Insurance is an important variable affecting access to health care. Yet little is known about the relationship of insurance to care in the early stages of psychosis. Specifically, little is known about type and adequacy of insurance benefits for patients experiencing their first episode of psychosis and how insurance influences service delivery during the critical early course of illness, when rapid intervention may improve long-term outcome
(1). Using data from the National Comorbidity Survey, the National Advisory Mental Health Council
(2) reported that, of individuals with severe mental disorders, 64% had private insurance, 18% were insured by government programs, and 18% had no insurance. This distribution is very similar to that for the U.S. population (64%, 22%, and 14%, respectively). On the other hand, among the approximately 42 National Comorbidity Survey respondents with nonaffective psychosis, only 44% had private insurance, 31% had government insurance, and 25% had no insurance (Kessler, 1997, personal communication). In a consecutive admission sample of 50 patients each from one private and one public psychiatric hospital, Minkin et al.
(3) found that although all of the patients in the private hospital had either private insurance or Medicaid/Medicare, only 36% of those in the public hospital had coverage.
Using data from the Epidemiologic Catchment Area (ECA) study, Landerman et al.
(4) found that having any insurance coverage for outpatient mental health care is strongly associated with obtaining care. This relationship was stronger for those patients with a DSM-III diagnosis than those without. Others have found that type of insurance coverage predicted use of services. For example, depressed patients covered by fee-for-service plans had more outpatient visits than those insured by prepaid plans (health-maintenance-organization [HMO]-type plans)
(5). Similarly, utilization of inpatient services was related to how care was managed
(6). Although the few studies conducted have suggested that insurance status has an important association with use of mental health services, a significant limitation has been their reliance on respondents’ reports. Owing to the complexity of insurance, many people are unclear about their insurance coverage. For example, Landerman et al.
(4) found that 44% of ECA respondents did not know whether they had mental health insurance coverage.
The purpose of this study was to describe the distribution of insurance status, based on multiple sources of information, in a first-admission sample of patients with psychotic disorders and examine the relationship between type of insurance and care received early in the course of the illness. Specifically, we determined whether respondents had health insurance and the type of insurance. Then we examined the relationship between insurance status and having had pharmacotherapy or psychotherapy before first admission, time from onset of psychosis until hospitalization, whether the hospitalization was voluntary or involuntary, and whether the inpatient facility was a public or a community hospital.
METHOD
Sample and Procedure
Data were taken from the Suffolk County Mental Health Project. Details about the design of the Suffolk County study have been presented elsewhere
(7). Briefly, the sample was composed of 696 presumed psychotic patients hospitalized in one of the 12 psychiatric facilities in Suffolk County, New York, between September 1989 and December 1995. The facilities included six 20–30-bed community hospital units, a 30-bed university hospital unit, a Veterans Administration (VA) hospital, two private hospitals (added in 1994), an adult state psychiatric center, and a child state psychiatric center. In most hospitals, the chief nurse or chief social worker for the unit identified eligible patients and obtained verbal consent for a project interviewer to contact them. At the academic and adult state facilities, a project interviewer reviewed all admissions
(8).
The inclusion criteria were age 15–60; resident of Suffolk County; and clinical evidence of psychosis, prescription of neuroleptic medication, or a facility diagnosis indicating psychosis on admission. These broad criteria meant that a small number of patients referred to the study were diagnosed as nonpsychotic by the research team
(9). Exclusion criteria were first psychiatric hospitalization more than 6 months before current admission, moderate or severe mental retardation, and non-English-speaking status. The response rate for the initial interview was 72% (N=696).
Informed Written Consent
After obtaining written consent for the baseline interview, we obtained written permission from patients to review their medical records, talk with the treating clinician, and interview significant others. At the state hospital, according to the institutional requirement, previous written approval was obtained from physicians indicating that patients were competent to provide informed consent.
Diagnosis
The Structured Clinical Interview for DSM-III-R (SCID)
(10) was administered at baseline and at 6-month follow-up by master’s level mental health professionals who had 3–6 months of training. Interviewers took copious notes, and most interviews were audiotaped. The baseline SCID ratings combined information obtained from the interview, the medical record review, the clinician interview, and the significant other
(11). Interrater reliability was routinely checked and, as reported elsewhere
(8), was in the acceptable-to-excellent range.
Diagnoses of psychosis were based on a consensus of two (baseline) to four (6-month follow-up) psychiatrists after review and discussion of all relevant diagnostic materials
(8,
9). In this paper, the 6-month follow-up diagnoses were used for 465 patients, and the baseline evaluations were used for 60 patients who did not receive a follow-up assessment.
The present analysis is based on 525 respondents with the following DSM-III-R diagnoses: bipolar disorder with psychotic features (N=150), major depressive disorder with psychotic features (N=98), other nonorganic psychoses (N=59), and schizophrenia spectrum psychoses (N=218).
Measures
Five demographic variables were analyzed: age, sex, race, marital status, and household socioeconomic status. Although the educational level of patients was known, it was not included in this analysis because many patients were young adults who had not yet reached their terminal point of education.
Household socioeconomic status was rated by applying the Hollingshead 7-point occupational scale to the person who contributed the most financially to the household in which the respondent lived at baseline. An additional scale point, number 8, was added for patients whose major source of support was public assistance. In cases where occupational status was unknown (where the primary support came from pension or savings, for example), the rating was made on the basis of the parents’ occupation in the household in which the patient was raised. The higher status was used in the event that two parents had different socioeconomic statuses.
Treatment variables included pre-admission treatment history according to clinical interviews and treatment records. These were used to rate type and extent of previous treatment with a modified version of the Strauss-Carpenter Prognostic Scale
(12). This included whether the respondent had had previous treatment and the type of this treatment (antipsychotic pharmacotherapy, nonantipsychotic pharmacotherapy, psychotherapy, and other treatment). Substance abuse treatment was not analyzed in this report.
Because obtaining psychiatric care often occurs in response to violence or suicide attempts, measures of both were included. Since the current analysis focuses on care obtained during the respondent’s lifetime, lifetime violence and suicide attempt measures were preferred over measures reflecting the behavior only at time of the hospital admission. Suicide attempt was measured by using a dichotomous lifetime variable ascertained as part of the SCID. A three level composite measure of lifetime violence (none, some, and a lot) was created from information on the Strauss-Carpenter Prognostic Scale
(12), the interview with the significant other, the hospital discharge record, and the Structured Interview for Schizotypy
(13). None was defined as no evidence of violence from any source. Respondents with a lot of violence were those who were rated on the Strauss-Carpenter Prognostic Scale as being frequently violent or who on the Structured Interview for Schizotypy endorsed more than one physical fight as an adult. Respondents not included in the categories of none or a lot were assigned to the category of some violence.
Data on insurance status (staff-model HMO, preferred provider, fee for service, Medicaid or Medicare, VA, or no insurance) were assembled from multiple sources (hospital admission and discharge records, hospital billing records, respondent and significant other responses to a questionnaire on insurance, employment history, and interviewers’ narratives). The most informative data sources for insurance type were hospital admission and discharge records, available for 438 (83%) of the 525 patients. In one hospital, billing records were also available (N=181). For the 87 patients for whom such data were not available, we integrated information provided by the significant other and the respondents. In the few cases where insurance status remained unclear, patient records were further reviewed for other information, such as employment history, which might help determine whether and what type of insurance the respondent had. The interrater reliability of the insurance coding was checked by having 50 randomly selected records recoded by a second rater. The raters agreed in all but five cases. Disagreement stemmed from the fact that the second rater was less familiar with hospital records than the primary rater. These disagreements were resolved after the raters conferred.
Statistical Analysis
Preliminary analysis indicated that only one respondent was a subscriber to a staff-model HMO and eight were insured by the VA. In half of the cases with private insurance, it was difficult to determine if the coverage was preferred provider or fee for service. This occurred because some insurers provide both types of coverage, in many cases respondents were not sure themselves, and in other cases insurance information came from hospital records where only the name of the plan and not the type were noted. Therefore, for this analysis, HMO, preferred-provider, and fee-for-service categories were combined into one category of private insurance. Thus, we stratified the insurance types of the sample into three groups: 1) private insurance, 2) Medicaid or Medicare, and 3) no insurance.
Bivariate analysis (chi-square and analysis of variance) was conducted to examine differences among the insurance groups on a set of nine background, demographic, and clinical variables. Similar analyses were performed to examine the relationship of insurance to pre-admission treatment received, with seven treatment measures. Modified Bonferroni correction was used to control for multiple comparisons within domains: five demographic variables (p<0.01), three clinical variables (p<0.02), three prehospitalization outpatient treatment measures (p<0.02), and three hospitalization measures (p<0.02).
As a multivariate test of the association of insurance type with treatment, logistic regression analysis was used to compare private versus no insurance in one model and Medicaid/Medicare versus no insurance in another model. These models were run in two stages. Insurance type was the dependent variable in these models. At first the nine background, demographic, and clinical variables and previous outpatient treatment were included. Then the models were run again with the addition of the hospitalization variables to test the relationship of hospitalization variables and insurance while controlling for previous outpatient treatment. Initially, the models included a test for interaction of diagnosis and other variables by including a dummy variable of affective versus nonaffective psychosis as an interaction term with all control variables. Since these interactions were not significant, they were not included in the final models.
RESULTS
At the time of first admission, 233 (44.4%) of the patients had no insurance, 78 (14.9%) had Medicaid or Medicare, and 203 (38.9%) had private health insurance. Eight (1.5%) were insured by the VA and excluded from the rest of the analysis because of the dissimilarity between the VA and the other government and nongovernment types of insurance. The insurance status of three patients was unknown.
There was no significant difference in age among the three insurance groups (the mean age for the entire sample was 29.5 years, SD=9.5); there was also no difference among the groups in the proportion with suicidal behavior (26.1%).
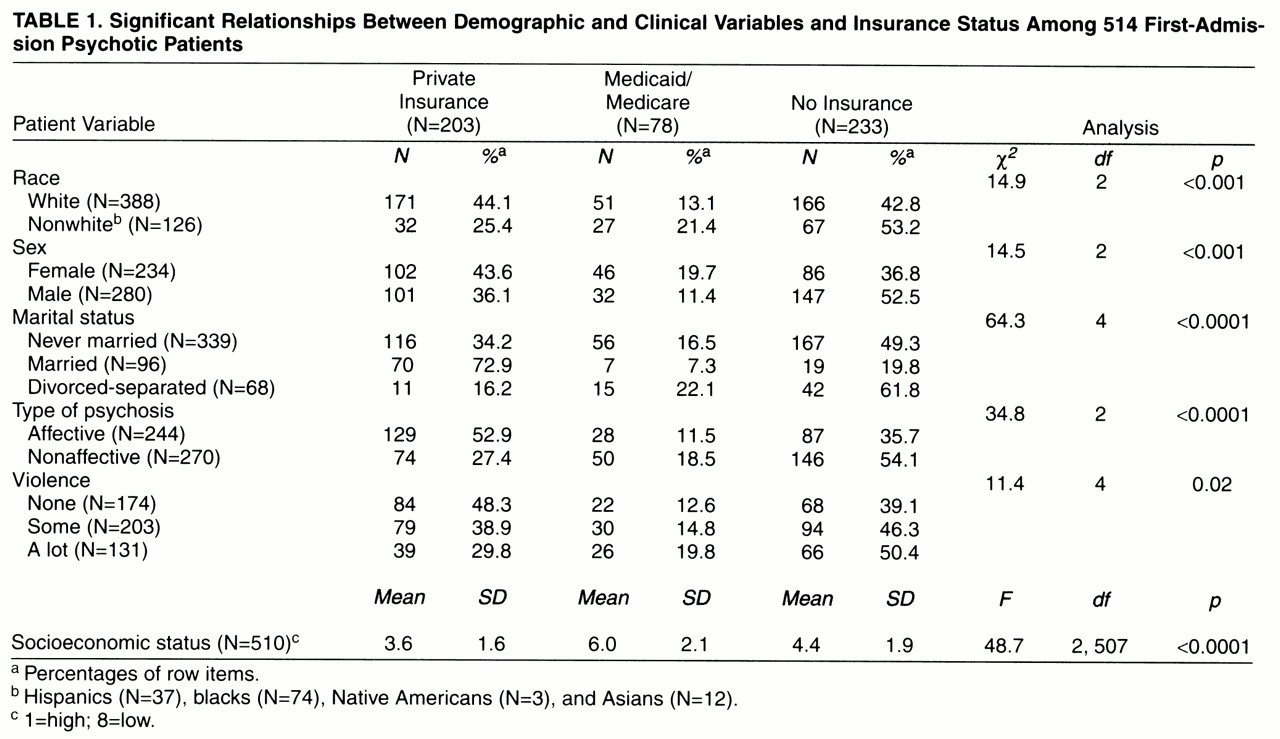
Table 1 presents the other demographic and clinical characteristics that were significantly associated with insurance status. As can be seen, white patients were more likely to have private insurance or no insurance, and nonwhite patients were more likely to have no insurance. Female patients were more likely to have private insurance, and male patients were more likely to have no insurance. Considerably more married patients had private insurance than did nonmarried or divorced-separated patients. Patients with affective psychosis were most likely to have private insurance, and those with nonaffective psychosis were most likely to have no insurance. Less violence was associated with a greater likelihood of having private insurance, although this finding was of borderline significance after adjustment for multiple comparisons. The private insurance group had the highest mean socioeconomic status level, followed by the group with no insurance and then the group with Medicaid/Medicare. Since having Medicaid often co-occurs with getting public assistance, which was our added number 8 on the socioeconomic scale, this rank order is not surprising.
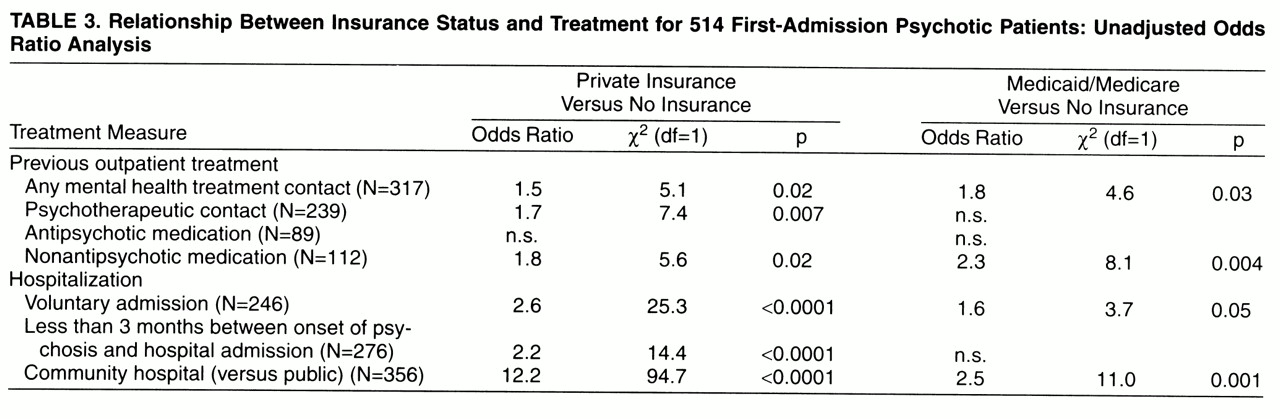
Tables 2–
4 present the relationship between insurance status and treatment. The odds ratios presented in
tables 3 and
4 are based on comparisons of each insurance group with the no insurance group.
Table 3 presents the unadjusted odds ratios.
Table 4 presents the adjusted odds ratios from the logistic regression models, which included demographic, clinical, and treatment variables. By and large, the adjusted and unadjusted odds ratios were very similar. On the basis of adjusted odds ratios, having private insurance was associated with a greater likelihood of having received previous mental health treatment in general, and psychotherapy specifically. There was also a clear trend that having private insurance was related to a greater likelihood of being hospitalized within 3 months of onset of psychosis, being admitted voluntarily, and being admitted to a community hospital rather than a public hospital. Having Medicaid/Medicare was related to a greater likelihood of receiving nonantipsychotic medication treatment. In addition, we found a trend toward a relationship between having Medicaid/Medicare and a greater likelihood of having received previous mental health treatment in general, being admitted voluntarily, and admission to a community hospital rather than a public hospital.
DISCUSSION
The results of this study suggest that 44% of first-admission psychotic patients have no health insurance, 15% have Medicaid/Medicare, and 39% have private insurance. Even after adjusting for diagnosis and key demographic variables, we found that patients who had private health insurance and, to a lesser extent, those who had Medicaid/Medicare were more likely to have received mental health assistance before their first psychiatric hospitalization. The private insurance group was more likely to have had psychotherapy and the Medicaid/Medicare group to have received nonantipsychotic medication. However, having insurance did not increase the likelihood of getting antipsychotic drug treatment. Having private insurance was associated with a greater likelihood of earlier (sooner) admission to the hospital after the onset of psychosis, being admitted on a voluntary basis, and being hospitalized in a community rather than a public facility. Having Medicaid/Medicare was also associated with a greater likelihood of admission to a community hospital and a strong trend toward having a voluntary admission.
These findings suggest that having some kind of health insurance is associated with obtaining some care before the first admission for psychotic illness. Having Medicaid/Medicare and private insurance were both associated with obtaining outpatient care. However, although having private insurance increased the likelihood of admission closer to the time of onset of psychosis, having Medicaid/Medicare did not. This was true both in the bivariate and multivariate analyses. In additional analyses not presented here, we found that the lack of difference in this time interval between the Medicaid/Medicare patients and those with no insurance was not related to socioeconomic status. One possible reason for this is that patients with private insurance may be more likely than Medicaid/Medicare patients and those with no insurance to be treated by private practitioners, who for the most part have admitting privileges and are thus easily able to admit their patients. with no insurance, are more likely to be treated in the state mental health care system, where the need for admission is reevaluated by state psychiatrists in the inpatient facility. Thus, there is an extra evaluation element for patients admitted to the state system. Another reason may relate to the fact that, compared with the private insurance group, Medicaid/Medicare patients, as well as patients with no insurance, were more likely to be hospitalized in public facilities. Such facilities are perceived to be less desirable, and patients might be more reluctant to be admitted to such hospitals. This may also contribute to the higher proportion of involuntary admissions among the Medicaid/Medicare and no insurance groups.
Some data relevant to this will become available during the coming year as Medicaid in Suffolk County moves over to managed care for mental health services. Under this arrangement, care will be provided by the private sector. Once the managed care Medicaid model is introduced, we plan to compare services and outcome variables under the non-managed-care and managed care models. In addition, we will be focusing on changes in insurance status for the entire sample over time and how this relates to care.
Our finding that 44% of first-admission patients had no insurance is alarming. It is considerably higher than the estimates based on the self-report data in the National Comorbidity Survey
(2), which indicate that 18% of patients with chronic mental disorder had no insurance. We do not think that this difference can be explained by underreporting in the current study because we used multiple data sources, including hospital records. Although it is possible that in the course of time many of the uninsured respondents will obtain insurance, it is likely that this will be Medicaid/Medicare.
We had hoped to compare patients’ treatment with a more specific typology of insurance to be rated by the extent to which the benefit was managed (e.g., HMO, preferred provider, and fee for service) and based on the extent of mental health care coverage, which is known to vary considerably and often to be inadequate for mental health care
(14,
15). However, this was not possible because we were uncertain in many cases as to what type of coverage the patients had, owing to the complex nature of insurance arrangements. Many insurance companies provide different plans, sometimes based on differences in employers. For example, patients with the same insurance company and plan name could have care provided by an HMO, by fee for service, or by a preferred provider. We had a similar difficulty in obtaining information on mental health coverage. The same plan of a given health insurer could vary tremendously in the benefits offered for mental health. Furthermore, these arrangements change even during a given policy year; for example, mental health care could be shifted from being provided in-house to being provided by an outside contractor.
We also found that insurance companies were not overly enthusiastic about helping us understand the type of coverage that they provide. Letters and phone calls requesting information went virtually unanswered, and promises to send information more often than not went unfulfilled. We can only speculate about the reasons for this lack of willingness to share information, such as staffing shortages or the sensitive nature of information on benefits in a very competitive and uncertain market, particularly in regard to mental health coverage. However, this difficulty in obtaining information may also be experienced by patients and their families who are in need of care and attempting to access care. To the extent that this is true, procedures for ensuring easier public access to information on insurance benefits are needed.