A psychiatric advance directive is a legal document that allows a patient to consent to or refuse future mental health treatment in the event of an incapacitating psychiatric crisis by documenting advance instructions or appointing a surrogate decision maker
(1) . Laws on psychiatric advance directives were intended to support patients’ self-determination at times when they are particularly vulnerable to loss of autonomy, to help them ensure that their preferences are known, and to minimize unwanted or involuntary treatment
(2,
3) . Advocates for psychiatric advance directives hope that the very process of preparing these documents will enhance patients’ sense of trust and collaboration with providers, thereby improving the therapeutic alliance and engagement with treatment
(4,
5) .
Structured facilitation to complete a psychiatric advance directive, in the form of a collaborative exercise between the patient with severe mental illness and a clinician or independent advocate, could provide an opportunity for respectful dialogue on the patient’s past treatment experiences and preferences for future treatment. Such a process could yield benefits beyond the original legislative intent of statutes on psychiatric advance directives. By validating the patient’s treatment experiences, preferences, and instructions in a legal document and by fostering personal investment in shared decisions about future treatment, the process of planning ahead for illness contingencies may motivate the patient to greater levels of participation and engagement in regular outpatient services. In turn, as patients become more actively engaged in their treatment and more involved in managing their illness and directing their own care, a more productive working relationship between patient and clinician may develop, and ultimately services may become more effective and more satisfactory. Whether psychiatric advance directives will achieve these proposed benefits is largely unknown.
There is growing interest in psychiatric advance directives, and 25 states have authorized such directives in new statutes or amended health care decision laws. However, little is known about how states can effectively implement these instruments. Studies suggest that, if given the choice and necessary assistance, one-half to two-thirds of patients with severe mental illness would complete a psychiatric advance directive
(6 –
10) . Yet, only 4%–13% of outpatients receiving public sector mental health treatment indicate that they have executed a psychiatric advance directive
(9,
10) .
The gap between interest in and completion of psychiatric advance directives is due in part to the substantial barriers facing patients as well as their clinicians. Patients report barriers such as difficulty in understanding advance directives, skepticism about their benefit, lack of contact with a trusted individual who could serve as proxy decision maker, and the sheer complexity of filling out the legal forms, obtaining witnesses, having the documents notarized, and filing the documents in a medical record or registry
(9) . Clinicians report system-level barriers, including lack of access to the documents in a crisis, lack of staff training on psychiatric advance directives, lack of communication between staff across different components of mental health systems, and lack of time to review the advance directive documents
(11) .
This study addresses several questions:
Can structured facilitation overcome major barriers to implementation of psychiatric advance directives and increase rates of completion?
What patient characteristics predict completion of a psychiatric advance directive?
What are the structure and content of psychiatric advance directives resulting from the facilitation process?
What impact do psychiatric advance directives have on the working alliance between patients and clinicians and on patients’ receipt of needed mental health services?
These questions are examined in a randomized controlled trial of a structured, manualized facilitation intervention for psychiatric advance directives.
Method
Screening, Sample Selection, Recruitment, and Randomization
The study protocol was approved by the institutional review boards of Duke University Medical Center and the participating programs and hospital. We planned to enroll approximately 500 patients from two county-based public mental health systems in the north-central region of North Carolina, a racially diverse, mixed urban-rural area. To increase the study’s generalizability to severely mentally ill patient populations at high risk of relapse and decisional incapacity, the sample was stratified so that approximately 20% of participants received the intervention shortly after discharge from the hospital following an acute inpatient admission. To be eligible, participants had to be 18 to 65 years of age; have a chart diagnosis of schizophrenia, schizoaffective disorder, other psychotic disorder, or major mood disorder with psychotic features; be currently receiving community-based treatment through one of two county-based programs in the north-central region of North Carolina; and be able to give informed consent to participate in the study.
A random sample was drawn from deidentified lists of mental health program clients prescreened for eligibility. Sequential admissions from the programs to the regional state psychiatric hospital were also screened. Treating clinicians verified that identified patients met study criteria and sought the patients’ permission to be contacted by a researcher. Patients willing to be contacted were approached by a research interviewer. After providing informed consent and completing a baseline interview, each participant was randomly assigned to either the facilitated psychiatric advance directive intervention or the control group. For participants assigned to the facilitated intervention group, a session to conduct the intervention was scheduled as soon as possible after the baseline interview.
Intervention
The facilitated psychiatric advance directive intervention was a semistructured, manualized interview and guided discussion of choices involved in anticipatory mental health treatment planning. It was adapted from several medical and psychiatric advance directive planning tools
(12 –
14), and it incorporated the required elements of psychiatric advance directives in North Carolina statutes. In North Carolina, persons may while competent create an “advance instruction for mental health treatment” (North Carolina General Statute [NCGS], chap. 122C-73–77) specifying preferences and instructions for their mental health treatment during a future period of decisional incapacity. Statutes also allow persons to appoint a proxy decision maker with a health care power of attorney (NCGS, chap. 32A). The instructional directive and health care power of attorney may be completed as stand-alone documents, or both documents may be completed as mutually reinforcing legal instruments.
The intervention includes orientation to concepts related to psychiatric advance directives, review of past treatment experiences, and documentation of future treatment preferences. The core of the intervention is a semistructured interview and guided discussion of choices involved in planning for mental health care during future periods of incapacity. If the participant wishes to prepare the relevant legal psychiatric advance directive documents, the facilitator helps with completion of the forms. The specific sections of the advance instruction and health care power of attorney statutory forms (e.g., medication choices, facilities preferences, and powers granted to or withheld from the health care agent) are used to organize and guide discussion of the participant’s preferences. The facilitator also helps the participant obtain witnesses, get documents notarized, and file forms in the medical record and an electronic registry.
The intervention was conducted by five trained research assistants, one with a master’s degree and the others with bachelor’s degrees. They were trained to fidelity by a doctoral-level clinical psychologist until they consistently achieved a score of at least 87% on 15 fidelity criteria. Reliability and fidelity were then monitored by random observation and fidelity measurement, with remediation as needed.
Control Condition
At the conclusion of the baseline interview, participants assigned to the control group were individually given an introduction to psychiatric advance directives, written materials describing the purpose of advance directives, copies of standard forms for psychiatric advance directives, and the toll-free telephone number of the local consumer organization that provides consultation to persons who wish to prepare psychiatric advance directives. Subjects with poor literacy skills had the materials read to them aloud. Control group participants were not given any help with contacting the consumer organization or with filling out the advance directive forms.
Measures
Attitudes, Barriers, and Competence
We asked participants to rate the usefulness of psychiatric advance directives and to specify potential problems they perceived in effective implementation of advance directives. To measure competence, we used the Decisional Competence Assessment Tool for Psychiatric Advance Directives, which is an abbreviated, simplified version of a previously developed instrument, the Competence Assessment Tool for Psychiatric Advance Directives
(15), which was in turn modeled on the MacArthur Competency Assessment Tool for Treatment
(16) . Like these previous instruments, the Decisional Competence Assessment Tool for Psychiatric Advance Directives assesses four dimensions of competence: understanding, appreciation, reasoning, and choice. Specifically, it measures ability to understand key components of psychiatric advance directives, appreciate the relevance of advance directives to treatment, reason about how such directives may affect one’s life, and choose whether to complete a psychiatric advance directive.
Descriptive Content Analysis
Research assistants coded the instructional content of completed psychiatric advance directives in 10 categories: crisis symptoms, medications, hospitalization, emergency contact information, relapse risk factors, protective factors, response to hospitalization, instructions to hospital staff, ECT preferences, and other instructions or medical information on side effects or allergies to medications.
Evaluative Content Analysis
A rating scale was developed by study clinicians with long-standing experience with community practice standards in North Carolina. Completed psychiatric advance directives were rated for congruity with community standards of care, clinical feasibility, and usefulness of clinical information, taking into account diagnosis, local practice standards, and local health care resources. Raters were two psychiatrists blind to study assignment and trained to reliability (kappa=0.71).
Short-Term Outcome Variables
Short-term outcomes were measured in terms of 1-month change in quality of working alliance and perception of whether need for mental health treatment was met. The short form of the Working Alliance Inventory, adapted for use with individuals with severe mental illness
(17,
18), was administered. Perception of whether need for treatment was met was measured operationally by a face-valid item from the Mental Health Statistics Improvement Program Consumer Survey index of treatment satisfaction
(19) : “[In the past month] I was able to get all the services I thought I needed.” Participants whose response to this question was “agree” or “agree strongly” were coded as positive on the perception that their need for mental health treatment was met. Missing values on these items were imputed as neutral scores.
Independently of our 1-month follow-up interviews with participants, we also tracked whether participants had completed psychiatric advance directives by 2 months after baseline.
Other Covariates
Independent variables were selected for analysis on the basis of prior studies of the correlates of psychiatric advance directives
(10,
20) . We dichotomized covariates if warranted by their distribution or nonlinear association with the outcomes.
Social contact and support were measured with items modified from the Duke Social Support Index
(21) . The anchored version of the Brief Psychiatric Rating Scale (BPRS)
(22) was used to assess current psychiatric symptoms. The Global Assessment of Functioning scale (GAF)
(23) was used to measure functional impairment. The Insight and Treatment Attitudes Questionnaire
(24) was used to measure awareness of mental health problems and acknowledgment of past, current, and future need for treatment. Substance abuse was assessed with questions adapted from the Michigan Alcoholism Screening Test
(25) and the Drug Abuse Screening Test
(26) . Motivation to enter and participate in treatment was measured by the Treatment Motivation Questionnaire
(27,
28) as adapted for persons with severe mental illness. This instrument assesses internal motivation for treatment, motivation related to belief in the goals of treatment, confidence in treatment, and inclination to interpersonal help seeking. Perceived coercion was measured with the MacArthur Perceived Coercion Scale, adapted for reference to outpatient treatment
(29) . The Drug Attitude Inventory
(30) was used to assess participants’ attitudes toward taking psychotropic medications. We reverse-coded this instrument so that high scores indicated low perceived benefit and more adverse effects. We assessed participants’ lifetime experiences of leverage in outpatient treatment
(20) —use of representative payeeship, housing supports contingent on treatment adherence, criminal sanctions requiring treatment, and involuntary outpatient commitment.
Statistical Analysis
Logistic regression analysis was used to examine the net effects several domains of the variables mentioned above had on completion of psychiatric advance directives: demographic and socioeconomic characteristics, clinical and functional predictors, services and system utilization, leverage and coercion-related experiences in past mental health treatment, perceived barriers to completion of a psychiatric advance directive, and attitudes about the benefits and drawbacks of psychiatric advance directives. We tested each variable and domain separately, then derived a final multivariable model using stepwise selection at p<0.10.
Logistic regression was also used to examine the impact of the intervention on whether participants reported at 1-month follow-up that their need for mental health treatment was met. Linear regression analysis was used to examine the relative impact of the intervention on Working Alliance Inventory score at 1 month, controlling for baseline score.
Results
Screening and Enrollment
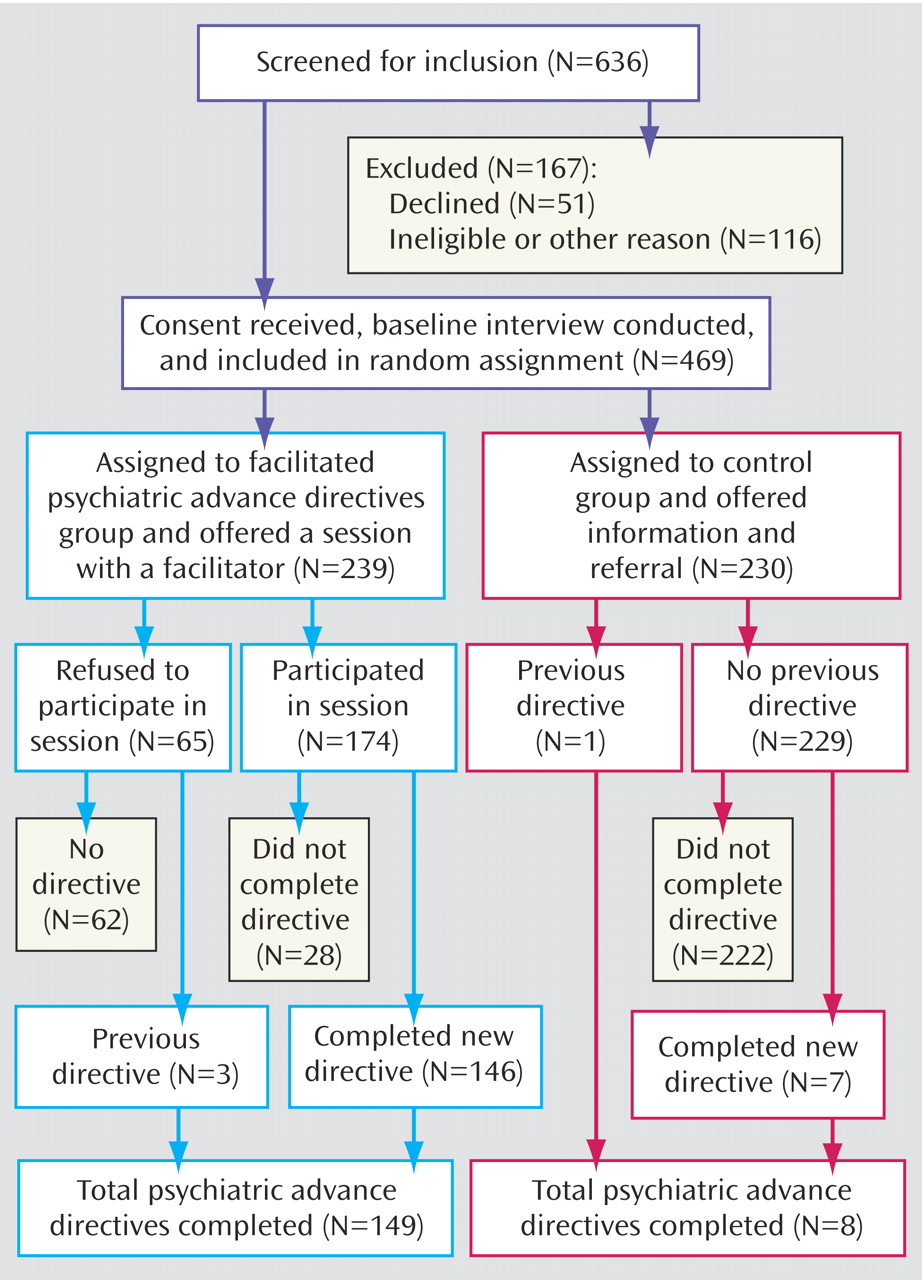
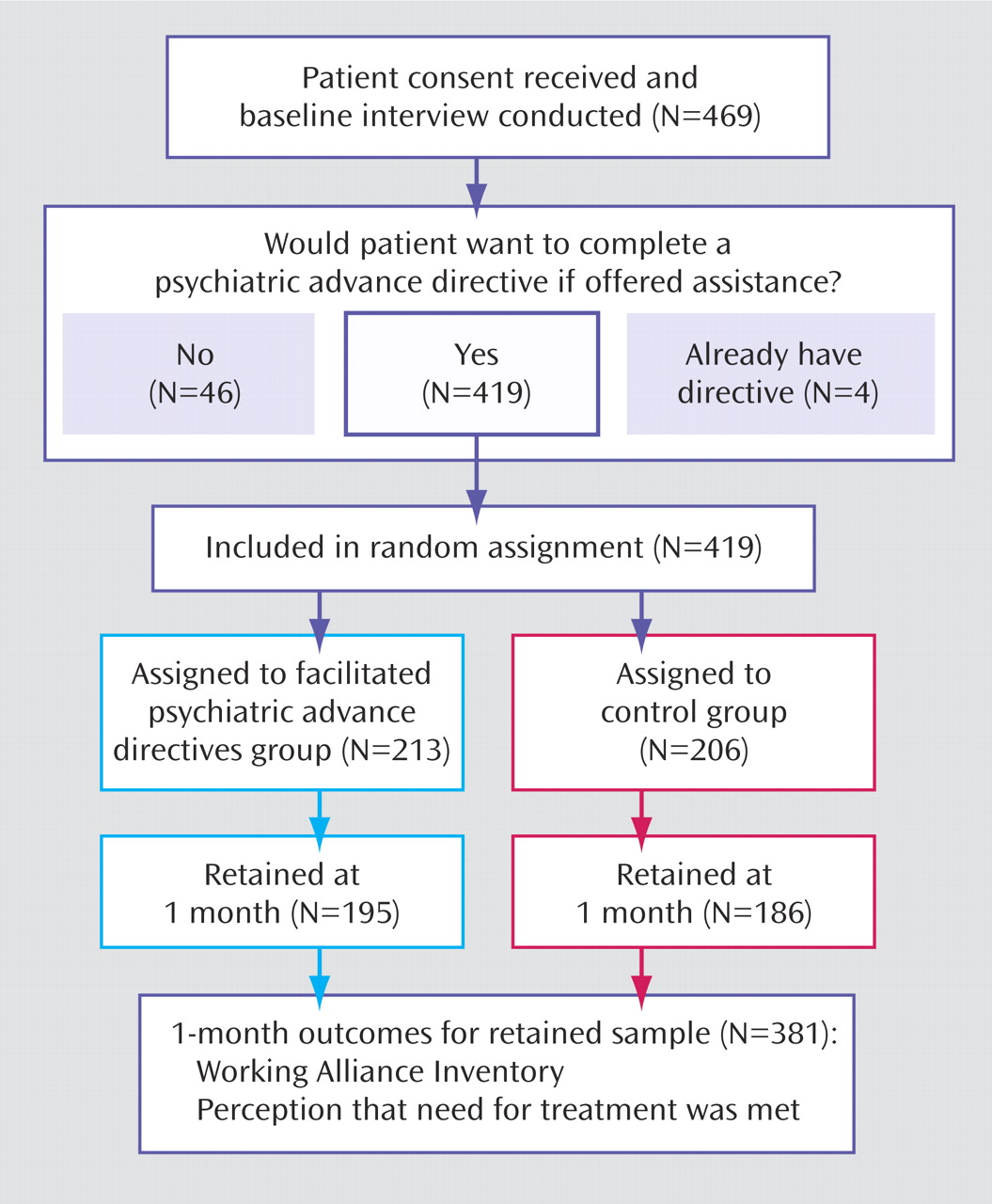
As
Figure 1 shows, 636 patients were screened for the study—254 and 249 patients, from the two county-based public outpatient mental health programs, and 133 patients admitted to a regional state psychiatric hospital from these programs. Of those screened, 116 (18%) were excluded because they did not meet eligibility criteria, were too ill, or could not be located, or for other reasons. The remaining 520 patients were approached in person and asked if they wished to participate in the study. Of those, 51 (10%) declined to enroll in the study, resulting in a sample of 469 patients. Seventy-nine participants (17%) were recruited for the hospital subsample.
After the baseline interview, 239 participants were randomly assigned to the intervention group and 230 to the control group. There were no significant demographic or clinical differences between the intervention and control groups at baseline. Attrition at 1-month follow-up was 9.4%, and no significant differences in attrition rate were found between the study groups.
Sample Characteristics
Participants’ average age was 42 years (SD=10.7). The sample was 60% female, 58% African American, 39% white, and 3% from other racial backgrounds. Only 11% were married or cohabiting. Twenty-eight percent of the sample had less than a high school education. At the time of enrollment, 57% of participants were living independently. Only 23% of participants had worked for pay in the past month.
Fifty-nine percent of participants had a chart diagnosis of schizophrenia or a related psychotic disorder, 27% had a diagnosis of bipolar disorder, and 14% had a diagnosis of depression with psychotic features. Ten percent had a concurrent chart diagnosis of a substance use disorder. The mean score on the BPRS was 33.6 (SD=9.2), indicating moderate symptom severity. The mean score on the GAF was 40.0 (SD=10.3), consistent with moderate functional impairment. The mean score on the Insight and Treatment Attitudes Questionnaire was 18.1 (SD=4.3), indicating reasonably high awareness of illness and the need for treatment. Overall, 72% of participants reported at least one outpatient visit during the past month, and 35% had been hospitalized for a psychiatric disorder in the previous 6 months.
About two-thirds (68%) of participants reported lifetime experiences of involuntary intervention in connection with a past hospitalization, such as being handcuffed by police for transport to the hospital, receiving forced medication, or being placed in physical restraints or seclusion. Nearly half (48%) reported having experienced leveraged community treatment, and one-quarter (24%) were currently subject to leveraged treatment. More than one-third (38%) of participants reported experiences in which they felt the need to be hospitalized but were not admitted.
Intervention Sessions
The median length of time between baseline and completion of the intervention was 21 days; 70% were completed within 1 month. Twenty-seven percent of participants who were assigned to the intervention group refused the intervention and did not meet with the facilitator. Of the participants who met with the facilitator, most (84%) completed a legally valid psychiatric advance directive within 2 months after baseline. On average, intervention sessions took 120 minutes to complete.
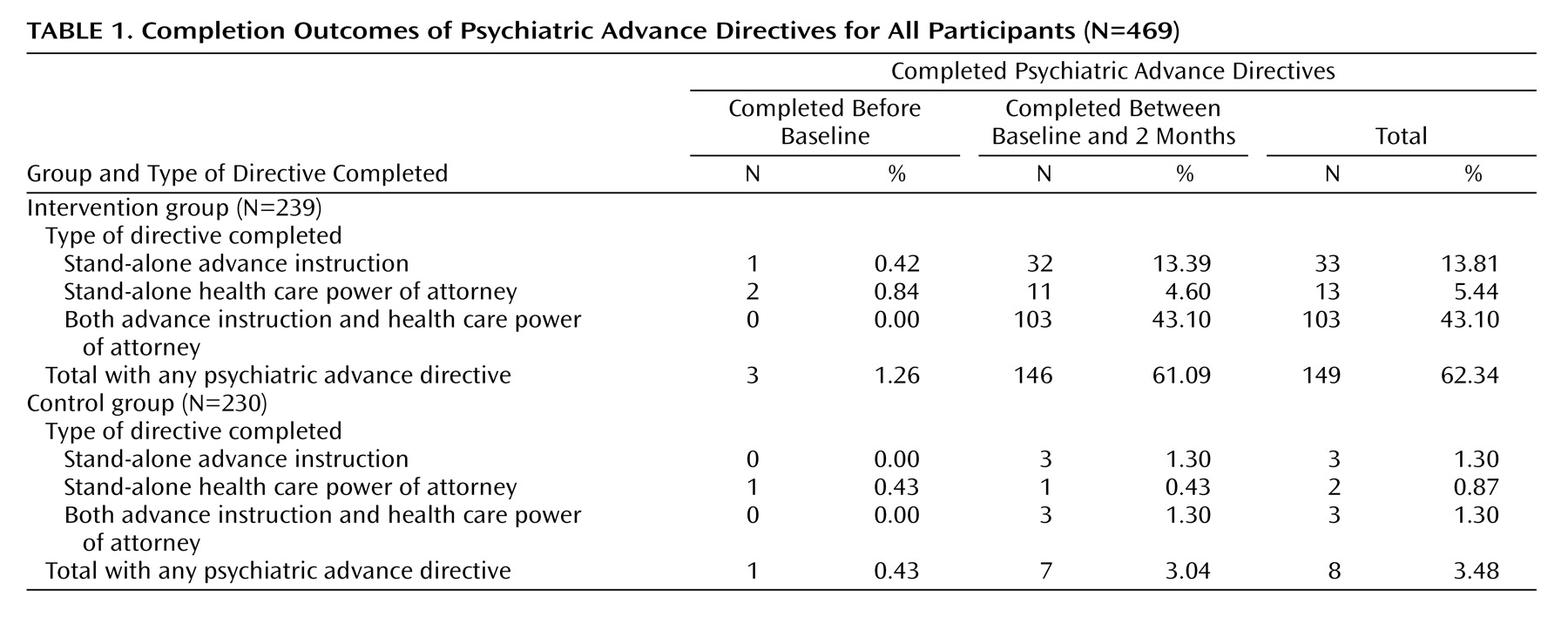
Completion of Psychiatric Advance Directives
Table 1 presents the primary results of the experiment. At baseline, three participants in the intervention group and one in the control group had already completed psychiatric advance directives. By 2 months from enrollment date, 61% of participants in the intervention group had completed a psychiatric advance directive, compared with only 3% in the control group. In the intervention group, 13% completed a stand-alone advance instruction, 5% completed a stand-alone health care power of attorney, and 43% completed both legal documents. Participants in the intervention group were far more likely to complete both components of a psychiatric advance directive—the instructional directive (56.5% versus 2.6%, p<0.001) and health care power of attorney (47.7% versus 1.7%, p<0.001).
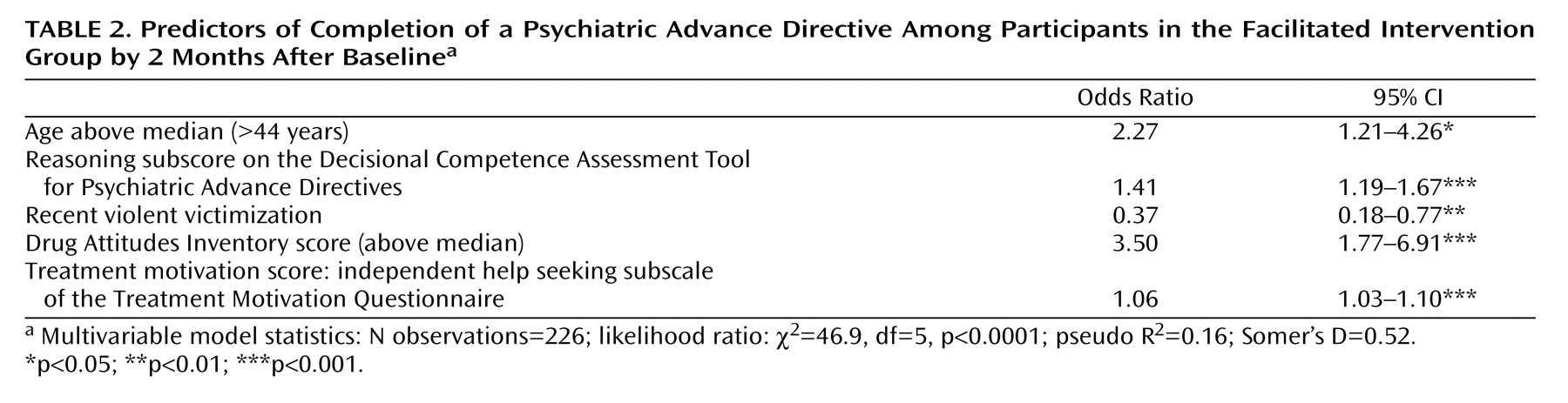
Predictors of Completion in the Intervention Group
Table 2 presents the final model of psychiatric advance directive completion in the intervention group. Significant net positive predictors included age, reasoning subscore on the Decisional Competence Assessment Tool for Psychiatric Advance Directives, a score on the Drug Attitude Inventory indicating adverse medication experience, and the Treatment Motivation Questionnaire’s subscale measuring independently motivated help seeking. The sole negative predictor was recent history of violent victimization.
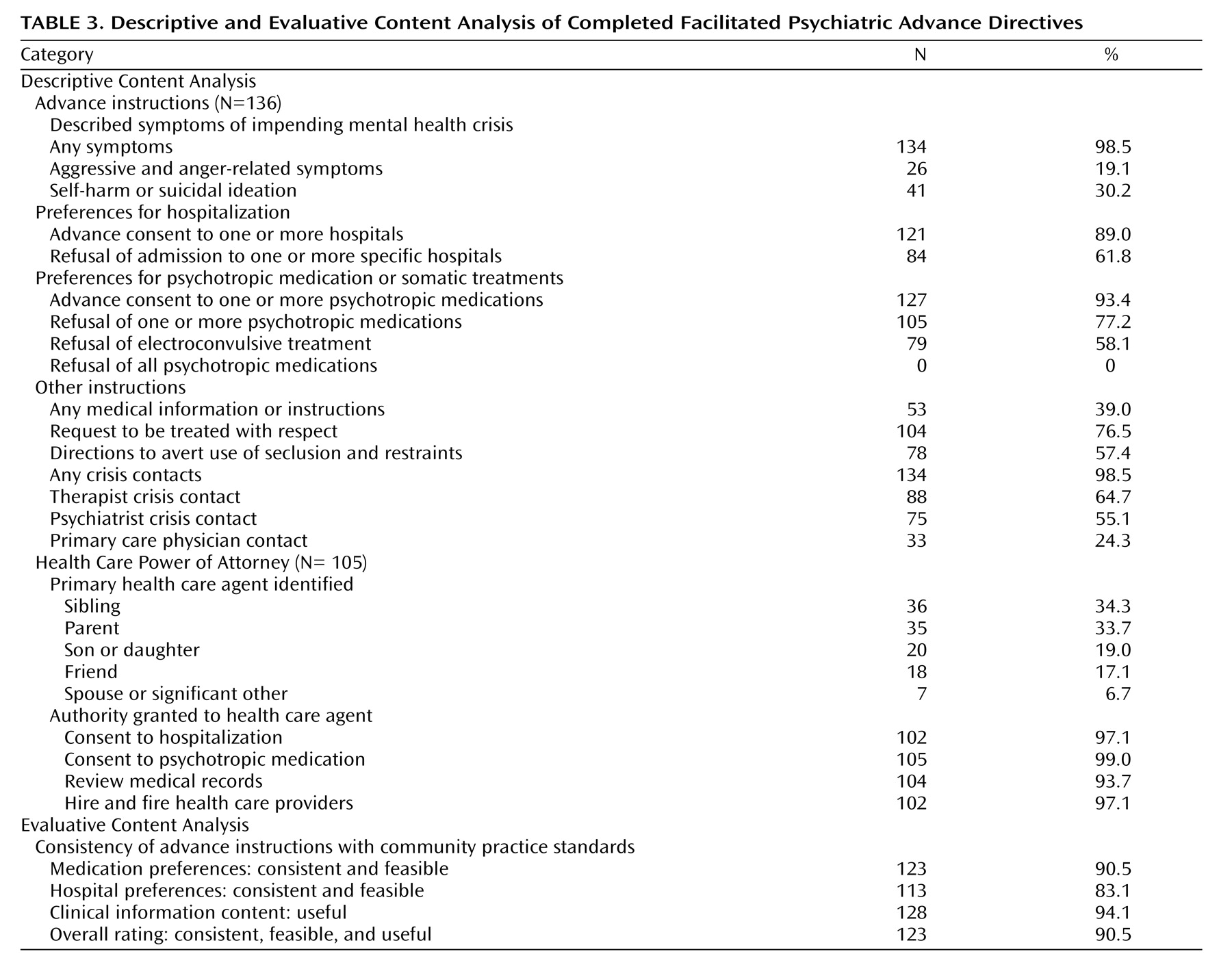
Descriptive Content Analysis
Table 3 presents a descriptive analysis of completed facilitated psychiatric advance directives. In the control group, too few advance directives were completed to allow statistical analysis; only seven control participants completed directives, and five of these participants did not respond to our requests for a copy of the documents. The two sets of documents that we were able to review had legal deficiencies, such as not being witnessed or notarized or appointment of a person as health care agent who would be statutorily disqualified for that role.
A large majority (89.0%) of completed psychiatric advance directives from participants in the intervention group included advance agreement to hospitalization in at least one specified inpatient facility, and 61.8% documented advance refusals of admission to particular hospitals. Ninety-three percent of directives gave advance consent to treatment with at least one specified psychotropic medication, and 77% included refusal of some medications. No participant refused all medications or treatment.
Completed advance directives authorized a variety of types of individuals as substitute decision makers with health care power of attorney, typically giving them broad authority to act in the event that the person loses capacity, including power to consent to hospitalization (97.1%), approve treatment with medications (99.0%), read the medical record (93.7%), and hire and fire the person’s health care provider (97.1%).
Evaluative Content Analysis
Study psychiatrists’ blinded ratings of instructions in the documents for advance instruction for mental health treatment showed high consistency with community practice standards in North Carolina. Medication preferences were rated as feasible and consistent with community practice standards (90.5%). Similarly, hospital preferences were rated as feasible and consistent (83.1%) and clinical information as clinically useful (94.1%). Global ratings of the documents indicated high feasibility, congruity with community practice standards, and useful information (90.5%).
Analysis of the Intervention’s Effects on 1-Month Outcomes
Figure 2 presents a diagram of the study’s design for examining additional outcomes at 1-month follow-up. This analysis was limited to participants in both arms of the study who had not already completed a psychiatric advance directive before baseline and indicated at baseline that they wished to complete one. The potential effect of selection bias associated with completion of advance directives would thus be minimized, allowing examination of the effects of completing a psychiatric advance directive while retaining the integrity of the randomized study design. Eighty-nine percent of the sample indicated that they would want to complete a psychiatric advance directive if given the opportunity. Thus, the control group was matched with the intervention group with respect to baseline psychiatric advance directive status and initial inclination to complete such a directive. All analyses reported in this section were examined for site effects, site-by-intervention effects, and site-by-covariate interaction effects. No site effects were found.
As shown in
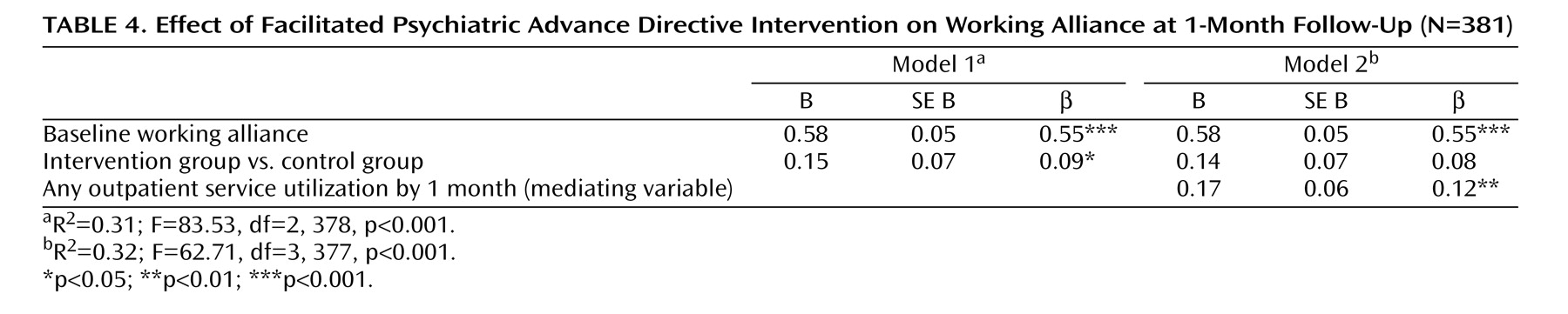
Table 4, we used regression analysis to examine the net effect of the intervention at 1-month follow-up on working alliance, controlling for outpatient service utilization as a potential mediating variable. Model 1 tests the overall effect of the intervention on working alliance at 1 month while controlling for baseline working alliance; the effect was positive and significant. Model 2 introduces a potential mediating effect—outpatient service utilization by 1 month. This variable was shown to have a strong and significant main effect on working alliance and a weak mediating effect on the relationship between the intervention and working alliance.
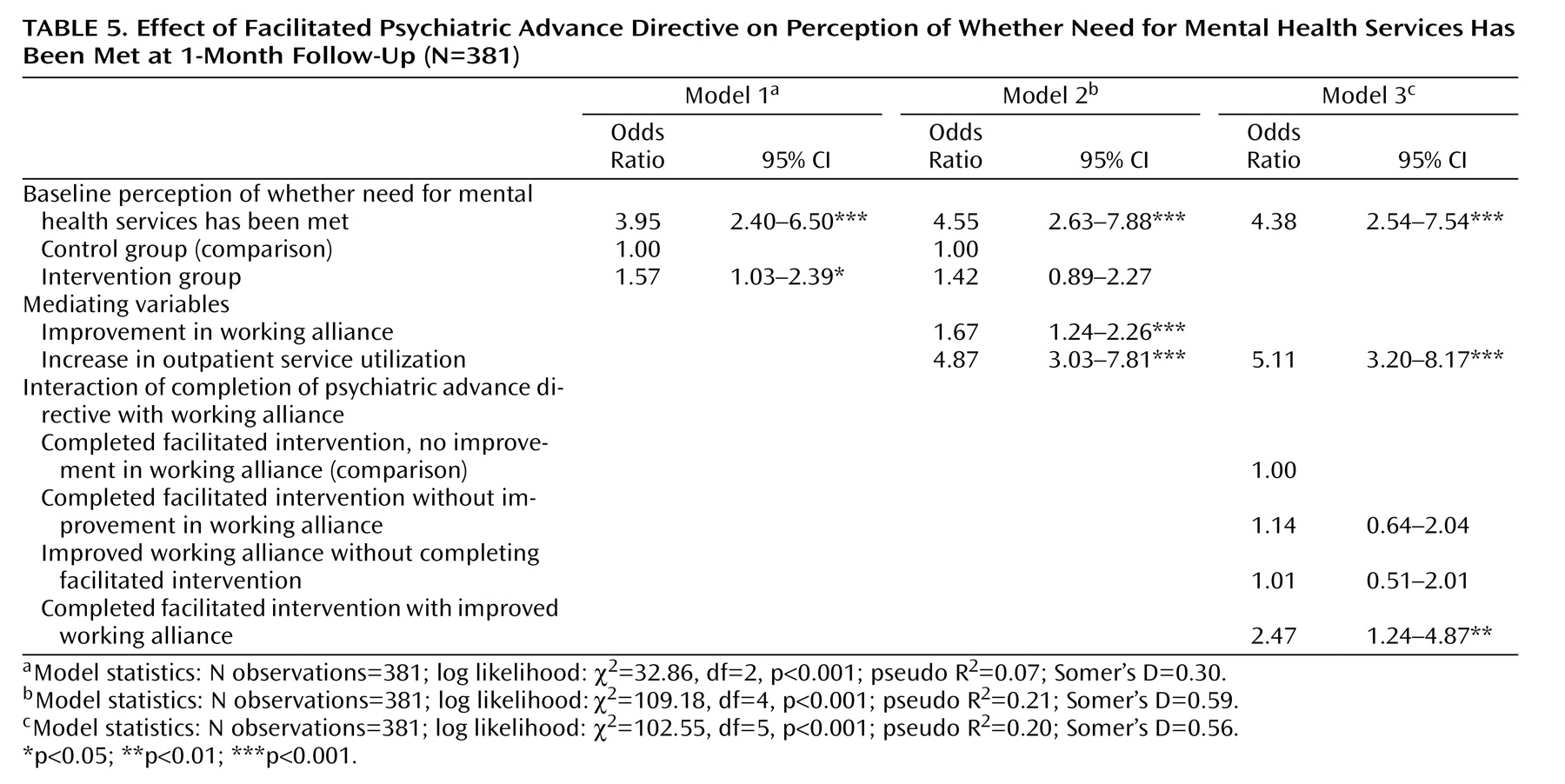
Table 5 presents the results of the analysis of the intervention’s effect on perception of whether need for treatment has been met. In model 1, participants in the intervention were significantly more likely than control subjects to report at 1-month follow-up that their need for treatment was met, controlling for baseline level (odds ratio=1.57, p<0.05). In model 2, this effect was mediated by improvement in working alliance and increase in outpatient services utilization. In model 3, we tested the categorical interaction effect of the intervention with improved working alliance. Participants in the intervention group whose working alliance improved were more than twice as likely as those whose working alliance did not improve to report that their need for treatment had been met (odds ratio=2.45, p<0.05).
Discussion
In this study we examined the effectiveness of using a manualized intervention that provided structured facilitation for persons with severe mental illness to complete psychiatric advance directives. Outcomes for the intervention group were compared with those in a control group who received information about psychiatric advance directives and referral for assistance from existing resources in the public mental health system.
We found that whereas only 3% of patients in the control group completed some type of psychiatric advance directive, 61% of patients in the intervention group did—comparable to the 66%–77% of respondents in a five-city study
(10) who reported a desire to complete a psychiatric advance directive if assisted. Patients in our intervention group were also far more likely to complete both legal components of a psychiatric advance directive—the advance instructional directive (56.5% versus 2.6%) and health care power of attorney (47.7% versus 1.7%).
Among participants in the intervention group, psychiatric advance directives were more likely to be completed by those who were older, those with higher scores on the reasoning subscale of the Decisional Competence Assessment Tool for Psychiatric Advance Directives, more adverse medication experiences according to the Drug Attitude Inventory, and higher scores on the independent help seeking subscale of the Treatment Motivation Questionnaire. These findings are generally consistent with earlier work by Srebnik and colleagues
(8) . Psychiatric advance directives were less likely to be completed by participants with a recent history of violent victimization. This model suggests that completion of psychiatric advance directives is determined by several variables operating jointly, including duration of illness and receipt of treatment, motivation from past adverse experiences with treatment, cognitive ability to understand and manipulate concepts related to advance directives, and independent help-seeking motivation. It is likely that violent victimization—the sole negative predictor of completion in the final model—functions as a proxy variable for adverse social environments that impede participation in treatment.
Virtually all of the psychiatric advance directives completed by participants in the intervention group were consistent with community practice standards for prescription of psychotropic medication and included feasible plans for hospitalization during a crisis. Again, these findings support the results of earlier work by Srebnik and colleagues
(5) .
Compared with the control group, participants in the intervention group showed significantly greater improvement in their working alliance with clinicians and were more likely to report that their need for mental health treatment had been met.
Overall, these results provide strong evidence that a structured 120-minute facilitation session can be effective in helping patients overcome barriers to completing legal documents for psychiatric advance directives. We also found that these facilitated sessions were useful in helping patients express their treatment preferences in ways likely to be useful to treating clinicians. On the whole, when given the opportunity, patients make reasonable treatment requests, directing their treatment team to current and appropriate treatment regimens. Their advance directives were feasible and congruent with good clinical care. Moreover, completing a psychiatric advance directive was associated, at least in the short term, with a significant improvement in patients’ working alliance with their clinicians and in their perception of whether their need for treatment had been met.
The principal limitation of this study is that the benefits of facilitation sessions for completing psychiatric advance directives observed in this study may not generalize to all patients with severe mental illness. Patients who were not engaged in treatment or who refused to participate may have had different responses to facilitation or may have articulated different wishes about future treatment. However, such patients may not have wished to complete psychiatric advance directives, and patients who are in treatment arguably constitute the most relevant target population for advance directives. In addition, the short-term improvements in working alliance and in perception that need for treatment has been met may not be sustained over time. Subsequent analysis will focus on these issues as well as the effects of psychiatric advance directives on crisis treatment and outcomes in periods of decisional incapacity.
In sum, it appears that the structured, manualized facilitation session is an effective method of helping patients complete psychiatric advance directives and ensuring that the documents contain useful information about patients’ preferences for treatment. However, for advance directives to achieve their promised benefit, system-level policies and interventions may be needed in order to embed facilitation of psychiatric advance directives in usual-care settings and institute ways to identify patients in crisis who have advance directives, retrieve the relevant documents, and respond appropriately.