The prevalence of rapid cycling in bipolar populations has been variable, with rates between 13% and 56%. Dunner and Fieve
(8), in their landmark study describing rapid cycling and its apparent link to decreased lithium response noted that 20% of their bipolar I patients displayed a rapid-cycling course. The majority of studies have reported prevalence rates under 20%
(2,
3,
6,
7,
9), although studies by Cowdry et al.
(10) and Joffe et al.
(11) found rates of 56% and 40%, respectively. More recently, Tondo and colleagues
(12) found that 24% of a combined group of bipolar I and II patients had a variant of rapid cycling. Notably, all of the prevalence data on rapid cycling reported to date were derived from tertiary or specialized centers where patients sought treatment. Thus, the prevalence rates may be inflated compared to the prevalence in community samples.
The purpose of this study was to delineate the prevalence, demographic characteristics, clinical phenomenology, severity of illness, and impairment of a well-characterized group of patients who did or did not meet DSM-IV criteria for rapid cycling. We also examined whether rapid-cycling patients differed in demographic or illness variables as a function of their bipolar I or bipolar II status and determined whether significant differences existed between each subgroup with regard to gender or age at onset. We hypothesized that rapid-cycling bipolar patients would suffer from more severe depressive and hypomanic/manic symptoms, more often receive diagnoses of bipolar II than bipolar I disorder, have poorer global functioning, and appear less often as recovered than their nonrapid-cycling counterparts.
Method
Study Overview
The Systematic Treatment Enhancement Program for Bipolar Disorder is a multicenter study funded by the National Institute of Mental Health designed to evaluate the course and outcome of patients with bipolar disorder. The study combines naturalistic and randomized trial data to assess somatic and psychosocial interventions in the treatment of all phases of bipolar illness. Patients are required to be at least 15 years old and to meet DSM-IV criteria for any subtype of bipolar illness (bipolar I, bipolar II, bipolar disorder not otherwise specified, or cyclothymia). After complete description of the study to the subjects, written informed consent was obtained. The methodology of the Systematic Treatment Enhancement Program is fully described by Sachs et al.
(14).
A variety of standardized assessment tools are used at study entry and at follow-up visits. The primary assessment tools used for this study were the standardized Affective Disorder Evaluation and the Mini-International Neuropsychiatric Interview (version 4.4)
(15). Primary diagnoses were obtained by using information from the Affective Disorder Evaluation. The Affective Disorder Evaluation incorporates a modified version of the mood and psychosis modules from the Structured Clinical Interview for DSM-IV. Additionally, the Mini-International Neuropsychiatric Interview was used, given its reliability and relatively rapid administration. Study eligibility required subjects to receive a consensus bipolar diagnosis on both instruments. All research personnel were trained and certified on the Mini-International Neuropsychiatric Interview and the Affective Disorder Evaluation by using videotaped training and examples.
After an initial patient interview with the Affective Disorder Evaluation, clinicians with the Systematic Treatment Enhancement Program for Bipolar Disorder assigned patients to one of eight clinical states. Four of the clinical status definitions corresponded to DSM-IV criteria for major depression, mania, hypomania, or mixed episodes. The remaining four clinical status definitions were assigned depending on the number of mood symptoms present (if any) and the duration of time that symptoms were present. A clinical status of “recovered” was assigned if patients had fewer than three moderate symptoms for at least 8 weeks. If patients had fewer than three moderate symptoms for fewer than 8 weeks, they were assigned the status of “recovering.” If patients had achieved the status of recovered but had a subsyndromal relapse within the prior 8 weeks (at least three moderate mood disorder symptoms but not meeting full criteria for a mood episode), they were assigned the clinical status of “roughening.” If the patients did not meet symptom criteria for a major mood episode nor had achieved recovered status within the prior 8 weeks but had at least three moderate symptoms, they were assigned the clinical status of “continued symptomatic.”
Data from the Affective Disorder Evaluation, the Mini-International Neuropsychiatric Interview, the Young Mania Rating Scale, and the Montgomery-Åsberg Depression Rating Scale were used for determination of clinical status, severity of illness, number of affective episodes, and presence of psychosis. Determination of rapid-cycling status was made by examining the number of prior affective episodes in the past 12 months and applying the DSM-IV criteria for rapid cycling. An affective episode was defined as a manic, hypomanic, mixed, or depressed mood separated by 8 weeks of euthymia or an episode of the opposite polarity. In assessing syndromal recovery, only the patients who had achieved the clinical status of “recovered” were included; all other symptom states (i.e., depressed, hypomanic, manic, mixed, recovering, continued symptomatic, or roughening) were classified as “not recovered.” Any patient who abused marijuana, cocaine, amphetamines, phencyclidine, LSD, opiates, or alcohol either in the 12 months before study entry or who carried a lifetime diagnosis of substance abuse (but not dependence) was defined as a substance abuser.
Statistical Analyses
The nonparametric Wilcoxon test was used to compare continuous variables among four groups: rapid cycling with bipolar I, rapid cycling with bipolar II, nonrapid cycling with bipolar I, and nonrapid cycling with bipolar II. When examining the association of these groups to discrete variables (e.g., patient sex), the chi-square test was used. If cell sizes were too small (fewer than 5), Fisher’s exact test was substituted. The generalized linear model was used when examining the effects of rapid-cycling status, lifetime diagnosis, and their interaction in predicting continuous variables (e.g., Montgomery-Åsberg Depression Rating Scale or Young Mania Rating Scale scores). Logistic regression was used when examining the effects of these predictor variables on discrete outcome variables (e.g., substance abuse status). For comorbidity items, data collection procedures for 4.5% of the participants failed to meet project quality-assurance standards. Data from these participants were excluded from analyses.
Results
Prevalence of Rapid Cycling
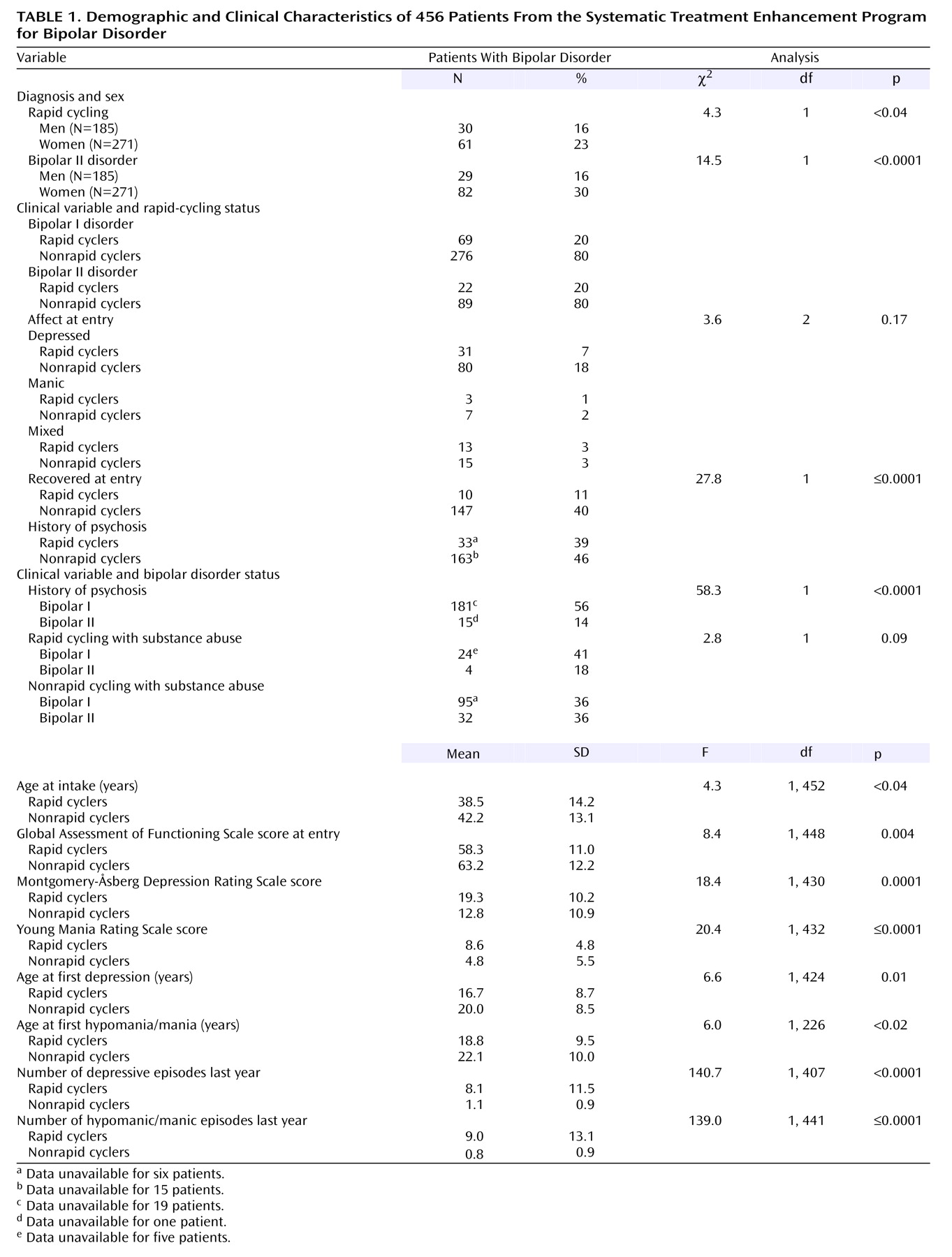
Of the first 500 patients enrolled in the Systematic Treatment Enhancement Program, 483 (96.6%) were diagnosed with either bipolar I or bipolar II disorder. The remaining 17 patients were diagnosed with either bipolar disorder not otherwise specified (N=14, 2.8%), schizoaffective disorder (bipolar type) (N=2, 0.4%), or other (N=1, 0.2%). Data regarding the frequency of mood episodes was unavailable for 44 patients (8.8%) from the original 500 from the Systematic Treatment Enhancement Program, and consequently, these patients were excluded from the present study. Of the 456 patients included in the present group, 345 (75.7%) were diagnosed with bipolar I disorder, and 111 (24.3%) were diagnosed with bipolar II disorder (
Table 1).
Applying DSM-IV rapid-cycling criteria to patients with data from the year before study entry revealed that 91 (20.0%) had a rapid-cycling condition, whereas 365 (80.0%) did not. As a check on the validity of the rapid-cycling designation, we examined the raw frequency of episodes in the prior year. Rapid cyclers experienced approximately eight times the number of depressive episodes (mean=8.1, SD=11.5, versus mean=1.1, SD=0.9, respectively) and nine times the number of hypomanic/manic episodes (mean=9.0 episodes, SD=13.1, versus mean=0.8 episodes, SD=0.9) in the year before study entry compared to their nonrapid-cycling counterparts (F=139.0, df=1, 441, p≤0.0001). A significant interaction was found between rapid-cycling status and bipolar I/II status on the number of depressive episodes in the last year. Rapid-cycling bipolar II patients had more depressive episodes than nonrapid-cycling bipolar II patients, but this difference did not extend to bipolar I patients (F=4.5, df=1, 407, p<0.04).
Patients with bipolar I and bipolar II disorders did not differ in rapid-cycling frequency. Of 345 bipolar I patients, 69 (20.0%) were found to have rapid cycling, compared to 22 (19.8%) of 111 bipolar II patients (χ2=0.0, df=1, p=0.97).
Rapid-Cycling Status and Demographic Variables
Of the 456 patients, 185 (40.6%) were men and 271 (59.4%) were women. A logistic regression model examined whether men and women were disproportionately represented in the bipolar I versus II groups or in the rapid cycling/nonrapid-cycling group designations. The main effects of bipolar I/II status, rapid-cycling status, and their interaction were entered as predictors of gender. Rapid-cycling status was related to female gender (χ2=4.3, df=1, p<0.04); 61 (23%) of 271 women were rapid cyclers, whereas 30 (16%) of 185 men were so designated. The model also revealed a main effect of bipolar I/II status, indicating that women were almost twice as likely to have bipolar II disorder (82 of 271, 30%) (χ2=14.5, df=1, p<0.0001) as men (29 of 185, 16%). Finally, an interaction between bipolar I/II status and rapid-cycling status approached but did not reach significance (χ2=2.7, df=1, p=0.10). This interaction suggested that the preponderance of women in the rapid-cycling category was more pronounced among bipolar I than bipolar II patients.
Rapid-cycling patients were significantly younger upon entry into the Systematic Treatment Enhancement Program than nonrapid-cycling patients by nearly 4 years (mean=38.5 years, SD=14.2, versus mean=42.2 years, SD=13.1) (F=4.3, df=1, 452, p<0.04). No differences were found between the two groups with regard to marital status: rapid cyclers were equally likely to be single, married, separated/divorced, or widowed as nonrapid-cycling patients.
Rapid Cycling and Illness Severity
A total of 149 patients entered the Systematic Treatment Enhancement Program for Bipolar Disorder during an active episode (111 depressed [24.0%], 10 manic [2.2%], and 28 mixed [6.2%]). The polarity of the index study episode was not associated with rapid-cycling status (χ2=3.6, df=2, p=0.17). The relation of bipolar I/II status to the polarity of the index episode approached significance (χ2=5.6, df=2, p=0.06). This difference was explained by the lack of manic patients in the bipolar II cell (N=0).
Rapid-cycling patients were more ill upon study entry than nonrapid-cycling patients. The mean Global Assessment of Functioning Scale score on study entry was 58.3 (SD=11.0) in the rapid-cycling group, compared to 63.2 (SD=12.2) in the nonrapid-cycling group (F=8.4, df=1, 448, p=0.004). Rapid cyclers also had higher scores on both the Montgomery-Åsberg Depression Rating Scale and the Young Mania Rating Scale at entry into the study. The mean depression score on the Montgomery-Åsberg Depression Rating Scale for rapid cyclers was 19.3 (SD=10.2) (score of 0–8=recovered, 9–17=mild, 18–34=moderate) compared to 12.8 (SD=10.9) in the nonrapid-cycling group (F=18.4, df=1, 430, p=0.0001). At the same time, on the Young Mania Rating Scale (score of 0–9=normal, 10–12=subsyndromal), rapid cyclers (mean=8.6, SD=8.2) scored higher than the nonrapid-cycling patients (mean=4.8, SD=5.5) (F=20.4, df=1, 432, p<0.0001). Far fewer rapid-cycling patients appeared to be “recovered” (N=10, 11.0%) at study entry than the nonrapid-cycling patients (N=147, 40.4%) (χ2=27.8, df=1, p≤0.0001).
Rapid-cycling patients began cycling at an earlier age than nonrapid cyclers. The mean age of first depression was 16.7 years (SD=8.7) in the rapid-cycling patients, compared to 20.0 years (SD=8.5) in nonrapid-cycling patients (F=6.6, df=1, 424, p=0.01). Rapid cyclers experienced a first hypomanic/manic episode at a mean of 18.8 years (SD=9.5) compared to 22.1 years (SD=10.0) in the nonrapid-cycling patients (F=6.0, df=1, 446, p<0.02).
Rapid cycling was not related to past psychotic episodes. Thirty-three (38.8%) of 85 rapid-cycling patients (data unavailable for six patients) reported psychosis at some time in their lives, while 163 (46.4%) of 351 nonrapid-cycling patients (data unavailable for 15 patients) had experienced a past psychotic episode (χ2=1.6, df=1, p=0.21). When subdivided into bipolar I versus bipolar II disorder groups, lifetime history of psychosis was more frequent among bipolar I patients (181 of 326, 55.5%) than bipolar II patients (15 of 110, 13.6%) (χ2=58.3, df=1, p<0.0001).
Lifetime diagnosis of bipolar I versus II disorders did not have a significant effect on the likelihood of being a substance abuser (χ2=0.0, df=1, p=0.96) nor did rapid-cycling status (χ2=2.41, df=1, p=0.12. An interaction between rapid-cycling and bipolar I/II status approached but did not reach significance (χ2=2.81, df=1, p=0.09). Specifically, 24 (41%) of 59 rapid-cycling bipolar I patients were substance abusers, whereas only four (18.2%) of 22 rapid-cycling bipolar II patients were so designated. Rates of substance abuse in nonrapid-cycling patients were equivalent for bipolar I (95 of 262, 36%) and bipolar II (32 of 89, 36%) patients.
Discussion
The present study examined the clinical correlates of rapid cycling in a large group of bipolar patients (N=456). The prevalence of rapid cycling in our group was 20%, a proportion consistent with the majority of other studies examining rapid cycling in selected bipolar populations (13%–56%)
(2–
4,
6,
8,
9).
Not surprisingly, rapid-cycling patients had a greater severity of illness than nonrapid-cycling patients. Although, by definition, the rapid-cycling group should have experienced more episodes in the prior 12 months than the nonrapid-cyclers, the magnitude of the difference in cycle frequency was impressive. The rapid-cycling patients experienced nearly eight times the number of depressive and nine times the number of hypomanic/manic episodes as the nonrapid-cycling patients. Moreover, the rapid-cycling cohort had worse mood states at study entry. Both Young Mania Rating scores and Montgomery-Åsberg Depression Rating Scale scores were significantly higher in the rapid-cycling group.
Patients with and without rapid cycling were equally likely to be in a manic, mixed, or depressed episode at study entry. When considering the issue of clinical significance, the higher Montgomery-Åsberg Depression Rating Scale scores in the rapid-cycling group indicated a “moderate” level of depression, whereas the scores of the nonrapid cyclers were consistent with a “mild” level of depression
(16). The prominence of depressive symptoms, in both frequency and severity, is consistent with prior reports that have described depression as the hallmark of rapid-cycling bipolar disorder
(13).
In contrast to earlier studies, we found that rapid cyclers were younger at study entry and that their bipolar disorder appeared at a younger age. The majority of prior studies have found either no average age difference between rapid- and nonrapid-cycling patients
(6,
10) or that rapid cyclers were older
(2,
3). Additionally, previous studies examining the onset of bipolar disorder have found either no differences between rapid and nonrapid cyclers
(1,
4,
8,
10) or that rapid cyclers were older when their symptoms began
(9). However, the younger age at onset in our rapid-cycling group is consistent with recent findings by Coryell et al.
(17). The poor outcomes observed among adult patients with rapid cycling mirror the outcomes of childhood and early adolescent bipolar patients
(18). If early-onset bipolar illness confers a liability to rapid cycling, early, aggressive pharmacological or psychosocial intervention may be a means of enhancing long-term outcome.
Consistent with prior studies, women were more likely to be rapid cyclers (23%) than men (16%). Previous explanations for this association include women’s increased risk for hypothyroidism
(10) and gonadal steroid effects
(19). However, evidence is limited for both of these explanations
(20–
23). Alternate explanations include the primacy of major depressive symptoms (more common among women) in anticipating later rapid cycling
(6). This explanation is consistent with more recent work by Maj et al.
(24), who found that patients who have polyphasic episodes are more likely to have poor symptomatic outcomes, especially if the first episode is depression. Furthermore, a recurrent pattern of depression often necessitates the use of adjunctive antidepressants, which in turn can provoke rapid cycling
(20). As bipolar women experience more depressive symptoms than men over the course of their illness
(25), they may be more vulnerable to rapid cycling and/or the possible cycling effects of antidepressant exposure. Future studies that examine the interactive effects of gender, prior depression history, and antidepressant exposure may help clarify the pathways to rapid cycling among women.
In contrast to earlier studies
(4,
6,
7,
9), we found that rapid-cycling patients were as likely to suffer from bipolar I as bipolar II disorder. This lack of association was also found by Dunner et al.
(4), Maj et al.
(3), and most recently, Coryell et al.
(17). The inconsistent association of rapid cycling and bipolar II disorder across different studies may reflect the heterogeneous patient populations, varying definitions of rapid cycling, and different criteria used to diagnose bipolar I and bipolar II disorder. Indeed, since Dunner and Fieve’s rapid-cycling study in 1974
(8), at least seven different definitions of rapid cycling have been used in studies. Rapid-cycling definitions prior to DSM-IV frequently recommended shortening the length of time required to define a mood episode, shortening the length of euthymia needed to describe mood episodes as distinct, or both. The DSM-IV definition used in our study is the most specific but possibly the least sensitive
(2), which may account for some of the differences noted between our present study and previous ones.
Our study revealed that psychosis, a marker of illness severity, was more strongly associated with bipolar I than bipolar II disorder but not a rapid-cycling course. This suggests that the increased morbidity of rapid cycling is more a consequence of the mood instability itself and not because rapid cyclers are more frequently psychotic. Only two previous studies have reported on the lifetime prevalence of psychosis in rapid-cycling patients. Our findings are similar to those reported by Bauer et al.
(1), who found no significant difference in the frequency of psychosis between rapid- (40%) and nonrapid-cycling patients (48%). In contrast, Wehr et al.
(20) found that 70% of rapid-cycling patients had experienced psychosis, although they did not examine a nonrapid-cycling cohort. Our data suggest that rapid cycling and psychosis are likely independent pathological mechanisms affecting the severity of bipolar disorder.
Finally, we examined the association between rapid cycling and substance abuse. There are considerable data suggesting that comorbid substance abuse worsens the prognosis of bipolar disorder, possibly by worsening compliance with medication
(26). Our data suggested that rapid-cycling bipolar I patients are more likely to abuse alcohol and drugs than rapid-cycling bipolar II patients, an effect that approached but did not achieve statistical significance. Our findings are similar to those of Calabrese and colleagues
(13), who reported that 69% of 105 rapid-cycling patients with comorbid substance abuse had bipolar type I, whereas 31% of rapid-cycling patients with substance abuse had bipolar type II. The data are also consistent with the lifetime prevalence study data from the Epidemiologic Catchment Area reported by Regier et al. in 1990
(27), showing that bipolar I patients carried a higher risk of substance abuse (odds ratio=7.9) compared to bipolar II patients (odds ratio=4.7). Our data do not clarify whether substance abuse is causative or ameliorative in nature. Are substances more likely to induce or exacerbate rapid cycling, or do rapid-cycling patients abuse substances in an effort to ameliorate their symptoms? We also did not examine what types of substances were used and whether or not the type of drug is associated with a particular phase of the illness. Nonetheless, this is the first time that a possible link has been shown between increased likelihood of abusing substances and the rapid-cycling bipolar variant.
Several limitations of our results deserve comment. As noted previously, the Systematic Treatment Enhancement Program for Bipolar Disorder is based at academic, specialty, and tertiary care sites across the United States and thereby attracts a more select population than might be found in the general community. The population of the Systematic Treatment Enhancement Program for Bipolar Disorder is a largely middle- to upper-middle-class cohort, which may limit the application of our findings to different population subgroups. In addition, we were unable to verify the presence of rapid cycling prospectively, although this limitation applies to the majority of the literature in this field. Finally, we were not able to examine the effects of antidepressants, either by type of antidepressant or total antidepressant exposure in the onset of rapid cycling or mixed states. However, in this study, knowing the number or types of antidepressants used in the prior year would not have clarified whether antidepressants induced or worsened cycling or whether a patient was cycling and antidepressants were given. Prospective follow-up of the Systematic Treatment Enhancement Program cohort will help to clarify these cause-and-effect relationships.
In summary, this study is consistent with prior reports describing the phenomenology of bipolar disorder accompanied by a rapid-cycling presentation. These patients experience a greater severity of illness than their nonrapid-cycling counterparts, with depressive symptoms appearing most prominent. Despite the numerous reports now describing this course modifier, there are few prospective randomized controlled trials examining the efficacy of psychotropic agents among these treatment-refractory patients
(5). Our findings support the need for additional randomized, controlled clinical trials in rapid-cycling bipolar disorder, with particular emphasis on treatment of the depressed phase. Our findings also suggest that examining treatment response by moderators such as gender, bipolar I versus II status, and age at illness onset may be useful in clarifying which subgroups are more or less likely to respond to a given treatment. In particular, studies exploring the use of a single mood stabilizer versus combination mood stabilizers, the role of atypical antipsychotic agents either as augmentation or monotherapy, and the role of bipolar-specific psychotherapies are all areas in need of further exploration.