Only minimal modifications in the DSM-IV criteria are recommended for diagnosing posttraumatic stress disorder (PTSD) in children and adolescents, although no children under 15 years were included in the DSM-IV field trial for PTSD
(1) . This raises questions about how suitable the criteria are for children. It also raises questions about which risk factors may increase vulnerability to PTSD at different ages and from whom diagnostic information should be obtained. The purpose of this investigation was to explore three developmental issues of PTSD expression and detection in children from the first few years of life through adolescence.
The first issue is the question of specifying risk factors for the development of PTSD symptoms in children of different ages. The majority of prior risk factor studies have sampled 7–18-year-old children, and none of those used developmentally modified criteria. It remains unclear how those findings correspond to younger children. In this study, we chose to examine risk factors drawn from meta-analytic reviews of studies of adults
(2,
3) . We measured five of these empirically supported risk factors: younger age, female gender, minority ethnic group, prior traumatization, and pretrauma psychiatric problems. Of these, pretrauma psychopathology has shown more uniform effect sizes across studies in adults
(3) . Meta-analytic reviews of child studies have been restricted to victims of sexual abuse
(4) or domestic violence
(5) and either did not support these risk factors (age and gender) or neglected to analyze them (ethnicity, prior trauma, and pretrauma psychopathology), but there have been multiple individual studies of children that support each of these risk factors
(6) . The only risk factor that has been shown to predict PTSD symptoms in preschool children from the limited literature is witnessing a threat to a caregiver
(7) . We believe that our study is the first exploration of these risk factors in a group of 0–18-year-old children.
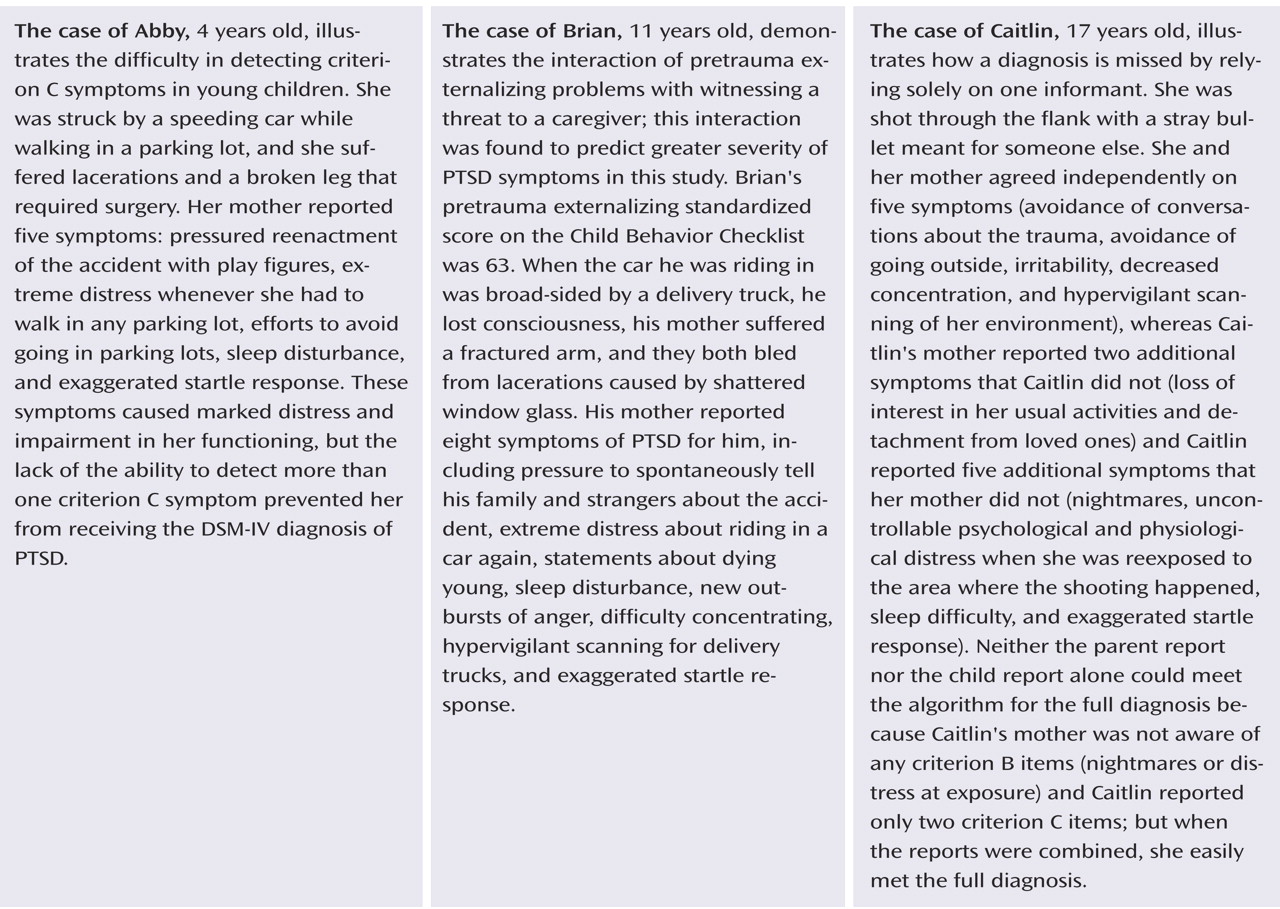
The second issue is the developmental appropriateness of the symptoms and algorithm thresholds for younger children. Modifications that have been proposed to make the DSM-IV criteria more sensitive for young children are to reduce the required number of items in the numbing/avoidance criterion (criterion C) from three to one and to reduce the number of items in the hyperarousal criterion (criterion D) from two to one
(8,
9) . To our knowledge, the appropriateness of the number of items per criterion has not been examined previously in school-age children and adolescents. This would be important to know because it has been documented that the threshold for criterion C may be too high even for adults
(10) . We believe that ours is the first exploration of this issue with developmentally modified probes in a group of 0–18-year-old children.
The third developmental issue is the absence of self-reports from young children, which may lead to underestimates of the level of symptomatology of internalizing disorders
(11) . In the three known studies that examined the relative value of parent versus child reports for PTSD symptoms
(12 –
14), the parent and child reports were significantly positively correlated, but in two of the studies children reported significantly more symptoms than parents. The consensus is that using a combination of parent and child reports, known as the “or rule,” is most likely to yield the most accurate assessment of internalizing symptomatology
(11) . Obviously, however, young children cannot report on their symptoms validly. Therefore, a third purpose of this study was to compare child and parent reports on children ages 11–18 years and then to consider within this homogeneous trauma cohort to what degree parent report alone may underestimate symptoms in the younger children.
We predicted that 1) younger age, female gender, minority race, prior traumatization, pretrauma psychiatric problems, and threat to caregiver would be predictive of trauma symptomatology, 2) the required number of PTSD criterion B symptoms (one) and D symptoms (two) would be evident across the ages of children studied but that children in the youngest group would be significantly less likely to manifest the required number of criterion C symptoms (three), and 3) the older children (ages 11–18 years) who were asked for self-reports would report significantly more signs and symptoms of PTSD following trauma than would their parents.
Method
Participants
Over 20 months (July 1999 through February 2001), there were 204 inpatient admissions of 0–18-year-old children from English-speaking families to a level I trauma center. Parents were approached personally in the hospital. One-half of them could not be approached in the hospital because their stay was less than 24 hours or because the recruiter was not available. Among the 102 families who were approached, only eight caregivers refused, and 94 consented to participation. The age of the children (mean=10.4 years, SD=4.9) in the 110 nonconsenting families (102 never approached, eight refused) did not differ significantly from that among the 94 families that gave consent (mean=10.3 years, SD=5.0) (t=0.10, df=202, p=0.92). However, the consenting families had a significantly higher percentage of female children (36.2%) than did the nonconsenting families (19.1%) (χ 2 =6.98, df=1, p=0.008).
Sixty-two of the 94 consenting families (30.4% of the 204 families of all hospitalized patients) could be reached by telephone for the follow-up interview 2 months later. The 30.4% participation rate is similar to or better than the rates in similarly designed studies in urban American settings (25% in reference 15 and 36% in reference 16). The children in the 32 consenting families without follow-up data were compared to the 62 participants. They did not differ on age, race, mother’s education, mother’s employment status, father’s education, father’s employment status, number of parents in the home, injury severity score, or pretrauma Child Behavior Checklist
(17) total, internalizing, or externalizing score. The groups differed significantly only on gender. The children in consenting families that did not participate by telephone were more often female (50.0%) than children in families that did participate (29.0%) (χ
2 =4.02, df=1, p=0.05).
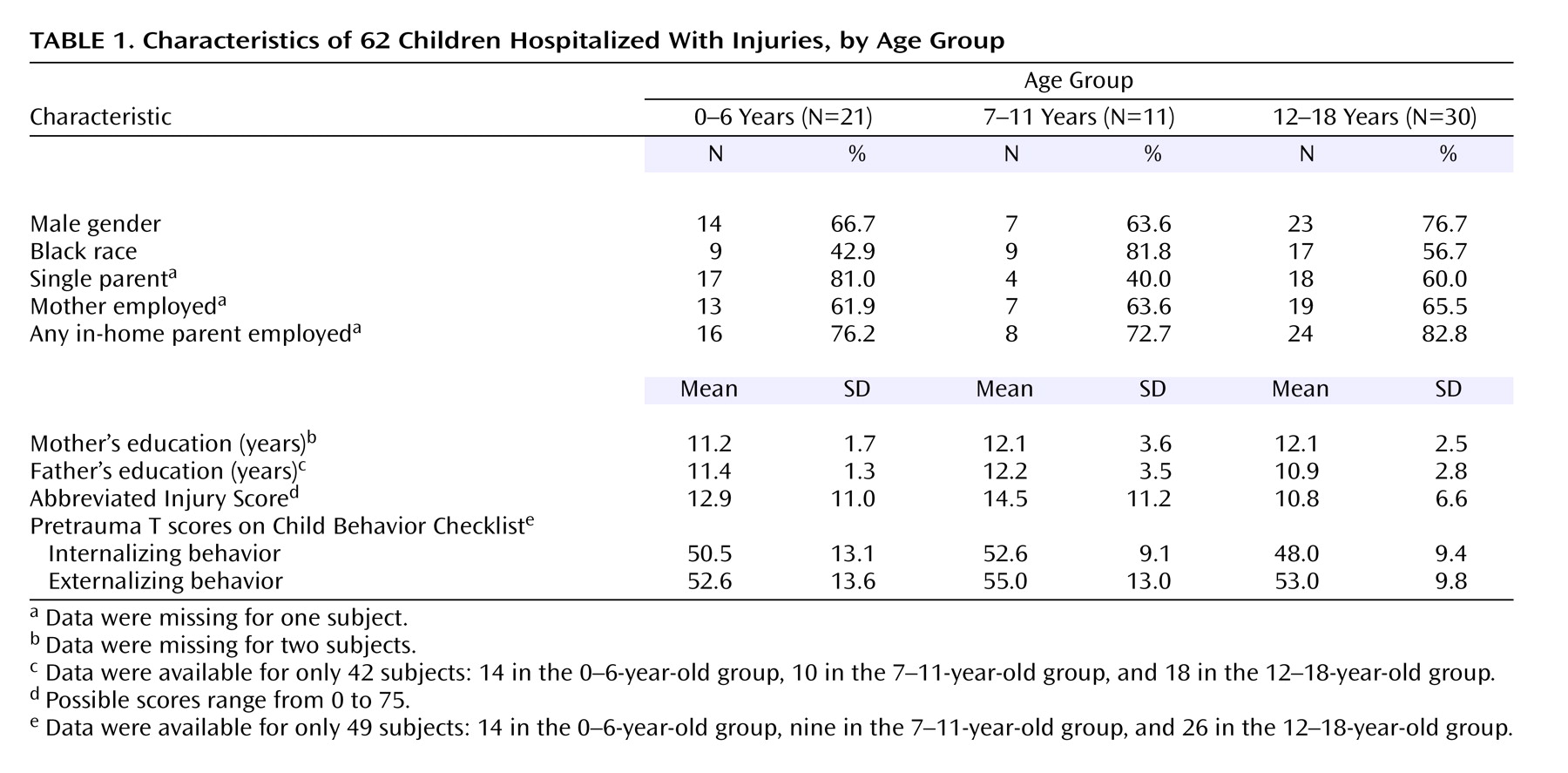
Demographic characteristics are presented in
Table 1 for the participants divided into three age groups, and these age groups did not differ significantly from each other on any of the demographic variables. The injuries were sustained from 44 incidents involving motor vehicles (while the children were passengers, pedestrians, or on bicycles), eight gunshot wounds, four falls, two burns, one assault, one kick by a horse, one football injury, and one dog bite. The injuries included 40 bone fractures, 16 internal organ injuries (gunshot wounds, splenic lacerations, and pulmonary contusions), and two burns; 10 patients had lacerations only. Three patients received craniotomies for brain swelling, and 13 had Glasgow Coma Scale scores below the normal of 15 in the emergency room. Some participants had multiple injuries.
For one adolescent, we were able to obtain information on PTSD from only the adolescent and not from the caregiver. Thus, data on PTSD from caregivers are available for 61 subjects.
Measures
Prior trauma was recorded as yes/no responses to questions about previous life-threatening traumatic events. Caregivers were asked systematically about sexual and physical abuse, car or airplane collisions, dog bites, house fires, and witnessing of domestic violence, and they were given an open-ended question about other possible events. Nineteen participants had prior events.
The Child Behavior Checklist
(17) was completed by the mothers to determine pretrauma emotional and behavioral problems in their children. The version for ages 2–3 or ages 4–18 was used depending on the child’s age. The broad scores for internalizing and externalizing behaviors were used in analyses.
One item was designed to determine whether the child had witnessed a threat to a caregiver. The item was scored yes if the parent was involved in the same accident as the child.
The Abbreviated Injury Score is the standard severity scale for physical injuries. Five regions of the body (general, head and neck, chest, abdomen, and extremities) are rated from the medical chart. Possible scores are 0 to 5. The three highest scores are squared and then summed. Total scores range from 0 to 75. The validity for the Abbreviated Injury Score in predicting mortality is well established
(18) .
A standardized, semistructured interview assessing PTSD criteria was administered by trained research assistants to caregivers and to adolescents 11 years old and older. This measure was created because we could find no validated developmentally sensitive instrument that covers the age range 0 to 18 years. This measure contained all of the DSM-IV items plus five items with wording modified according to previous empirical studies
(8,
19) . The criterion B score is the number of intrusion symptoms (maximum=5). The criterion C score is the number of avoidance and numbing symptoms (maximum=7). The criterion D score is the number of arousal symptoms (maximum=5). The kappa representing interrater reliability for making the diagnosis was 0.79, and the median kappa for all of the items was 0.75
(8) .
Procedure
The Tulane institutional review board approved this protocol. Potential subjects were approached in person during their inpatient stay to request their participation in this study. After the study was explained to a legal guardian, written informed consent was obtained. Written informed consent was also obtained from children who were 11 years and older. The study was explained to children who were between 6 and 10 years old, who then gave their verbal assent. Children younger than 6 years were not asked for assent. The exclusion criteria included mental retardation and pervasive developmental disorders, and no subjects met these criteria according to maternal reports.
Parents completed the Child Behavior Checklist in the hospital to provide information on the children’s pretrauma behavior. Two months later, we called the parents at home and interviewed them about their children’s PTSD symptoms. If the children were at least 11 years old, we also interviewed them by telephone for follow-up.
Data Analysis
Bivariate relationships were examined with Spearman rank correlations for nonnormally distributed continuous data, and a point-biserial correlation was used if one variable was dichotomous. Differences in the mean number of symptoms between age groups were tested with Kruskal-Wallis tests, and pairwise comparisons following significant results were conducted with Wilcoxon rank-sum tests. Differences between age groups in rates of the presence of criteria B, C, and D were tested with Fisher exact tests. Differences in the mean numbers of symptoms according to parent report alone, child report alone, and combined parent and child reports were examined with Wilcoxon signed-rank tests for nonparametric one-sample comparisons. Tests of the ability of risk factors to predict PTSD symptoms were conducted with simple and multiple linear regressions, plus appropriate interaction terms.
Results
Risk Factors and PTSD Symptoms
Each of the seven risk factors was examined for a significant bivariate relationship with the outcome variable by means of simple linear regressions. Witnessing a threat to a caregiver predicted the total number of PTSD symptoms (beta weight=0.34, F=7.61, df=1, 59, p<0.05). Pretrauma externalizing score was a nearly significant predictor (beta weight=0.27, F=3.52, df=1, 46, p=0.07). Child Behavior Checklist scores were missing for 13 of the 62 subjects, but these were fairly evenly distributed between the highly symptomatic (53.8%, or seven of 13, were in the more symptomatic half of the group) and less symptomatic (46.2%, or six of 13, were in the less symptomatic half of the group). The other five predictors were not significant: the beta weights were 0.11 (p=0.39) for younger age, 0.20 (p=0.12) for female gender, –0.10 (p=0.44) for minority race, –0.14 (p=0.28) for prior traumatization, and 0.14 (p=0.33) for pretrauma internalizing score.
Next, we tested a multiple regression model with the predictors that had significant bivariate relationships. The full model included witnessing a threat to a caregiver, pretrauma externalizing score, and an interaction term including these two variables. We opted to use a liberal criterion for entry of predictors into a multiple regression since this was an exploratory study, and we allowed the externalizing variable, which fell just short of significance. The interaction term reflects the documented impact of the parent-child relationship (witnessing a threat to a caregiver) as a mediator of the child’s adaptation following trauma
(20) . The full model regression was significant (F=6.93, df=3, 44, p<0.001) and accounted for 32% of the variance. The interaction of pretrauma externalizing score and witnessing a threat to a caregiver was significant (beta weight=1.91, F=9.68, df=1, 44, p<0.01). The directionality of this interaction indicated that children who witnessed a threat to their caregiver and had elevated pretrauma externalizing scores developed more PTSD symptoms.
Number of Criteria B, C, and D Symptoms by Age
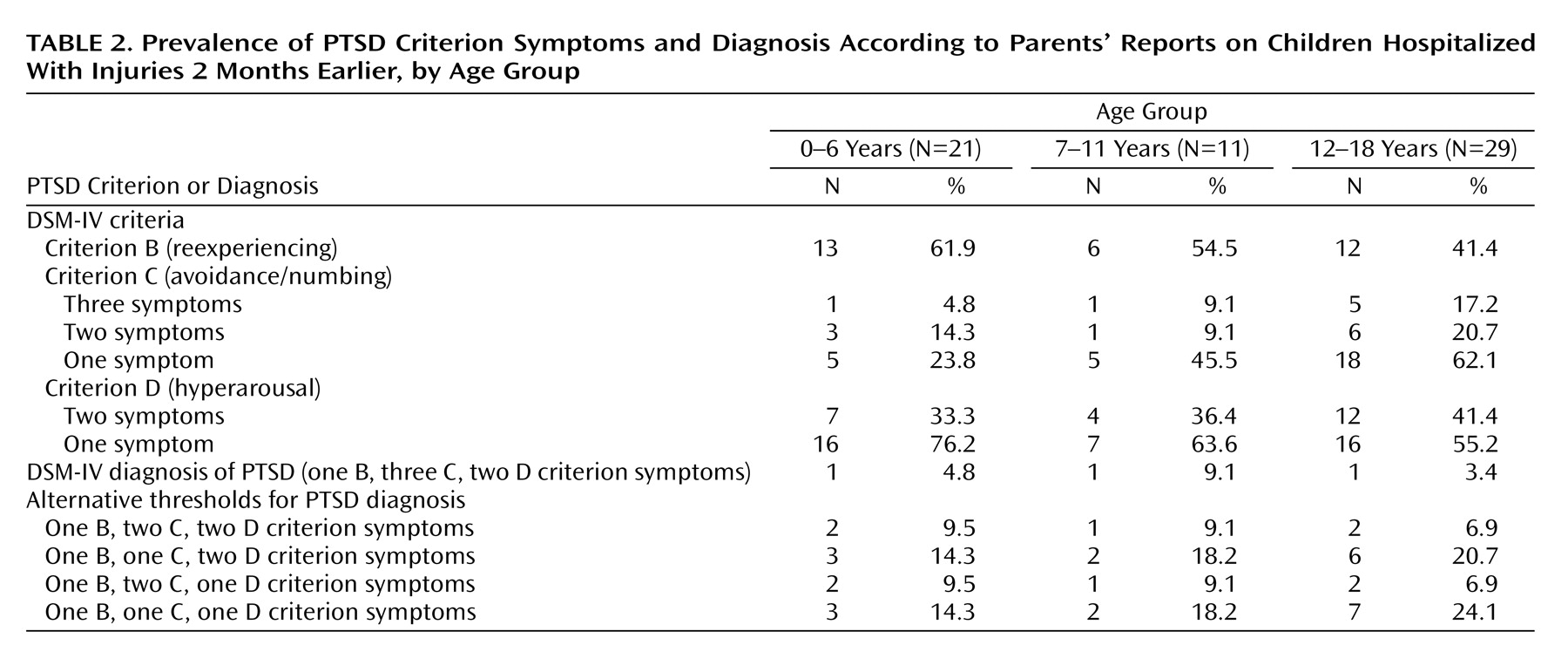
The distribution of symptoms by age showed that children of all ages often met the DSM-IV thresholds of one symptom for criterion B and two symptoms for criterion D (
Table 2 ). However, for criterion C, only one child under 7 years of age met the DSM-IV threshold of three symptoms. This was confirmed statistically with a correlation that showed that criterion C symptoms increased significantly with age (r
s =0.33, N=61, p<0.05). The numbers of symptoms in criteria B and D were not significantly correlated with age, despite a visual trend for children age 12 years and older to show more symptoms of all types. Gender, ethnicity, and Abbreviated Injury Score were ruled out as potential confounders of any age-by-symptom relationships because none of them had a significant bivariate relationship with any of the dependent variables.
Next, the children were divided into three age groups to test whether symptom loads differed by traditionally and empirically defined age groupings. The age groups were 0–6 years (N=21), 7–11 years (N=11), and 12–18 years (N=29). The division between 6 and 7 years was chosen because only one child below age 7 years had three criterion C symptoms. The cutoff point between 11 and 12 years was chosen because this age has traditionally been used to mark the major developmental shift between prepubertal and adolescent children. The distributions of participants within each age group were not skewed toward the younger or older ages—age 0 years, N=2; age 1, N=0; age 2, N=2; age 3, N=3; age 4, N=6; age 5, N=4; age 6, N=4; age 7, N=2; age 8, N=3; age 9, N=1; age 10, N=1; age 11, N=4; age 12, N=5; age 13, N=5; age 14, N=4; age 15, N=6; age 16, N=5; age 17, N=3; and age 18, N=2.
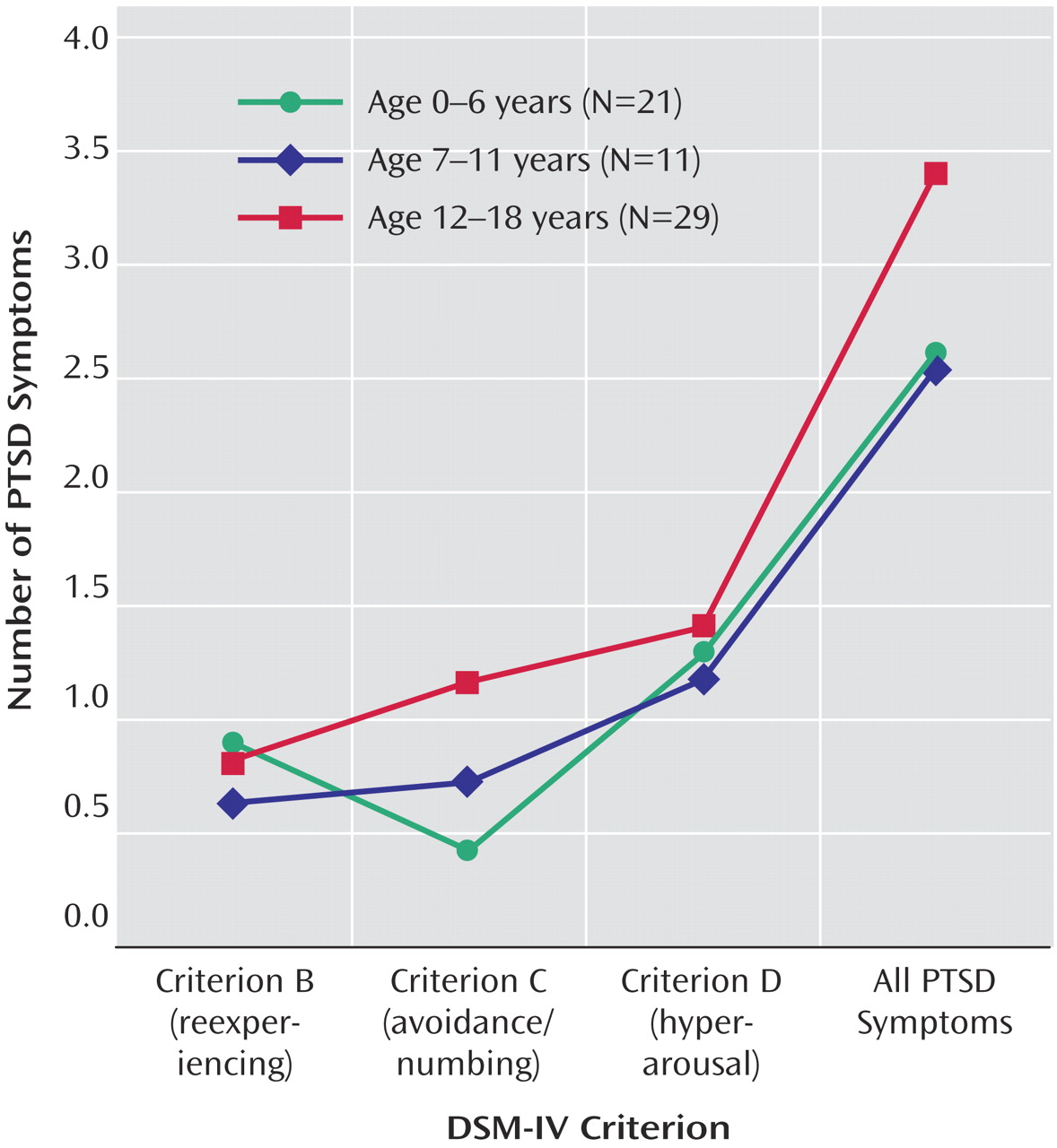
The number of PTSD symptoms by parent report in each of the three criteria (B, C, and D) and the total number of PTSD symptoms are plotted for each age group in
Figure 1 . This figure makes evident visually the discrepancy among age groups for criterion C. Kruskal-Wallis tests were conducted to test whether the number of symptoms endorsed for each criterion and the total number of symptoms differed by age group. The tests for criterion B, criterion D, and total PTSD symptoms were not significant. The test for criterion C symptoms was significant (χ
2 =6.03, df=2, p<0.05). Pairwise comparisons showed that the 0–6-year-old group had significantly fewer criterion C symptoms (mean=0.43, SD=0.87) than did the 12–18-year-old group (mean=1.17, SD=1.44) (z=–2.4, p<0.01 one-sided). The number of criterion C symptoms for the 7–11-year-old group (mean=0.73, SD=1.19) was in between the numbers for the youngest and oldest groups.
Presence of Algorithm-Driven Criteria and Diagnosis by Age
Because the “presence” of criteria C and D and the diagnosis of PTSD are derived from algorithms, we further examined the prevalence of these categorical entities from parental reports by age (
Table 2 ). The disparity in criterion C by age is apparent, as only 4.8% of the 0–6-year-olds (N=1) had three symptoms, thereby meeting the criterion C threshold, compared to 9.1% for the 7–11-year-old group and 17.2% for the 12–18-year-old group; however, there was insufficient power for these categorical differences to reach conventional levels of statistical significance (Fisher’s exact test, p=0.07). For the 0–6-year-old group, the prevalence of criterion C increased to 14.3% when only two symptoms were required and increased to 23.8% when only one symptom was required, making it more comparable to the rate for 12–18-year-olds based on three criterion C symptoms (17.2%). The pattern of changes in the 7–11-year-old group is more difficult to interpret; the prevalence of criterion C did not increase when the threshold was lowered from three to two symptoms (9.1%) but increased substantially when only one symptom was required (45.5%). For the 12–18-year-olds, there was not a substantial difference in the prevalence of criterion C whether three (17.2%) or two (20.7%) symptoms were required, but a one-symptom threshold appeared too liberal (62.1%).
The rates of criterion D were similar across age groups regardless of whether one or two symptoms were required (
Table 2 ). It is interesting that despite the higher rate of criterion C in the 12–18-year-old group, their rate of PTSD diagnosis was not higher than the rates for the younger groups. This “low” rate of diagnosis in the older group was explained by three teens who met the thresholds for criteria C and D but whose parents were not aware of their criterion B symptoms, an important issue addressed in the next section.
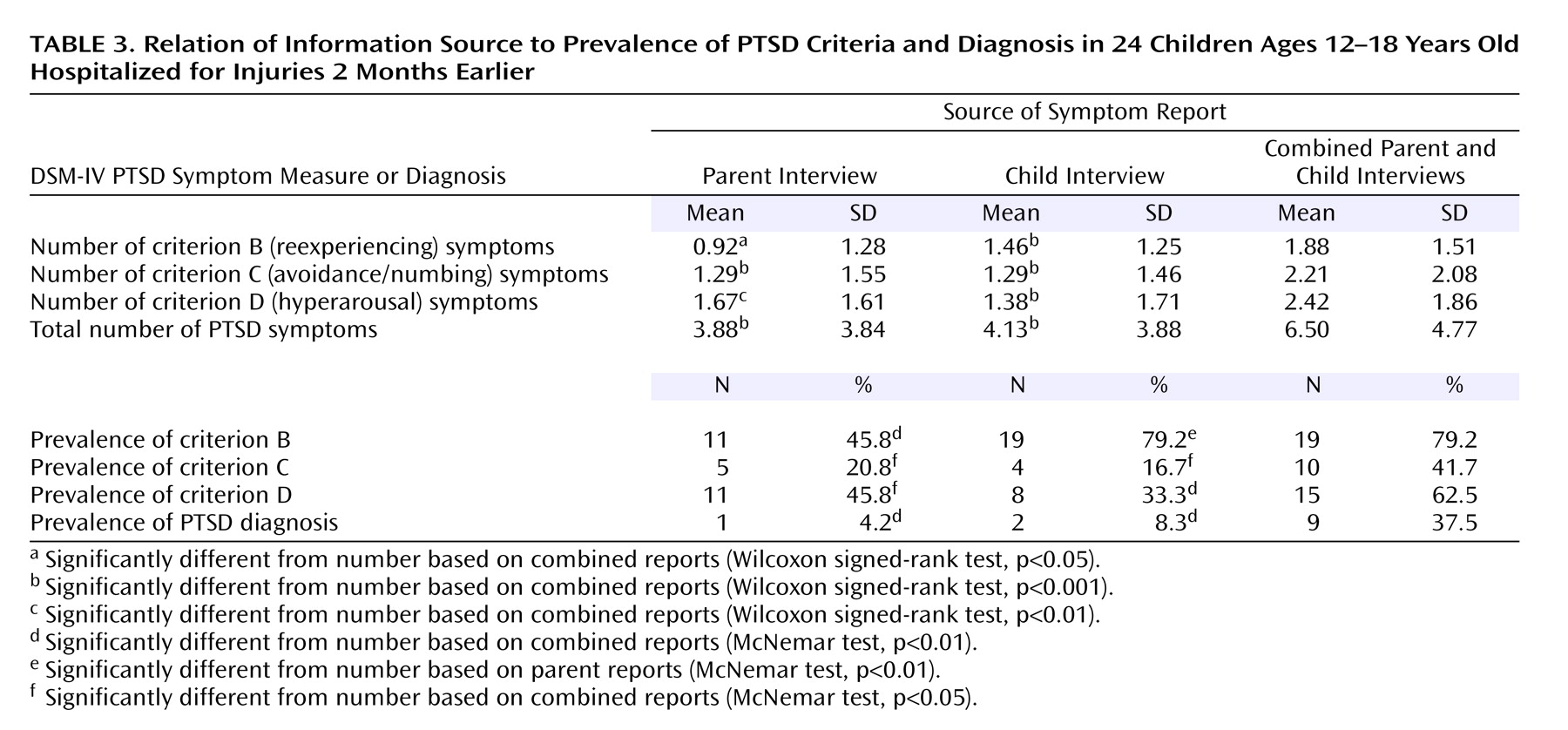
Parent Report Versus Combined Parent-Child Report
Both parent and child interview data were collected for 24 subjects who were ages 11 through 18. The parents’ and children’s reports significantly positively correlated with each other on criterion B (r s =0.48, p<0.05), criterion C (r s =0.42, p<0.05), and total symptoms (r s =0.56, p<0.01) but not on criterion D (r s =0.23). This indicated that for all but criterion D the parents and children generally agreed about who was the most and the least symptomatic.
Children reported more symptoms than parents only for criterion B, and contrary to expectations, parents reported more criterion D symptoms than their children, but both of these differences were nonsignificant. Children and parents reported similar numbers of criterion C symptoms (
Table 3 ). If the parents had been aware of all their children’s criterion B symptoms, then the rate of diagnosis in the 12–18-year-old group by parent report would have been higher (16.7%), as noted in the previous section.
Scores based on only the parents’ reports were compared to those based on just the child reports in terms of their effects on the algorithms for each criterion. Criterion B was present more often by child report (79.2%) than by parent report (45.8%) (McNemar test: χ 2 =8.00, df=1, p<0.01), supporting the hypothesis. For criteria C and D, the parents’ reports reached the thresholds more often than those of the children, contrary to the hypothesis, but these differences were nonsignificant.
Last, the combination of the parent and child scores (the “or rule”) was compared to scores based on the parents alone. Combined scores yielded significantly higher rates of symptoms and of categorical endorsements than parent-alone data for all criteria and the overall diagnosis (
Table 3 ). The magnitude of the differences in numbers of symptoms between combined reports and parent reports was 2.0-fold for criterion B symptoms, 1.7-fold for criterion C symptoms, 1.4-fold for criterion D symptoms, and 1.7-fold for total symptoms. Thus, combined parent-child reports captured almost twice as many symptoms as the parents’ reports alone.
When the combined scores were applied to the DSM-IV algorithm to arrive at diagnoses for the study group, the prevalence of PTSD was 37.5%. Compared to the diagnosis rate of 4.2% based on parents only, this is an 8.9-fold increase. If this rate of increase were applied to the 0–6-year-old group to find a “truer” diagnostic rate, the prevalence would be closer to 43%, as opposed to the 4.8% found with the current DSM-IV criteria.
Discussion
This study makes three contributions to the understanding of PTSD symptomatology in children and adolescents. First, the risk factor analysis across the span of childhood indicated that the risk from witnessing a threat to a caregiver, which had previously been emphasized more for younger children
(7), carries salience for all ages. Specifically, the interaction between witnessing a threat to the caregiver and pretrauma externalizing behavior had an effect on the total number of PTSD symptoms. This adds support to empirically supported models that have demonstrated the importance of the caregiving context for the adaptation of children following trauma
(20) . Also, this result draws attention to the importance of including terms for the interactions between child and caregiving variables in the design and analysis stages of studies.
The second contribution is that support was added to the prior research finding that the DSM-IV algorithm threshold of three symptoms for criterion C is inappropriate for diagnosing preschool children
(8,
9,
19) . This was demonstrated in a cohort that spanned the entire age range of childhood and adolescence; to our knowledge, no previous study has examined this question across such a broad range of ages. The study design eliminated the possibility that young children did not manifest three criterion C symptoms because they had suffered less severe traumas or because they were assessed with different methods. The findings were mixed as to whether the three-symptom threshold is appropriate for 7–11-year-old children. The rate of the presence of criterion C for this group (9.1%) was in between the rates of the younger and older groups and was not statistically significantly different from either. We are not aware of any prior studies that examined the effect of lowering the criterion C threshold in school-age children. However, the studies of school-age children that have produced separate rates of each criterion have shown that criterion C is endorsed less often than criteria B and D
(15) . This suggests that future studies should examine the impact of lowering the criterion C threshold for all prepubertal children (i.e., under 12 years), as has been suggested previously even for adults
(10) .
How can we begin to make sense of developmental shifts in the presence and/or manifestation of criterion C PTSD symptoms around age 7 and/or 12 years? Substantial data already support a stage model of normal development in which cognitive shifts occur around 7 years with the emergence of concrete operations
(21) and advanced executive functions
(22) . EEG studies have demonstrated shifts in normal development of hemispheric coherence between 5 and 8 years and again between 10 and 14 years
(23), and they have demonstrated a progression from undifferentiated to differentiated brain processing from 6 to 12 years, possibly due to the selective atrophy of unused neural circuits
(24) . This convergence of evidence for biobehavioral shifts has not yet been integrated into a mechanism-driven theory of how neural network changes translate into criterion C symptom manifestations.
The third contribution is that when both parents and children were interviewed about the children’s symptoms, the scores produced by combining responses (the “or rule”) were significantly higher than the scores of either informant alone, regardless of criterion, by a magnitude of almost twofold. The implication for young children, for whom only a parent report is available, is that the assessed number of PTSD symptoms will always be an underestimate of the true symptom load
(11) . Furthermore, this finding raises questions about possible underreporting of symptoms in studies of older children that used only parent or child informants, but not both.
Some limitations of this study are important to highlight. The 7–11-year-old group was small, and the findings for this age group ought to be viewed with caution. Child Behavior Checklist data were missing for 13 participants, but they were evenly distributed among participants with low and high levels of PTSD symptomatology. This study group had disproportionate numbers of black participants, unemployed parents, and single-parent families compared to the population of the United States and compared to subjects in European studies. These findings may not be generalizable to those populations. The findings on risk factors may be unique to individuals who suffer bodily injuries and may not be generalizable to other types of traumas. The amount of variance accounted for by this set of predictors was only 32%. Risk factors that have shown better promise in adult studies include aspects of the person’s psychological reaction at the time of the trauma, such as perception of threat and peritraumatic dissociation
(2) . Unfortunately, these highly internalized constructs are far more challenging to assess in young children than in adults, and this difference serves as another reminder of the difficulty inherent in the developmentally sensitive assessment of young children.