Major depression remains one of the most debilitating illnesses confronting society, exerting a major impact on social, emotional, and occupational functioning
(1). Since the disorder can exhibit a perilous course once established, identifying early predictors of later-life depression might facilitate interventions that reduce the impact of the disorder before a chronic course has been established. Prospective epidemiologic studies offer perhaps the best design for identifying such early predictors because these studies remain free of biases that limit conclusions from cross-sectional, retrospective, or clinic-based studies. Given the fact that the incidence of depression dramatically increases from adolescence into early adulthood, prospective epidemiologic studies across this age range provide particularly important information
(2). After complete description of the study to the subjects, written informed consent was obtained. For all participants less than 18 years of age, a parent or guardian also provided written consent.
Using prospective epidemiologic data, we recently showed that adolescents with major depression face a two-fold to four-fold greater risk for depression as young adults
(2); this finding is consistent with those of clinic-based studies. Although this suggests the importance of targeting interventions for adolescents with major depression, the diagnosis of depression is far less common than other potential predisposing factors for depression. Specifically, a large proportion of adolescents exhibit depressive symptoms that are subthreshold for a diagnosis. Studies among adults suggest that such subclinical syndromes carry a high risk for full-blown episodes of major depression
(3). It is crucial, however, to extend these findings to adolescents, among whom “moodiness,” or subclinical depressive symptoms, may be part of the normal process of emotional maturation. The current study examines this issue, testing the hypothesis that subclinical depressive symptoms in adolescence are not part of normal, developmental moodiness but, rather, are harbingers of serious adult depressive disorders.
METHOD
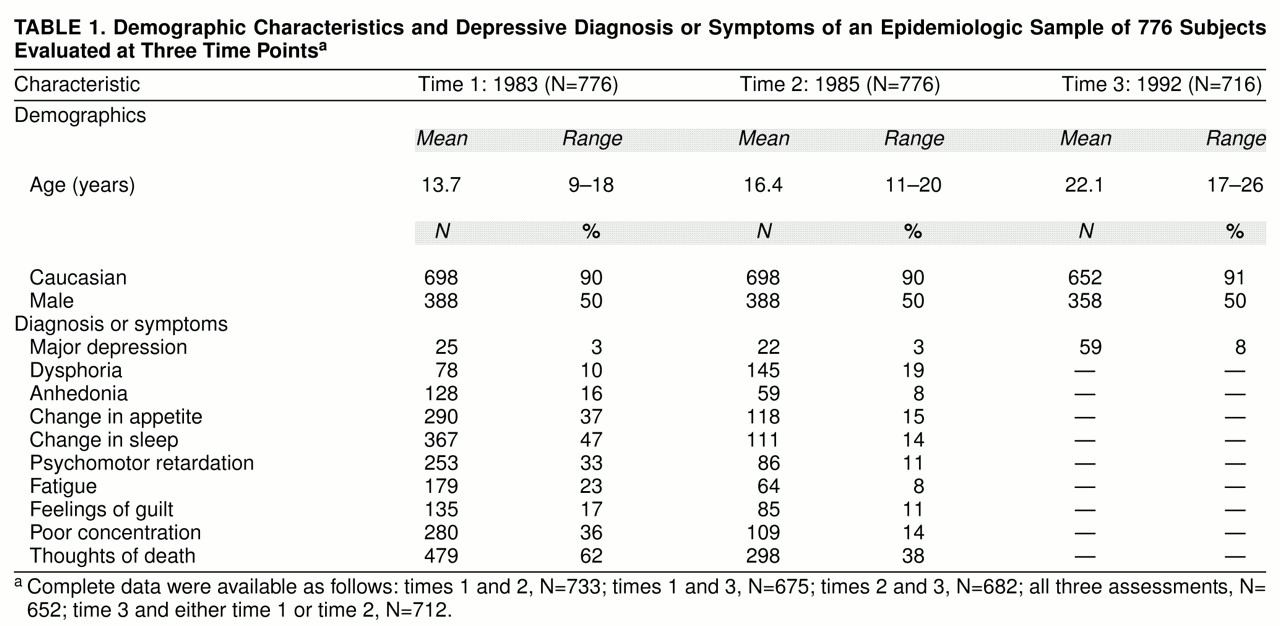
This study is based on an epidemiologically selected cohort of 776 subjects living in semirural New York State. Subjects received psychiatric assessments in 1983 (time 1), 1985 (time 2), and 1992 (time 3). The sample was randomly selected by using complete enumeration and remained representative of the geographical area from which it was selected
(2).
Parent and child interviews in 1983 and 1985 assessed depressive symptoms by using an unpublished schedule developed by Orvaschel covering DSM-III-R criteria and involving modifications of the Diagnostic Interview Schedule for Children. At time 3, only young adults provided diagnostic information; parents were not reinterviewed. All disorders were diagnosed without exclusionary criteria and had to be present during the previous year.
We assessed psychopathology both dichotomously and continuously using disorder-specific symptom/impairment scales. Symptom/impairment scales were derived by summing positive responses to questions regarding symptoms or impairment for each disorder. Because cross-informant agreement is usually poor, we combined parent and child information using standard algorithms designed to maximize sensitivity and specificity. Diagnoses required both endorsement of DSM criteria from either parents or subjects and a symptom/impairment score at least one standard deviation above the sample mean. Impairment questions covered inability to perform schoolwork or social activities because of depressive symptoms. Other work with these data supports the validity of the diagnoses
(2). Reliability is suggested by the correlation between time 1 and time 2 depression symptom/impairment scale scores (r=0.47, N=733, p<0.001).
Logistic regression was used to examine associations between adolescent depressive symptoms and an adult diagnosis of major depression. All subjects who met criteria for major depression at either time 1 (N=25) or time 2 (N=22) were excluded from the analyses. We also considered the predictive value of adolescent symptoms in other domains after removing subjects who met criteria for the full-blown disorder of interest in adolescence. All logistic models included age, sex, and social class as covariates. To provide estimates of effect sizes, associations with symptom scale scores are presented as odds ratios for a difference in symptoms of two standard deviations from the mean.
RESULTS
Table 1 displays characteristics of the sample. Although information on 776 individuals was collected at each time point, complete psychiatric data were not available for all subjects, as summarized in
table 1. Interestingly, although the prevalence of dysphoria was considerably higher at time 2 than time 1, the prevalence of other symptoms was highest at time 1.
Depressive symptoms in adolescence predicted major depressive episodes in adulthood, after we controlled for age, sex, and social class. This was true both for time 1 (χ2=11.6, df=1, p<0.001) and time 2 (χ2=5.9, df=1, p=0.01) symptoms. From the standpoint of effect sizes, a difference of two standard deviations from the mean in depressive symptoms predicted a two-fold to three-fold greater risk for an adult depressive episode (time 1 odds ratio=2.56, 95% confidence interval=1.49–4.41; time 2 odds ratio=1.85, 95% confidence interval=1.12–2.96).
When we reexamined these associations for each sex and for each of two age strata formed by dichotomizing the sample at the median age, we found no significant interactions with either sex or age (data not shown). An interaction term between time 1 and time 2 symptoms was fit but was nonsignificant. We also fit models including other risk factors for depression, such as health-related variables, from our previous work. Such other factors did not remove the association between adolescent depressive symptoms and adult major depression.
We examined the predictive value of individual depressive symptoms. At time 1, no symptom entered the model, suggesting that the overall depressive symptoms were the most salient predictors. At time 2, however, both anhedonia (odds ratio=2.84, 95% confidence interval=1.08–7.46) and thoughts about death (odds ratio=1.44, 95% confidence interval=1.13–1.83) entered. Finally, no symptoms of disorders besides depression predicted adult major depression.
DISCUSSION
Consistent with previous studies among adults
(3), the current report found a predictive relationship between subclinical depressive symptoms in adolescence and major depression in adulthood. These findings are also consistent with previous reports noting depressive symptoms to be relatively stable through adolescence
(4). The findings might alert clinicians to the potential significance of depressive symptoms below the threshold for a disorder. Moreover, from the public health perspective, the findings might alert the field to the importance of considering targeted interventions on subclinical depressive symptoms among adolescents.
With respect to specific symptoms, Eaton et al.
(5) found that a range of individual depressive symptoms in adults strongly predicted full-blown depressive episodes at follow-up. Eaton et al.
(5) found a stronger magnitude of associations for many symptoms than we did in the current study; we found that only anhedonia or thoughts of death predicted adult depression and that these associations occurred only at time 2. Taken together, these data suggest that as individuals mature, a wider array of specific symptoms might predict future depression. Such age-related trends are interesting in the light of differences in symptom prevalence between time 1 and time 2. Higher rates of dysphoria but not other symptoms at time 2 might relate to developmental changes in the manifestation of depression, which could, in turn, relate to the stronger associations for individual symptoms seen in older cohorts.
As discussed elsewhere
(2), our results should be interpreted in the light of limitations of standardized, epidemiologically based instruments. Because such limitations tend to diminish statistical power, our data may underestimate the true risk for adult disorders faced by adolescents with depressive symptoms. Effect sizes may be smaller due to the limited specificity of symptom ratings in epidemiologic versus clinical samples. Such limited specificity is exemplified by the high rate of thoughts about death at time 1 in this sample. Finally, the current study assessed depression at three relatively widely spaced time points. Although the study outlines the predictive value of adolescent symptoms, it seems important to know if adolescent symptoms predict full-blown depressive episodes over shorter intervals.