorders, F32–F34 and F38–F39 for depressive disorders, and F00–F03 for dementia.
Using 2005 administrative data, we adjusted for sociodemographic characteristics, including age (in ten-year bands) and place of residence (urban versus nonurban). We controlled for income using 2004 household income quintiles built with a combination of household-specific and neighborhood-level income data (
35). We used British Columbia's geographic regions (referred to as local health areas) to create variables indicating urban and nonurban residence.
Statistical analysis
To test for statistically significant differences across ethnic groups with respect to the covariates we examined, we performed chi square tests on categorical variables (such as sex and diagnosis) and analysis of variance (ANOVA) with Bonferroni post hoc comparisons on continuous variables (including age, income, and number of ADGs).
Using logistic regression, we modeled the association between antipsychotic drug use and ethnicity, controlling for the effects of sex, age, urban residence, recent immigrant status, income, overall health status, and clinical indications for antipsychotic medication for our entire cohort. We ran two regression models to determine whether ethnic variations in antipsychotic use differed by type of diagnosis. Our first model examined whether antipsychotic drug use differed by ethnicity and controlled for schizophrenia or bipolar disorder diagnosis and health and sociodemographic variables. The second model, built on the first, added depression and dementia diagnoses. To test the robustness of our findings, we ran these models again using a subgroup of individuals who had at least one of the mental disorder or dementia diagnoses we described earlier.
We also attempted to run two separate analyses: one for the subgroup of individuals with one or more diagnoses of schizophrenia or bipolar disorder and another for those without these diagnoses; however, the small sample of persons in the schizophrenia or bipolar disorder stratum prevented these stratified models from running or obtaining statistically reliable results.
All statistical analyses were completed with version 10.1 of Stata for Linux64.
Results
Description of the sample and antipsychotic drug use
A total of 27,658 individuals met our inclusion criteria for this study. [A figure showing the study sample selection is available as a supplement to this article at
ps.psychiatryonline.org.]
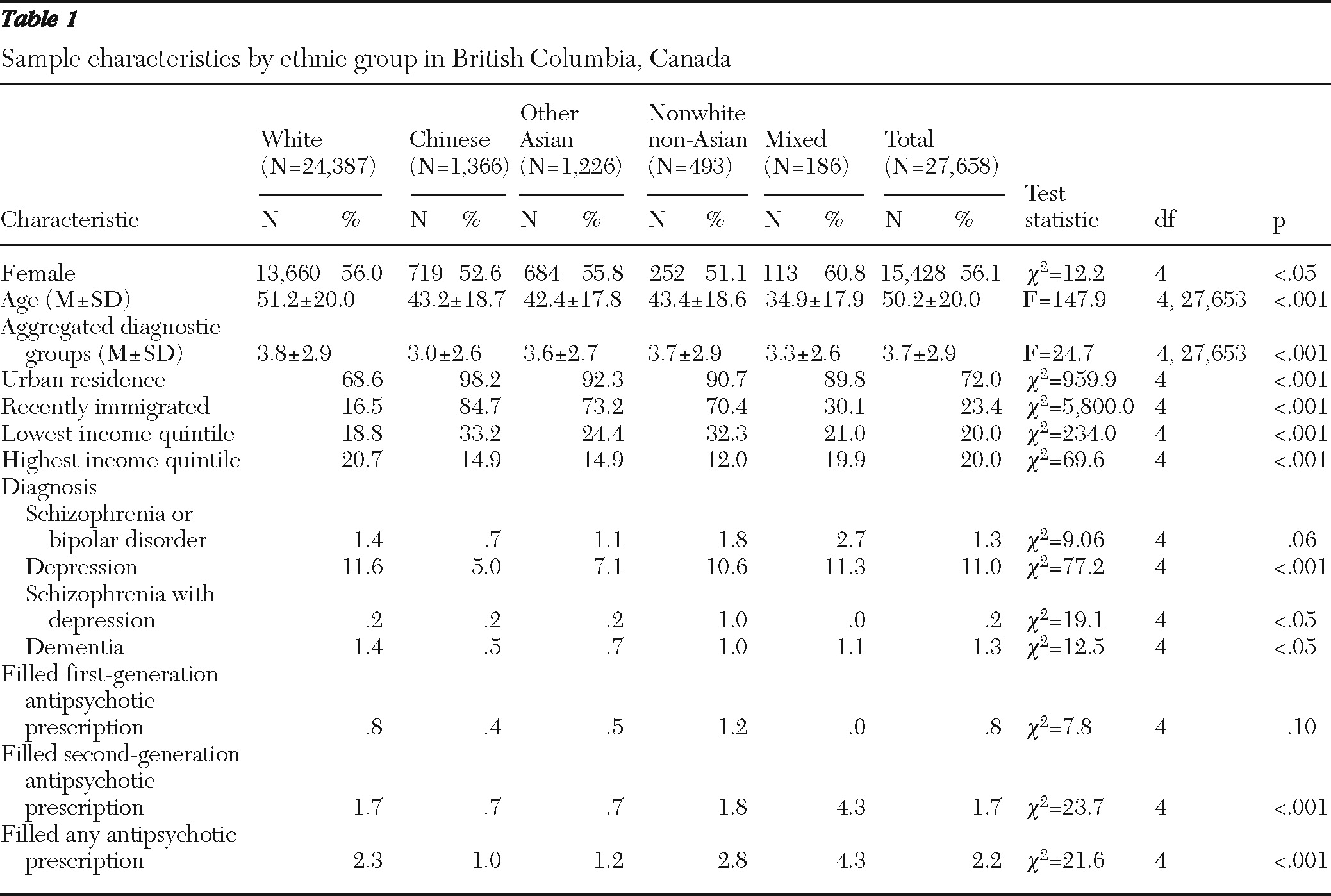
Table 1 describes our final sample according to ethnic groups. Chi square test and ANOVA results indicate statistically significant differences across ethnic groups for all the covariates we examined, except for the diagnoses of schizophrenia or bipolar disorders and the proportion of individuals that filled a first-generation antipsychotic.
In comparison with other single-ethnicity groups, those self-identifying as white were approximately ten years older, had a slightly higher mean number of ADGs, were more likely to live in nonurban areas, were less likely to be recent immigrants, and were more likely to be in the top income quintile. In comparison with others from minority groups, those identifying as Chinese had slightly fewer ADGs and were more likely to live in urban areas, to have recently immigrated, and to be from households with lower income.
The distribution and concentration of diagnoses also differed by ethnicity. The highest prevalence of depression (11.6%) and dementia (1.4%) diagnoses were found among those who self-identified as white. The highest prevalence of diagnoses for schizophrenia or bipolar disorder (2.7%) was found among respondents in the mixed ethnic group. Those who self-identified as Chinese had the lowest prevalence of diagnoses for depression (5.0%), dementia (.5%), and schizophrenia or bipolar disorders (.7%).
Ethnic differences in antipsychotic prescription fills
In 2005, 2.2% of the individuals in our sample filled at least one antipsychotic prescription. Without adjustment for other factors, individuals in our sample who self-identified as Chinese (1.0%) were least likely to fill a prescription for antipsychotics, whereas individuals of mixed ethnicity (4.3%) were most likely to do so (see
Table 1).
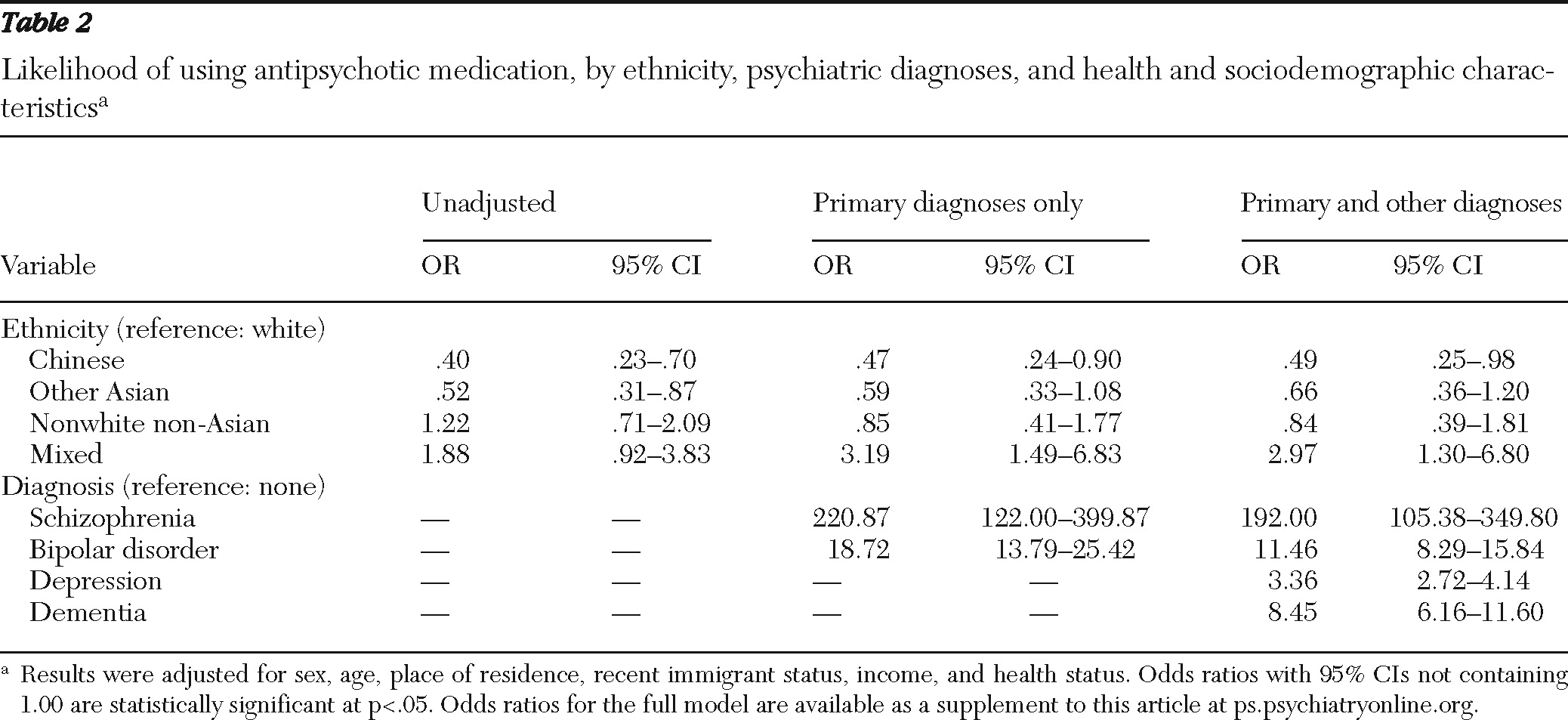
Table 2 presents the results of the two adjusted logistic regression models examining differences in antipsychotic drug use by ethnicity. In the model that controlled for schizophrenia and bipolar disorders, significant ethnic differences in use of antipsychotic medication remained after adjustment for individuals' sex, age, place of residence, immigrant status, income, health status, and primary diagnoses. Persons identifying as Chinese had much lower odds than those identifying as white of filling a prescription for an antipsychotic (odds ratio [OR]=.47, p<.05). In contrast, those identifying as being of mixed ethnicity were more likely than whites to have filled antipsychotic prescriptions (OR=3.19, p<.05).
When we ran the second model, which also controlled for depression and dementia, all of the ORs moved slightly toward 1.00, except for the nonwhite non-Asian category. Statistically significant differences were found among Chinese (OR=.49, p<.05) and mixed ethnic groups (OR=2.97, p<.05), indicating that disparities persisted in this more fully adjusted model. Although they were not significant, the point estimates for the other Asian and nonwhite non-Asian groups suggested lower odds of purchasing antipsychotics for these groups compared with whites. [Odds ratios for the full model are available as a supplement to this article at
ps.psychiatryonline.org.]
Results from the subgroup analyses based on a sample of individuals who had a diagnosis of either a mental disorder or dementia (N=3,445) produced findings mirroring full population results (results available by request).
Discussion
Using linked survey and administrative data, our study investigated ethnic differences in the use of antipsychotic drugs across ethnic groups that had not been studied. Results suggest that ethnic disparities in use persisted even after we accounted for important sources of variation, such as sex, age, recent immigration, income, health status, and diagnoses of schizophrenia or bipolar disorder. Chinese and other Asians were less likely to fill antipsychotic prescriptions compared with whites, and these disparities decreased slightly after analyses further controlled for dementia and depression diagnoses. Conversely, people of mixed ethnicity were significantly more likely than whites to use antipsychotic medication, and this difference remained, although it decreased slightly, after the model was adjusted to fully account for all the diagnoses examined.
Our finding of lower likelihood of antipsychotic drug use among Chinese and other Asian people compared with whites is consistent with the existing literature on the use of mental health services in general and medication use among patients with serious mental illness. It has been reported, for instance, that even after adjustment for differences in the prevalence of major depressive disorders, Chinese, South Asian, and Southeast Asians living in Canada were less likely than white Canadians to have sought care for their condition (
36). Similarly, Chinese immigrants in Canada diagnosed as having a serious mental illness were found to have received fewer psychiatric drugs than an equivalent comparison group drawn from the general population (
37). Our findings also complement the existing literature on ethnic disparities in antipsychotic drug utilization by including Asians in the list of ethnic minorities that were found to have lower levels of use (
16–
24).
One potential reason for the lower likelihood of filling antipsychotic prescriptions among Chinese is cultural differences in views on Western medicine (
38). Although we accounted for some measure of acculturation by controlling for recent immigration status, it remains possible that many Chinese patients maintained strong negative views toward the use of antipsychotic medications to treat mental disorders. It is also possible that the lower odds of filling reflect cases of nonadherence in 2005 resulting from unpleasant experience with medication in previous years. Compared with whites, Chinese patients have been reported to respond to significantly lower doses of antipsychotics (
39). If clinicians inadvertently did not take into account this information when determining dosage levels, their Chinese patients may experience more adverse events, consequently affecting their adherence to the prescription regimen.
We were unable to adequately explain the higher likelihood of antipsychotic use observed among people of mixed ethnicity. In our data, these individuals were predominantly young women from lower income groups with unusually high rates of diagnoses of schizophrenia or bipolar disorder and depression. Even though they had particularly high rates of diagnoses of conditions for which antipsychotics would be prescribed, it may also be the case that a greater share of this population uses antipsychotics for conditions we did not control for, such as attention deficit disorder, autism, or substance use disorders (
40). However, to our knowledge there is no literature suggesting that Canadians of mixed ethnicity are more prone to other psychological disorders or clinical conditions that would be treated with these medications.
This study was not without limitations. Our data captured only filled prescriptions, and filled prescriptions do not equal written prescriptions or antipsychotic drug consumption. Individuals may have been prescribed these medications but never filled them or filled these prescriptions but never actually took the medications. However, given the seriousness of the main diagnosis for which these medications are used, misclassification of prescribing practices is likely to have been small. Furthermore, because individuals with untreated schizophrenia often end up in hospitals, which leads to the resumption of pharmacotherapy, filled but not consumed prescriptions are also likely to have been minimal in this drug class. Also, although our linkage of three cycles of CCHS data to administrative records produced a sample with a higher percentage of persons from ethnic minorities than CCHS samples used in other analyses (
41), our final sample still underrepresented ethnic minority populations in British Columbia compared with census data (
29). Our income data were also from 2004, whereas all the other health administrative data we used were from 2005. It is possible that the ORs we calculated for income were biased, but we believe that the effect was negligible because incomes at the population level are fairly stable within short periods of time.
Conclusions
Our study provides evidence of significant disparities in the use of antipsychotic medication in a population that has a large representation of Asian ethnicities. We found that Asians, specifically Chinese, were less likely than whites to use antipsychotic drugs, whereas people of mixed ethnicities were more likely to use them. These differences persisted even when sociodemographic characteristics, health status, and clinical indications for the drugs' use were accounted for. In addition, disparities were greater when antipsychotic drugs appeared to have been used in treating conditions other than schizophrenia and bipolar disorder. Future studies may be directed toward examining whether these differences are provider or patient driven and in determining how these variations result in meaningful differences in mental health outcomes. Planners and providers of mental health care may need to take into account differences in cultural beliefs and practices as well as group differences in pharmacological response to antipsychotic medications to ensure that patients from ethnic minority groups are receiving care appropriate to their level of need.
Acknowledgments and disclosures
This study was funded by an operating grant (“Equity in Pharmacare: The Effects of Ethnicity and Policy in British Columbia”) from the Canadian Institutes of Health Research. The construction of the research database was supported, in part, by contributions of the BC-MoHS to the University of British Columbia Centre for Health Services and Policy Research. Mr. Puyat was supported in part by a Western Regional Training Centre studentship funded by Canadian Health Services Research Foundation, Alberta Heritage Foundation for Medical Research, and Canadian Institutes of Health Research (CIHR). Dr. Hanley was supported by CIHR and the Michael Smith Foundation for Health Research (MSFHR). Dr. Law receives salary support through a New Investigator Award from CIHR. Dr. Wong was supported by a scholar award from MSFHR and a New Investigator award from CIHR. Sponsors had no role in the project or in decisions to publish results.
The authors report no competing interests.