Persons from racial-ethnic minority groups have disproportionately poor mental health status, experience more barriers to and receive lower quality mental health care, and are underrepresented in mental health research (
1,
2 ). The relatively lower socioeconomic status of most racial-ethnic minority groups explains some variation—that is, persons from racial-ethnic minority groups are more likely to be uninsured or underinsured, to be less educated and have lower income, and to reside in areas where medical services are less available (
3,
4 ). Moreover, persons from racial-ethnic minority groups may be more distrustful of health care providers, have lower health literacy, be less likely to seek care, and prefer fewer services (
5,
6 ). Nonetheless, disparities persist even after controlling for such factors. Some of this variation is likely due to differences based on race-ethnicity in physician-patient interactions (
7,
8,
9,
10 ).
Race-ethnicity has been shown to influence physician-patient communication during clinical encounters and physician decision making (
10,
11 ). Physicians tend to view patients from minority groups as less intelligent, less effective communicators, less compliant, more likely to abuse alcohol and drugs, and less likable than white patients (
8,
12 ). Although distressing, these facts are consistent with social categorization (or social cognition) theory (
10,
12 ). This theory, originating in the social psychology literature, posits that humans use categorization to make vast amounts of social information manageable. Characteristics are unconsciously assigned to social groups (for example, racial-ethnic groups), and those characteristics are then unconsciously applied to individuals through stereotyping (
13 ). Physicians may be especially vulnerable to stereotyping because of time pressures and the need to make rapid assessments—that is, physicians have more social information to process, so rely more heavily on social categorization (
14 ).
Social categorization and racial-ethnic stereotyping likely influence physician behavior and decision making. However, because these are unconscious processes, physicians may be unaware of them and may underestimate their own contributions to racial-ethnic disparities. Understandably, physicians may be reluctant to explore their unconscious biases; it would be difficult for most physicians, who have dedicated their careers to helping others, to confront their own contributions to racial-ethnic inequality (
10 ). Nonetheless, attempts to eliminate disparities will not be successful as long as health care providers believe that the sources of disparities are entirely external to themselves. Physicians must become aware of their own unconscious biases in order to change the behaviors that contribute to racial-ethnic inequalities.
We hypothesized that there are several prerequisites for changing physician behavior: physicians must be aware that racial-ethnic disparities exist, physicians must believe that they may contribute to disparities, and physicians must be motivated to change their behavior. The purpose of this study was to evaluate the extent to which psychiatrists have achieved these prerequisites and to identify factors that are associated with achievement of each.
Methods
Study sample
Data were collected through an online survey of American Psychiatric Association (APA) members conducted from April 2006 to August 2006. The survey was also distributed at the APA's Institute on Psychiatric Services in October 2006. For the online portion of the study, names and addresses of 2,000 randomly selected member psychiatrists were purchased from the APA. A letter of introduction and unique access code were mailed to each; a printed survey was available. A maximum of three contact attempts were made. Of the 2,000 individuals identified, a correct address could not be obtained for 24 and seven were retired or deceased. Of the final sample of 1,969 eligible members, 186 psychiatrists (9%) completed the survey online.
Surveys were also distributed from an exhibit hall booth at the 58th Institute on Psychiatric Services, a national professional conference. Respondents were compensated with a $5 specialty coffee gift card. Of the 190 psychiatrists who completed the survey at the conference, two had previously participated, and only their responses to the online survey were used. The final sample for this study was 374 individuals.
The University of Rochester Research Subjects Review Board reviewed this study and determined that it was exempt from institutional review board review.
Survey
Content of our survey was informed by a survey developed by the Kaiser Family Foundation (
15 ) that was subsequently modified by Lurie and colleagues (
16 ) for use with cardiologists. The survey included questions about familiarity with racial disparities research, perceived awareness of psychiatrists about racial disparities, and changes in awareness over the past decade. To measure perceived determinants of quality of care, physicians rated the extent to which 12 patient factors (including race) affect quality of psychiatric care, both in general and in their own practice setting. A "difference" variable was calculated by subtracting the perceived influence of race in the participant's practice from the perceived influence of race in general. Finally, respondents were asked whether they had participated in the past year in any program designed to reduce racial disparities in health care or whether they would be interested in participating in such a program; they were also asked whether they believed such programs were likely to reduce health disparities. Most items were measured on 5-point Likert scales. Key terms, such as quality of care, were defined.
Sociodemographic variables included gender, race, ethnicity, years in practice, practice setting and size, proportion of patient population that is non-Hispanic white (referred to as "white" in this article) versus other (referred to as "nonwhite" in this article), and number of professional meetings attended annually. A copy of the survey is available on request.
Analyses
Univariate statistics were generated for all variables in the data set. Most data were treated as categorical, and most bivariate analyses were conducted with chi square analysis or Fisher's exact test, as appropriate. Multivariate analyses were conducted using logistic regression. Analyses were guided by a priori hypotheses to limit type II error, and they were conducted using two-sided tests with α =.05. Analyses were performed using SAS, version 9.1.
Results
Participants
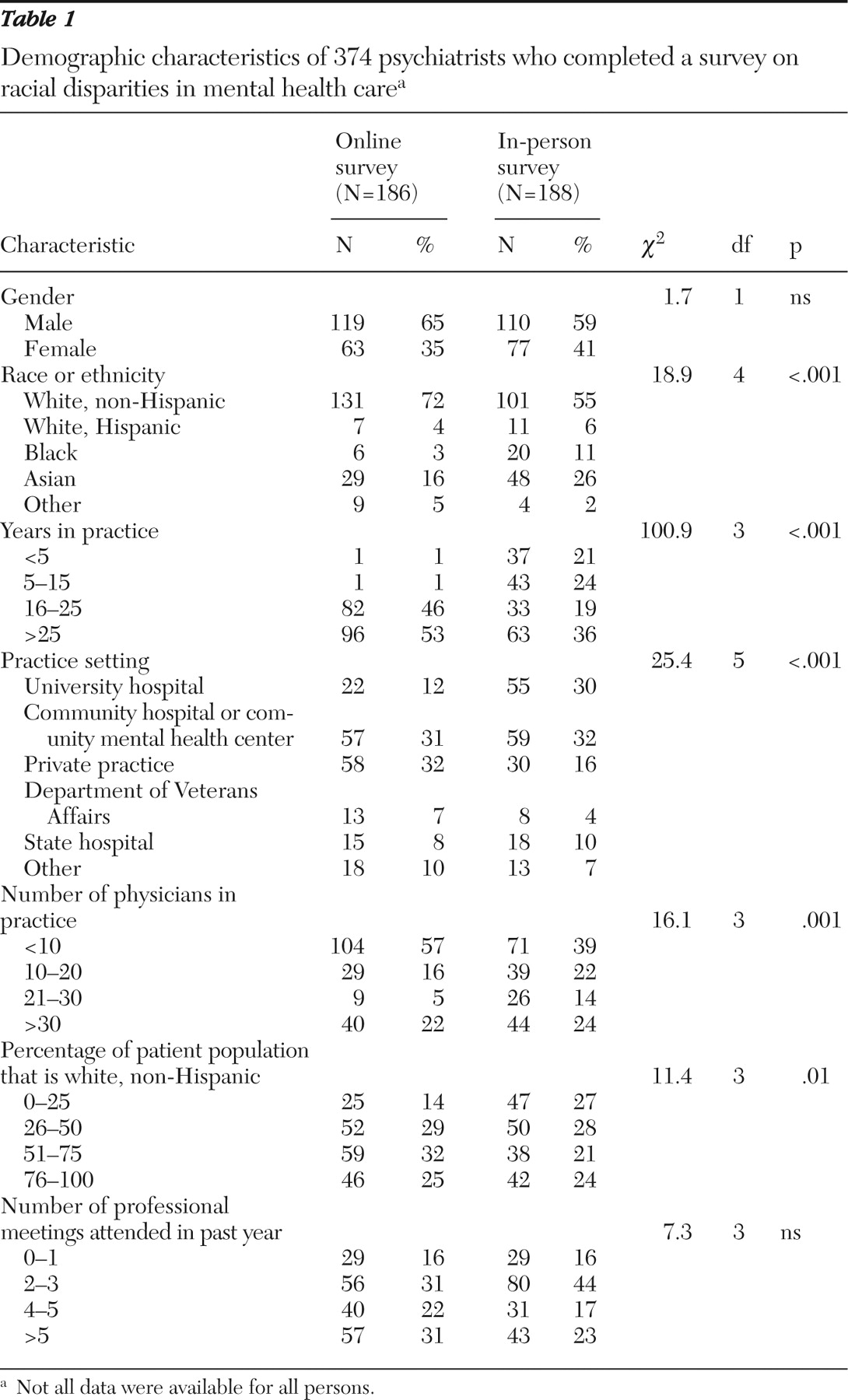
As shown in
Table 1, most participants were male (62%) and white (63%). Most (77%) had been in practice for 15 years or more, and almost half (48%) worked in small practices (less than ten physicians). Almost one-third of participants (32%) worked in community hospitals or community mental health centers (CMHCs), and most others worked in university hospitals (21%) or private practice (24%). The racial-ethnic makeup of respondents' patient populations varied widely, but in many respondents' practices (48%), at least half of the patients were from racial-ethnic minority groups.
Awareness of disparities
Most respondents were not at all or a bit familiar with research on racial inequalities in psychiatric care (N=190 of 370, 51%), and approximately one-third of respondents were moderately familiar (N=136 of 370, 37%), and only 12% were familiar or very familiar (N=44 of 370). Compared with their respective comparison groups, respondents were more likely to be familiar or very familiar with this research if they were nonwhite ( χ 2 =6.9, df=2, p=.03) or if they treated a greater proportion of patients from minority groups ( χ 2 =6.9, df=2, p=.03). Those who attended more professional meetings annually also reported greater familiarity ( χ 2 =18.0, df=6, p=.006). Familiarity was not associated with the physician's gender, practice setting, or years in practice.
A majority of respondents believed that, compared with ten years ago, there is somewhat more or much more awareness of racial inequalities in psychiatric care among psychiatrists in general (N=272 of 368, 74%). Less than one-fifth of respondents felt that awareness has remained the same (N=69 of 368, 19%), and only 7% (N=27 of 368) felt that awareness has decreased. Most felt that psychiatrists, compared with other types of physicians, are more aware of racial disparities in health care. Specifically, 275 of 365 respondents (75%) believed that psychiatrists are somewhat or much more aware than physicians in other fields, whereas 64 of 365 respondents (18%) felt that psychiatrists are no more or less aware. Only 26 of 365 (7%) felt that psychiatrists are somewhat or much less aware than physicians in other fields.
Beliefs about disparities
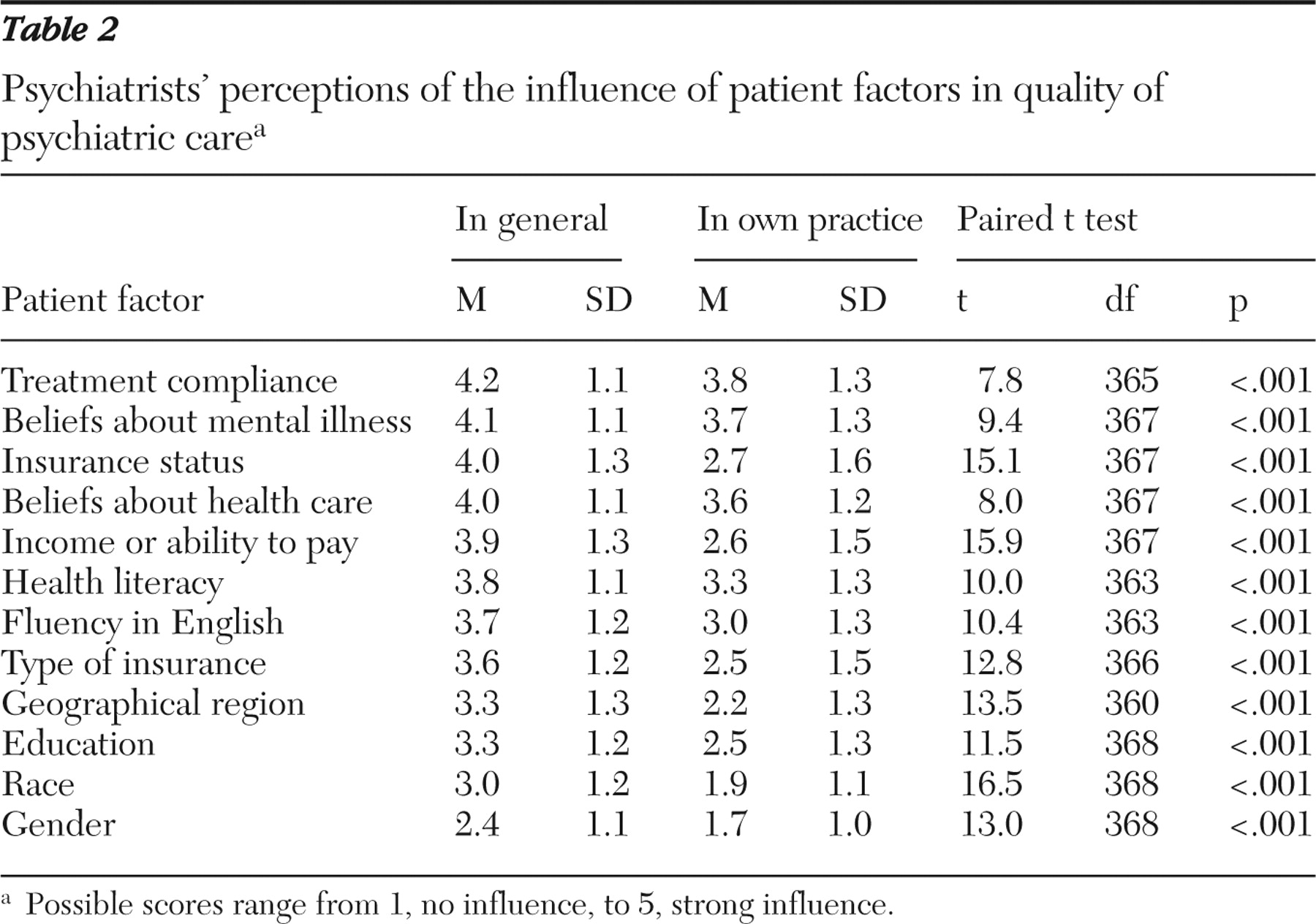
When asked to rate the effect of 12 patient factors on quality of psychiatric care, respondents generally reported that race has less of an impact on quality than other factors, both in general and in the respondents' own practices (
Table 2 ). In both scenarios, only gender was rated as having less influence on quality of care.
For every patient factor, participants believed overall that the factor has a stronger influence on quality of care in general than on quality of care in their own practices (p<.001 for all). In regard to race, 222 of 369 respondents (60%) believed that race has a stronger influence on quality of care in general than in their own practices, whereas 127 of 369 respondents (34%) believed that race is equally influential in both instances. Only 20 of 369 respondents (5%) said that race has more of an influence on quality of care in their own practices than on quality of care in general.
Most white respondents (N=165 of 227, 73%) believed that race has more influence on quality of care outside of their practice than within it, whereas nonwhite respondents were more likely to perceive that patient race is equally influential in both settings (N=65 of 130, 50%; χ 2 =32.3, df=2, p<.001). Those who had been in practice longer also tended to believe that race has more influence on quality of care in general than in their own practices (p<.001, by Fisher's exact test). Respondents were more likely to believe that race has a stronger influence on quality of care in general than in their own practices if they attended the fewest professional meetings annually (no meetings or one meeting) (N=37 of 58, 64%) or the most meetings (more than five) (N=64 of 96, 67%), compared with those who attended two to three meetings (N=76 of 132, 58%) or four or five meetings (N=42 of 70, 60%) (p<.001 by Fisher's exact test). Gender, practice setting, proportion of the respondent's patient population that is white, and familiarity with racial disparities research were not associated with whether the respondent perceived a different influence of race in general and in the respondent's own practice.
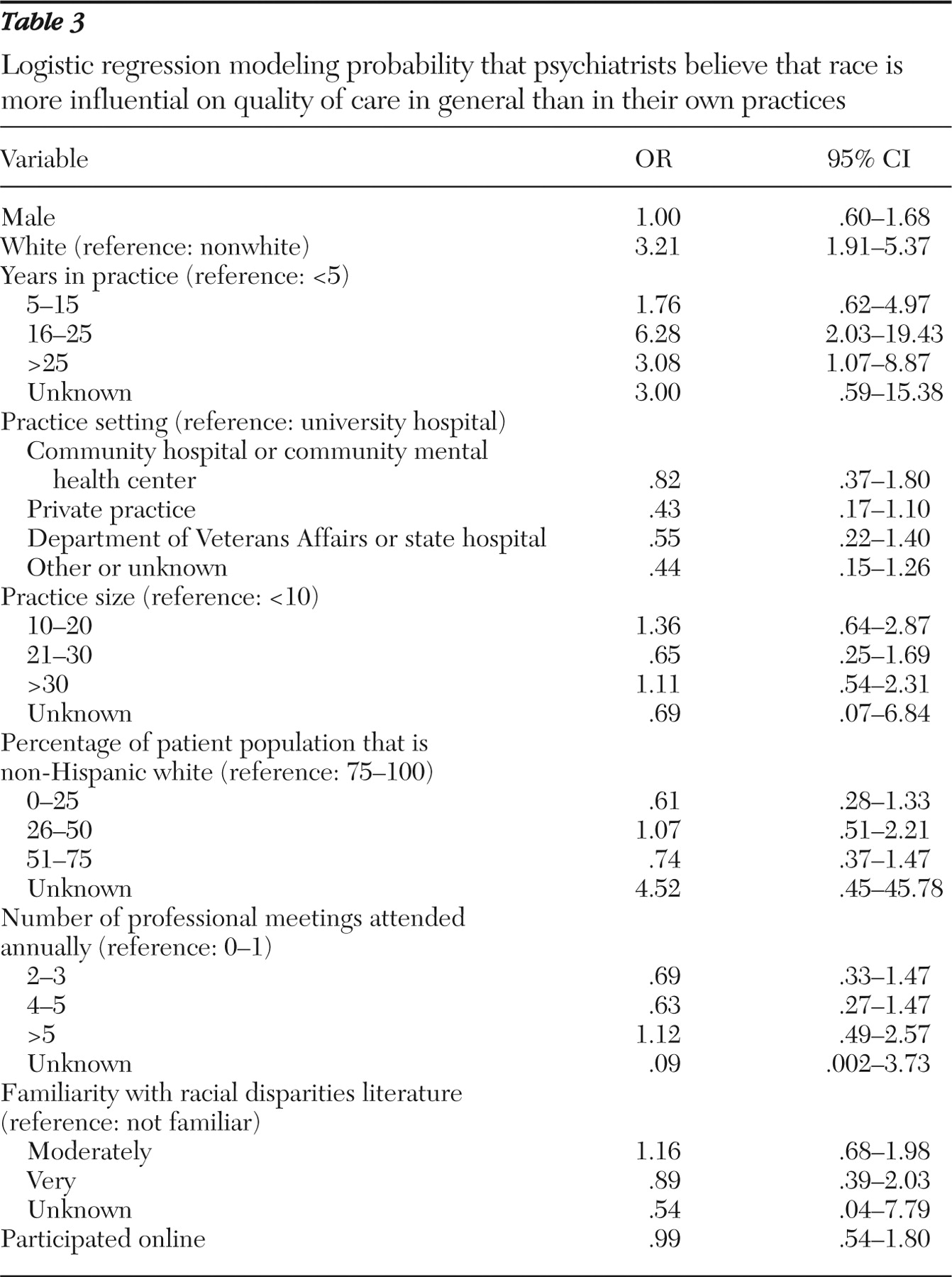
Logistic regression was used to model the likelihood that a respondent believed that race is more influential on quality of care in general than in the respondent's own practice. After the analysis controlled for covariates, the only variables that were significantly associated with belief were the respondent's race and length of time in practice (
Table 3 ). Compared with nonwhite respondents, white respondents were more likely to feel that race is more influential in quality of care generally than in their own practice. Additionally, respondents who had been in practice for more than 15 years were more likely than those who had been in practice for five years or less to believe that race has a stronger influence on quality of care in general than in their own practices.
Interest in educational programs
Almost one-quarter of respondents (N=86 of 368, 23%) had participated in an educational program to reduce racial disparities in health care. Of the 282 remaining respondents, 174 (62%) stated they would be interested in participating in such a program. Moreover, most (N=279 of 366, 76%) felt that raising awareness of racial disparities would be somewhat or very effective in reducing such disparities.
Respondents who were not interested in participating in an educational program were compared with those who had participated or would be interested in participating. In bivariate analysis, more nonwhite respondents than white respondents were interested in participating in an educational program ( χ 2 =10.4, df=1, p=.001). Respondents who worked in a university setting were more likely than respondents who worked in other settings to be interested in participating ( χ 2 =15.7, df=3, p=.001). Respondents who had been in practice longer were less likely to be interested ( χ 2 =8.8, df=3, p=.03). Self-reported familiarity with the racial disparities literature was positively associated with interest ( χ 2 =12.4, df=2, p=.001). Interest was not associated with gender, racial-ethnic makeup of the respondent's patient population, or number of professional meetings attended annually.
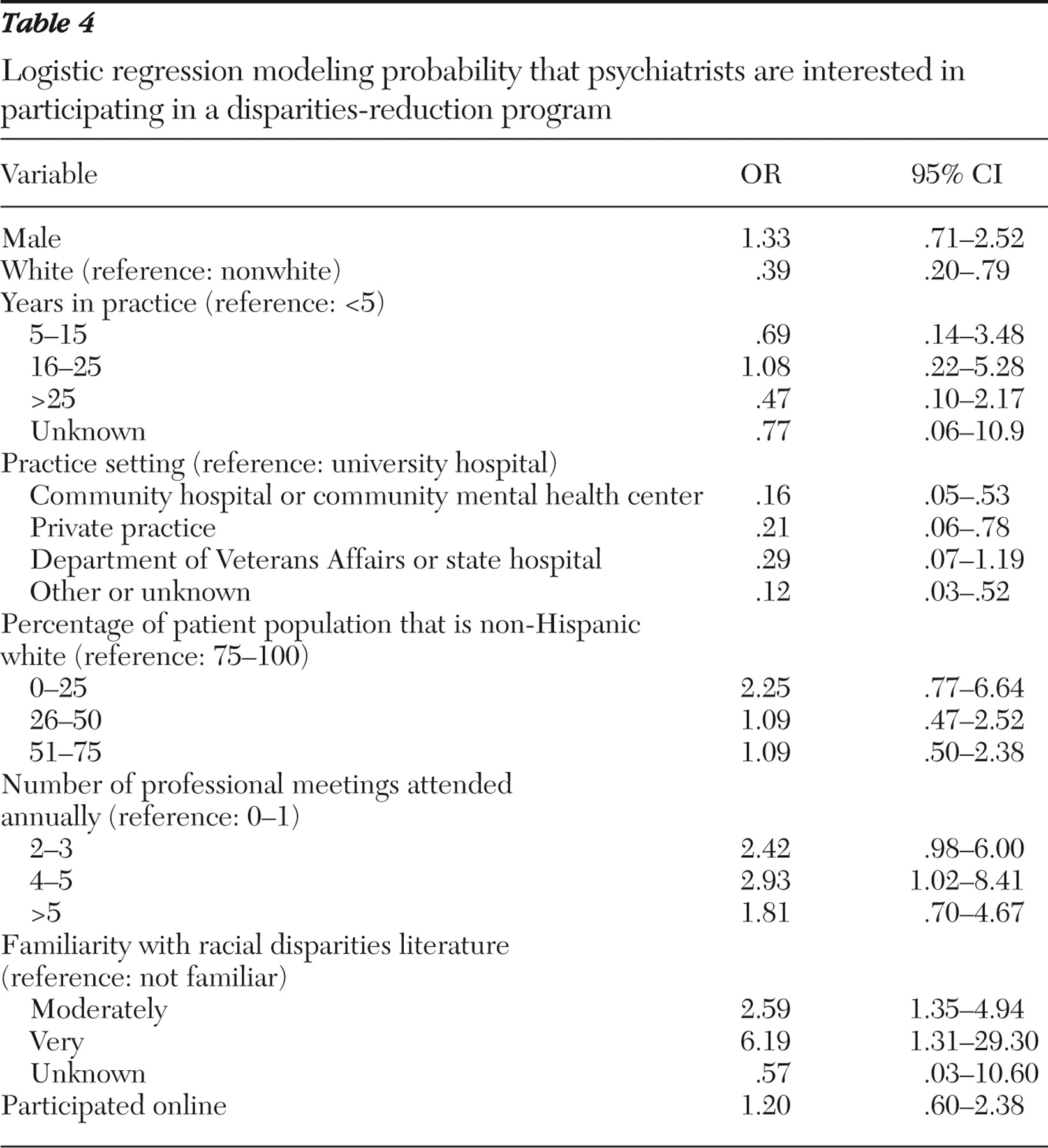
Logistic regression was used to model the likelihood that a respondent was interested in or had participated in a disparities-reduction education program. After controlling for covariates, we found that respondents' race-ethnicity, practice setting, and familiarity with the racial disparities literature were independently associated with interest in an educational program (
Table 4 ). Nonwhite respondents were more likely than white respondents to be interested in participating in an educational program, as were those who practiced in a university setting and those who were moderately or very familiar with the racial disparities literature.
Discussion
This study contributes insights into the challenges to achieving racial-ethnic equality in mental health care. Specifically, our findings suggest that many psychiatrists are unfamiliar with the body of literature on racial disparities and that, even among those who are knowledgeable about disparities, psychiatrists may be reluctant to acknowledge their own role in contributing to inequalities. Moreover, although most psychiatrists felt that increasing awareness of disparities would help eliminate inequality, a significant proportion was not interested in participating in disparities-reduction programs.
Although most respondents felt that psychiatrists had become more aware of racial disparities in the past decade, fewer than one in eight reported familiarity with research on racial disparities. This may suggest that psychiatrists are aware that disparities exist but are not well-versed in the academic literature. Additional research is warranted to determine how physicians learn about health care disparities, as well as to objectively determine physicians' knowledge. Identifying gaps in knowledge, as well as identifying preferred sources of information, will help guide the design of future interventions.
Knowing that disparities exist is, by itself, an insufficient impetus to change. Health care providers will be more motivated to change their behavior if they believe their behavior may contribute to racial-ethnic disparities. Troublingly, not only did respondents in this study believe that disparities were more likely to exist in other providers' practices than in their own, but they also generally believed that disparities were more prevalent in other medical fields than in their own, a finding that is consistent with other research (
16 ). We posit that this trend reflects a natural discomfort that results when health care providers are asked to consider their own contributions to racial-ethnic inequalities. Although it is distressing to address others' contributions to disparities, it is almost certainly more difficult to consider our own discriminatory and racially driven behavior, particularly when that behavior arises from unconscious beliefs and assumptions (
10 ).
Our results indicate that recently trained psychiatrists are more likely to perceive racial disparities as equally prevalent in their own practices as in other providers' practices. This may reflect an increased focus in medical education on issues of race-ethnicity, or it may reflect a more general shift in cultural beliefs about race and racial inequality among younger generations. Somewhat contradictorily, however, physicians who were more familiar with the disparities literature were more likely to see disparities as more prevalent in other physicians' practices, suggesting that education about racial-ethnic disparities may have an effect that is opposite of what is intended. Physicians who are more educated about disparities may believe they have been able to achieve equality in their own practices, and this is indeed a valid possibility but one that should be tested empirically. Another possibility is that familiarity with the research on racial disparities does not itself render physicians more willing to accept their role in perpetuating inequalities. Understanding the complex relationships between these various factors requires longitudinal studies that measure changes in physicians' attitudes, beliefs, and behaviors over time.
A limitation of this study is that our sample may not be representative of all psychiatrists practicing in the United States, because members of the APA and psychiatrists who attend APA meetings may be systematically different from other psychiatrists. Our response rate was adequate for this type of study, but response bias may limit the generalizability of our results—that is, we cannot determine whether psychiatrists who elected to participate in the study are systematically different from those who did not respond. Moreover, all data were collected by self-report, which may make comparisons less reliable. We attempted to standardize responses by defining all key terms, but our findings must be interpreted as stemming from respondents' subjective beliefs. Finally, the cross-sectional study design prevents us from drawing conclusions as to causation. Longitudinal research is needed to clarify the direction of the relationships that we have reported.
Conclusions
Once physicians have begun to consider their own role in perpetuating racial-ethnic disparities and have expressed an interest in changing their behaviors, what are the most effective interventions? Increasing awareness of racial-ethnic disparities is useful but insufficient (
17 ). When educational interventions are undertaken, they may be most effective when presented from within the provider community—for example, educational information presented by the APA or other national or local professional groups may be deemed more authoritative and believable than information from other sources (
16 ).
Ideally, programs to reduce disparities should include a component to demonstrate the existence of disparities within the physicians' own practices (
17 ). For example, hospitals or CMHCs may collect data on patient outcomes or patient satisfaction and examine these findings for correlations with race-ethnicity. Reporting these findings to the treating physicians may help physicians to understand and accept the pervasive nature of racial-ethnic disparities (
13 ). In the authors' personal experience, however, a major limitation of this approach is that such feedback may be met with skepticism by physicians who are not yet prepared to confront their own role in the existence of disparities. Broaching this topic with physicians in a nonaccusatory and collaborative manner is essential for success.
In addition to providing information, programs to reduce disparities in clinical care should also emphasize cultural sensitivity and cultural competence. Cultural sensitivity refers to one's insight into his or her own cultural beliefs and experiences (
13 ), whereas cultural competence refers to one's ability to understand and respond effectively to others' cultural needs and to establish interpersonal relationships bridging cultural differences (
7 ). Several components of effective cultural sensitivity and cultural competence training programs have been described. First, programs should help clinicians understand how their own experiences affect their perceptions of other races (
13,
18 ). Second, programs should help clinicians become aware of the circumstances that activate racial-ethnic stereotyping (
13 ). Third, programs should introduce communication techniques that help clinicians approach their patients as individuals; the "patient-centered communication" approach is perhaps the most widely described and advocated of these techniques (
7,
9,
13,
19 ). Finally, programs should help clinicians learn to attend selectively to relevant racial-ethnic and cultural information and screen out irrelevant information (
20 ). Relevant information may include cultural differences in health beliefs, medical practices, attitudes toward medical care and the medical system, and levels of trust of physicians (
3 ). Relevant information may also include differences in incidence and prevalence of certain illnesses among specific groups and differences in pharmacokinetics and pharmacodynamics (ethnopharmacology) (
3,
21 ).
Ultimately, racial-ethnic disparities in health care will persist as long as there are inequalities in our society. Physicians, nonetheless, have the special opportunity and obligation as leaders within the health care community to improve the quality of care and health outcomes of patients from racial-ethnic minority groups. High-quality, empirically driven interventions may help physicians and other health care providers come one step closer to the goal of health equality.
Acknowledgments and disclosures
The Committee to Aid Research to End Schizophrenia (CARES) sponsored this study.
The authors report no competing interests.