Depression is commonly found as a coexisting condition in patients with dementia and has been estimated to occur in 11%–57% of these patients
(1–
3). Most prior studies have found the prevalence of major depression in Alzheimer’s dementia to be between 15% and 20%
(4), and depression may be more common in vascular dementia
(5). The variation in prevalence estimates is probably caused by studies’ use of different criteria for the diagnoses of depression and dementia and differences in patient selection criteria. This variation also probably reflects the overlap of some symptoms of the two disorders
(4,
6). Some reports have suggested that depression may occasionally represent the initial clinical presentation of a dementing illness
(4,
7).
Patients with coexisting dementia and depression have long been thought to have a poor long-term course of depression
(8,
9), but no studies have specifically examined relapse or recurrence rates in this population. There have been a limited number of studies examining the course of illness in these patients
(10–
13), and in general these studies have involved small numbers of patients (in the largest, N=21), with follow-up determinations usually involving changes in rating scale scores as opposed to actual measures of relapse or recurrence. In addition, only one of these studies
(10) compared patients who had coexisting dementia and depression with patients who had either disorder alone in terms of course of illness, and that study compared only patients with dementia who were depressed and those who were not. The studies have reported contradictory results regarding the persistence of depressive symptoms in patients with coexisting dementia and depression. Lopez et al.
(10) found that seven of 10 patients were still depressed at 1 year, but there was no significant difference in outcomes (neuropsychological deficits) in comparison with patients who had dementia alone. Snowden and Lane
(11) found that two of three patients surviving at 4-year follow-up were still depressed, Brodaty and Luscombe
(12) found that three of five patients were depressed at 1 year, and Ballard et al.
(13) noted that most depression associated with Alzheimer’s dementia resolved within 3 months (as opposed to depression with vascular dementia, which was more persistent). Earlier studies examined other aspects of course of illness in patients with coexisting dementia and depression in comparison with either condition alone
(1,
14,
15). In one study
(1), initial hospital stays were noted to be significantly longer for inpatients with coexisting dementia and depression than for geriatric inpatients with either condition alone; however, response rates to antidepressant treatment were found to be similar in patients with both dementia and depression and those with depression alone. In a 2-year follow-up of 16 patients with mixed symptoms of depression and dementia
(14), a more favorable outcome was associated with greater severity of depressive symptoms at baseline and higher cognitive functioning. In another study
(15), outpatients with depression and dementia of the Alzheimer’s type did not have significant differences in outcome on assessments of physical/mental condition, self-care ability, or ability to interact in comparison with those with dementia of the Alzheimer’s type alone, when followed over a 17-month period.
There have also been four placebo-controlled studies examining the use of antidepressants in patients with both dementia and depression
(16–
19). Two of these studies (
16,
17) found significant improvement in the patients treated with antidepressants, yet this improvement was comparable to that seen in the patients given placebo. The two other studies
(18,
19) found significantly greater improvement with antidepressant treatment than with placebo.
Thus, there is some suggestion from these studies that 1) patients with coexisting dementia and depression may not have a more severe course of illness than do patients with dementia alone, 2) they may have as good a response to antidepressant treatment as patients with depression alone, and 3) the prognosis may be better in patients with milder dementia. Our clinical observation has been that patients with both dementia and depression often require more intensive clinical management than patients with either condition alone. The literature in the area of coexisting dementia and depression is clearly limited and incomplete thus far, and little is known about long-term outcomes and health care utilization among these patients.
It is not clear at present whether the overall course of depression in dementia is similar to that of depression alone, whether the course is highly influenced by the underlying dementia, or whether the course in coexisting dementia and depression is different from that in either syndrome alone. Clearly, there is high comorbidity of depression and dementia, and this issue has far-reaching implications for utilization of health services. If the intensity of utilization is higher for patients with both dementia and depression than for patients with either syndrome alone, it suggests the need for aggressive treatment approaches and treatment guidelines for patients with coexisting depression and dementia.
No studies have examined rehospitalization rates in patients with coexisting dementia and depression. Some authors have examined rehospitalization rates for patients with late-life depression as a marker of “severe relapse” in order to identify characteristics of patients at high risk for future hospitalization
(20,
21). While patients may relapse without rehospitalization, readmission serves as a discrete outcome, is an indirect measure of severity of illness, and measures hospital utilization
(20). In this study we sought to examine interactions between dementia and depression in terms of the impact on course of illness in a large group of older patients in the Department of Veterans Affairs (VA) health care system with the use of outcome measures such as readmission and others as well. On the basis of our clinical observation (noted above) that patients with both dementia and depression often require more intensive clinical management than patients with either condition alone, we hypothesized that comorbid dementia and depression interact to worsen the severity of course of illness, as quantified by intensity of utilization of inpatient and outpatient services.
METHOD
Data were obtained from the VA Patient Treatment File. This national computerized database contains discharge records for all VA medical centers across the United States and includes information regarding patients’ characteristics, such as age, race, gender, and marital status, and administrative data, such as admission and discharge dates and discharge diagnoses (including primary diagnoses that are responsible for length of stay, as well as accompanying secondary diagnoses). In addition, the VA has a separate data file, the Outpatient Clinic File, which includes information pertaining to utilization of outpatient care that can be linked to data from the VA Patient Treatment File.
We defined fiscal year 1992 (Oct. 1, 1991, to Sept. 30, 1992) as the index year for our study. We obtained data for fiscal year 1992 from the VA Patient Treatment File and identified all patients over the age of 60 years who were hospitalized for ICD-9-CM
(22) and DSM-III-R diagnoses of dementia (dementia of the Alzheimer’s type or multi-infarct dementia) and major depression together or for dementia or major depression alone. Patients with diagnoses of bipolar affective disorder or primary delirium were excluded from the study. We also excluded patients with dementia other than Alzheimer’s dementia or multi-infarct dementia for several reasons: 1) Alzheimer’s and multi-infarct dementias are the types of dementia most commonly encountered clinically, 2) we wished to examine differences in outcomes between these two dementia types (in patients with and without depression), and 3) many dementias with other etiologies (Huntington’s disease, Pick’s disease, etc.) are entirely different in course, so that determinations of the impact of coexistent depression would probably be exceedingly difficult.
Using this approach, we identified a total of 7,115 elderly patients and grouped them according to the diagnosis (as defined above) that was responsible for the length of stay at the index admission: group 1 for patients with dementia alone, group 2 for patients with coexisting dementia and depression, and group 3 for patients with depression alone. Within groups 1 and 2, we also identified patients by type of dementia (dementia of the Alzheimer’s type or multi-infarct dementia).
The course of illness of each patient in these groups was examined over the 2-year period after the index hospitalization. A 2-year follow-up was chosen in order to encompass the period that has often been used to measure relapse/recurrence rates in the course of late-life depression
(8,
9) and outcomes in coexisting depression and dementia
(14,
15), and because Stoudemire et al.
(21) found that the greatest risk of rehospitalization occurred within the first 18 months after index hospitalization for late-life depression.
Primary outcome variables included initial length of stay, total number of readmissions, total readmission length of stay, average readmission length of stay, lengths and rates of psychiatric and medical readmissions, time to rehospitalization (medical, psychiatric, or nursing home), and utilization of outpatient care (as measured by number of medical and psychiatric outpatient visits).
Demographic variables included age, race, gender, and marital status. Discharge location following the index stay was also examined. Because mortality rates differed between groups, a separate variable, survival months (date of death minus date of index hospitalization/365.25 × 12), was calculated for each patient. Other variables examined were the number of secondary or coexisting medical diagnoses (as an estimate of medical comorbidity) and the number of secondary or coexisting psychiatric diagnoses (as an estimate of psychiatric comorbidity); in both cases, these were diagnoses listed by clinicians in addition to the diagnoses responsible for the length of stay and for inclusion in one of the three study groups at discharge from the index hospitalization.
Categorical differences were assessed by means of chi-square tests of independence (3×2 design). Groups were compared by using three-group one-way univariate analysis of variance (ANOVA) and multivariate analysis of variance (MANOVA). The effects of covariates were examined with analysis of covariance (ANCOVA) and multivariate analysis of covariance (MANCOVA).
Specifically, our statistical analysis of outcome data involved the following steps. First, we grouped the variables pertaining to outcomes during 2-year follow-up under the following categories: overall inpatient care utilization, psychiatric inpatient care utilization, medical inpatient care utilization, nursing home care utilization, and outpatient care utilization. (One exception to what follows was the analyses performed on the variable initial length of stay and the variables for outpatient care utilization. Since initial length of stay was the only index stay variable and thus was not grouped with any others, only ANOVA and ANCOVA [both without adjustment for survival months] were performed, and these analyses included the entire study group. For the outpatient care variables, no grouping was possible because they did not relate to the same type of outcome [e.g., medical versus psychiatric], and so only ANOVA and ANCOVA were performed on data from patients in the study who had outpatient care utilization during follow-up.) Next, we performed a chi-square test regarding whether patients in a given group had each type of utilization (e.g., for overall inpatient care utilization, patients having any readmission) during 2-year follow-up. Including only patients who had utilized services in a given category during follow-up, we then performed MANOVAs for the group of variables in each category (e.g., the overall inpatient care utilization MANOVA included total readmissions, total readmission days, average readmission length of stay, and time to any readmission). In these MANOVAs we included the variable survival months in order to adjust for differential mortality during follow-up. Next, we performed ANOVAs to test differences between groups in individual outcome variables. We then performed ANCOVAs and MANCOVAS using the covariates age, medical comorbidity, and psychiatric comorbidity in addition to the adjustment for survival months. For all analysis of variance models, post hoc tests were conducted with the Tukey-Kramer method for adjustment of simultaneous pairwise comparisons. Finally, we performed a subanalysis to test for differences in outcomes by type of dementia. This last analysis used a factorial 2 (depressed, not depressed) × 2 (multi-infarct dementia, not multi-infarct dementia) design.
RESULTS
The total study group (N=7,115) consisted of 5,060 patients with dementia alone (group 1), 265 patients with both depression and dementia (group 2), and 1,790 patients with depression alone (group 3).
Sociodemographic Characteristics
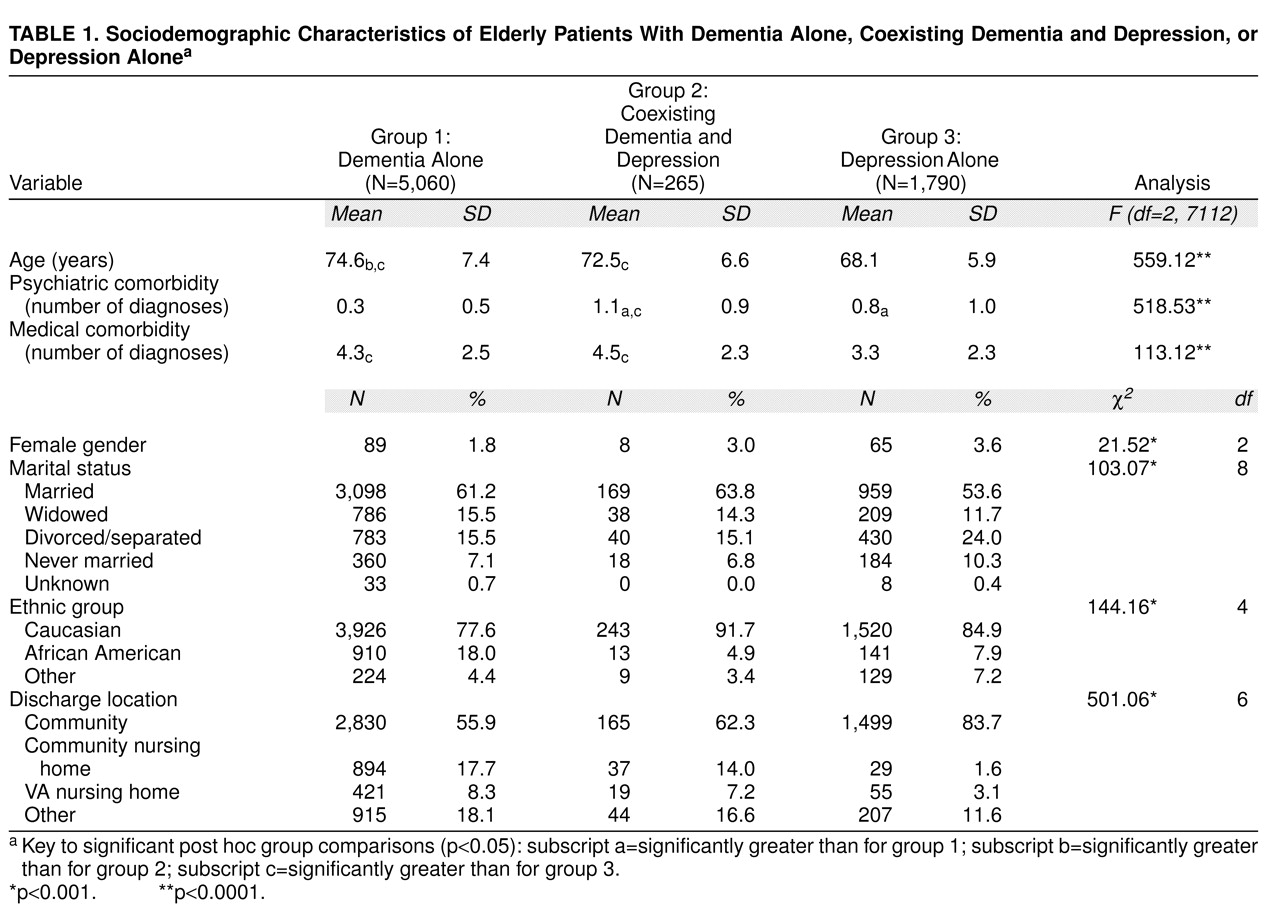
Table 1 presents sociodemographic characteristics of the patients in the three study groups. The mean age for the entire study group was 72.9 years (SD=7.6). Group 1 was significantly older than the other two groups, and group 2 was also significantly older than group 3. There were fewer women in group 1 than in the other two groups, and there was a higher percentage of African Americans in group 1 than in the other groups. Group 3 patients were more likely to have been divorced or never married than the patients in the other two groups. Group 3 had a much higher percentage of patients discharged to the community after the index hospitalization than groups 1 and 2. The latter two groups were much more likely to be discharged to a VA nursing home or a community nursing home than group 3. At index admission, group 2 had significantly more psychiatric comorbidity than groups 1 and 3. Group 3 also had significantly greater psychiatric comorbidity than group 1. Both group 1 and group 2 had significantly greater medical comorbidity at the index stay than group 3.
During the study period, 32.3% (N=2,295) of the initial study population died. A significantly higher percentage of patients in the initial group 1 (39.2%, N=1,986) died during the study period, compared with 27.9% (N=74) in the initial group 2 and 13.1% (N=235) in the initial group 3 (χ2=419.59, df=2, p<0.001). The survival times were significantly different between groups, with a mean of 18.3 months (SD=8.4) for group 1, 19.9 months (SD=7.8) for group 2, and 22.3 months (SD=5.0) for group 3 (F=183.20, df=2, 7112, p<0.0001).
Utilization of Inpatient and Outpatient Health Care Services
MANOVA and ANOVA results for utilization of inpatient and outpatient health care during the 2-year study period are reported in
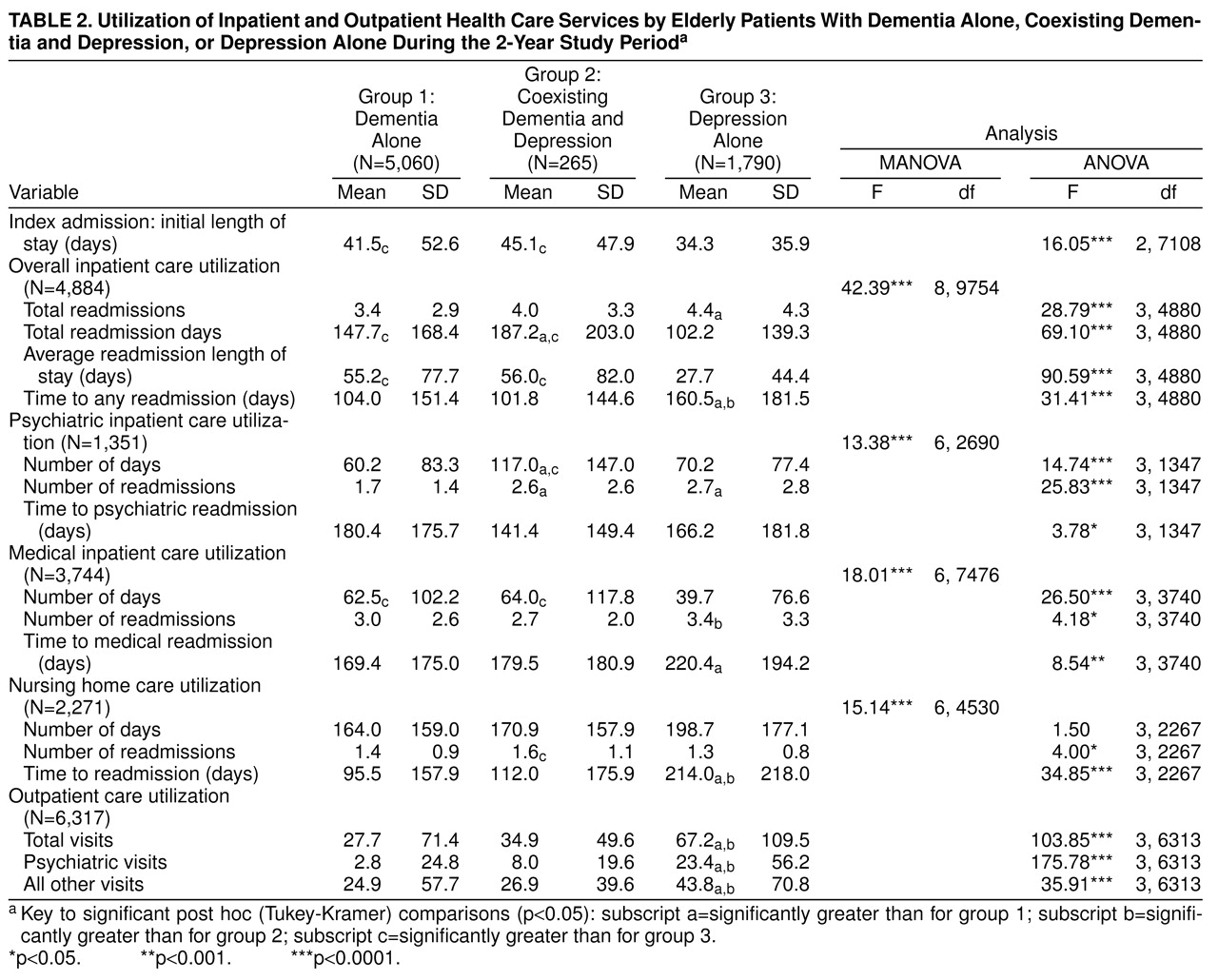
table 2. Significant differences between the study groups were found for all health care utilization variables examined. Both group 1 and group 2 had significantly longer initial lengths of stay on index admission than group 3.
There was no significant difference in the percentages of patients in the three study groups who had any type of readmission during follow-up (group 1=68.6%, N=3,472; group 2=69.4%, N=184; group 3=68.6%, N=1,228). Among patients with any type of readmission, group 2 had significantly more total readmission days than the other study groups; group 1 also had significantly more than group 3. Group 3 had significantly more readmissions than group 1. Groups 1 and 2 had significantly longer average readmission lengths of stay and significantly less time to any type of readmission than group 3.
In terms of utilization of psychiatric care during follow-up, 9.4% (N=475) of group 1, 30.2% (N=80) of group 2, and 44.5% (N=796) of group 3 had psychiatric readmissions (χ2=1080.36, df=2, p<0.001). Among patients with psychiatric readmissions, group 2 had significantly more inpatient psychiatric days than groups 1 and 3. Both group 2 and group 3 had significantly more psychiatric readmissions than group 1. Time to psychiatric readmission was less for group 2 than for the other study groups, but the difference was not significant.
With respect to utilization of medical care during follow-up, 53.8% (N=2,720) of group 1, 51.7% (N=137) of group 2, and 49.6% (N=887) of group 3 had medical readmissions (χ2=9.46, df=2, p<0.01). Among patients with medical readmissions, both group 1 and group 2 had significantly more inpatient medical days than group 3. Group 3 had significantly more medical readmissions than group 2. Group 1 had significantly less time to a medical readmission than group 3.
Regarding nursing home care utilization during follow-up, 39.5% (N=1,998) of group 1, 37.7% (N=100) of group 2, and 9.7% (N=173) of group 3 had nursing home readmissions (χ2=545.41, df=2, p<0.001). There was no difference between study groups in the number of nursing home days during follow-up for patients with nursing home readmissions. However, group 2 had significantly more nursing home readmissions, and groups 1 and 2 had significantly less time to nursing home readmission than group 3.
For utilization of outpatient care during follow-up, 86.3% (N=4,365) of group 1, 87.5% (N=232) of group 2, and 96.1% (N=1,720) of group 3 had outpatient visits of any type (χ2=128.59, df=2, p<0.001). Among the patients with outpatient care during follow-up, for all outcomes measured (total visits, psychiatric visits, and all other visits), group 3 had significantly higher utilization than the other two study groups.
Adjustment for Covariates
Three other covariates (age, medical comorbidity, and psychiatric comorbidity) were added to the original statistical model (which included the survival months adjustment for differential time to death) and tested to rule them out as alternative explanations for the group differences seen in the preceding analyses. In these ANCOVAs and MANCOVAs, the additional covariates often had significant effects on individual outcome variables; however, in only one case did they alter the overall significance of differences between groups. In that instance, when the ANCOVA was performed for initial length of stay, the overall significance of differences due to group remained (F=6.75, df=2, 7109, p<0.001); however, mean initial length of stay for group 2 was no longer significantly greater than that for group 3 in post hoc testing (least squares means: group 1=41.0 days, group 2=42.5 days, group 3=35.8 days; group 1>group 3, p<0.001). With all other outcome variables, when the effects of these covariates were controlled for, significant differences due to group remained.
Type of Dementia Subanalysis
The subanalysis performed to examine the effect of dementia type on differences between groups 1 and 2 yielded no significant interaction between group and type of dementia in any case except for inpatient psychiatric days. In that case, there was both a significant group effect (F=13.01, df=1, 547, p<0.0003) and a significant group-by-type of dementia interaction (F=9.39, df=1, 547, p<0.002). Examination of the least squares means of the four cells—(group 1 without multi-infarct dementia, mean=61.4 days; group 1 with multi-infarct dementia, mean=57.6 days; group 2 without multi-infarct dementia, mean=156.2 days; and group 2 with multi-infarct dementia, mean=76.3 days; the mean of group 2 without multi-infarct dementia was significantly greater than that of the other groups on post hoc testing)—revealed that type of dementia (patients not having multi-infarct dementia) accounted for group differences in this case.
DISCUSSION
In an attempt to examine the course of depression in patients with dementia, we compared the utilization of inpatient and outpatient care over a 2-year period of patients who had coexisting dementia and depression with that of patients who had either disorder alone. Our results indicate that patients with both dementia and depression are high utilizers of inpatient care; in our study, these patients generally utilized as much inpatient medical and nursing home care as patients with dementia alone and as much inpatient psychiatric care as patients with depression alone. In addition, the mean total number of readmission inpatient days was significantly higher for patients with depression and dementia than for patients with either condition alone. On the other hand, patients with coexisting dementia and depression did not utilize significantly more outpatient care than the other groups. In fact, they utilized significantly less total and psychiatric outpatient care than patients with depression alone.
Greenwald et al.
(1) noted that in patients with coexisting dementia and depression, depression appears to interact with dementia to lower performance on cognitive tests. Worsened course of illness in these patients could be envisioned as due to worsened overall cognition and perhaps worsened performance of activities of daily living. This worsened functioning could account for increased hospital admissions and overall utilization of care. It is also notable that in our study, patients with coexisting dementia and depression did not use more outpatient resources than the other groups, and they even used less outpatient care than the depressed group. This may relate to the fact that as cognitive impairment worsens, patients are less likely to be able to articulate more subtle changes in affective states
(4), and care increasingly relies on caregiver observation. In this case, once less subtle behavioral or affective changes are noted, the patient might be beyond the point of care in the outpatient setting and require readmission. Given that patients with dementia in our study were much more likely to be discharged to a nursing home than depressed patients, it is also possible that they were less likely to be taken for outpatient care and possibly more likely to be hospitalized when their functioning worsened.
Thirty-two percent of our initial study population died during the study period. A significantly higher percentage of group 1 died during the study period in comparison with groups 2 and 3. However, the fact that mortality differed between groups did not have an impact on group differences in the outcomes of interest when the analyses were adjusted for this variable. Other variables that might have been postulated to affect the outcomes of interest—specifically, age, medical comorbidity, and psychiatric comorbidity—also did not affect the impact of group differences (except in the case of initial length of stay). An interaction between type of dementia and group probably accounted for group 2’s significantly higher number of psychiatric care days in comparison with group 1; however, this interaction did not account for the significance of any other aspect of group 2’s high utilization of inpatient care.
Our results must be interpreted with caution, given that all patients studied were veterans and most were men, and thus the findings cannot be generalized to nonveteran populations containing equal numbers of men and women. Other limitations with respect to interpreting our results include the retrospective nature of our study and the database we used. This database is compiled primarily for administrative purposes and thus did not allow us to assess factors such as type of treatment, age at onset of depression or dementia, or accuracy of diagnoses. Finally, the group of patients with coexisting dementia and depression was relatively small in comparison with the other two study groups.
These limitations notwithstanding, the finding of increased health care utilization among patients with both dementia and depression is an important one, since it probably reflects a higher cost both to the patients themselves in terms of poorer outcomes and to the system in terms of expense. In addition, it is possible that given the difficulty of diagnosing depression in dementia (because of the overlap of symptoms between dementia and depression mentioned earlier), coexisting dementia and depression was underdiagnosed in the study group. Thus, some patients who truly had both dementia and depression may have been diagnosed as having dementia or depression alone. While it is clearly imperative to differentiate depression from dementia, it is equally necessary to consider that these disorders coexist
(2). The health care utilization of potentially undiagnosed patients with both dementia and depression may have been buried in the data on the other diagnostic groups. Use of instruments that have been created to assess depression in dementia patients
(23,
24) might be helpful for combating this potential underdiagnosis.
The results of this study provide new data on the increased liability to health care utilization of patients with coexisting dementia and depression. Further understanding of the appropriate interventions needed for this vulnerable population, with careful attention to appropriate pharmacological and psychosocial treatments, is needed. Aggressive outpatient treatment approaches and treatment guidelines for patients with both dementia and depression, while taking into consideration that many of these patients may be in nursing home settings, might improve patient outcomes and reduce utilization of inpatient care.