Recent studies suggest that a developmental subtype of bipolar disorder can be identified by age at onset of bipolar disorder
(1,
2) . Adults with juvenile-onset bipolar disorder report chronic and unremitting illness, predominance of irritability as compared to euphoria, and mixed mania. These features are similar to illness characteristics described in prospective evaluations of children with bipolar disorder. Furthermore, oppositional defiant disorder/conduct disorder is one of the most common comorbid conditions of childhood bipolar disorder
(3,
4), and there is some evidence that antisocial personality disorder is more common among adults with bipolar disorder than comparison subjects
(5) . Finally, juvenile bipolar disorder is a known risk factor for substance use disorders
(6) . We hypothesized that the following bipolar disorder illness characteristics and comorbid conditions typical of childhood bipolar disorder would occur most commonly among adult bipolar disorder subjects who identified childhood onset of bipolar disorder: irritable mood, mixed manic episodes, nonremitting course, prolonged episode duration, substance use disorders, and antisocial personality disorder.
Previous studies have utilized clinical samples. A large-scale population study of this topic is needed to mitigate recruitment bias and to provide a reasonable estimate of the proportion of childhood-onset bipolar disorder among those with lifetime bipolar disorder.
Method
Subjects were 1,411 respondents of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions who met DSM-IV criteria for bipolar disorder. Cases of bipolar disorder were excluded if they were deemed secondary to substance use or a general medical condition. The National Epidemiologic Survey on Alcohol and Related Conditions is a representative sample of the United States conducted by the National Institute on Alcoholism and Alcohol Abuse (NIAAA). A detailed description of the survey has been described in detail elsewhere
(7) . Briefly, 43,093 noninstitutionalized civilian respondents, 18 years and older, completed face-to-face computer-assisted personal interviews. The overall survey response rate was 81%.
Approximately 1,800 lay interviewers with an average of 5 years of related experience administered the National Epidemiologic Survey on Alcohol and Related Conditions using laptop computer-assisted software. Interviewers completed 10 days of centralized, standardized training sessions.
The NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version was used to generate the diagnoses presented in this report. This interview has demonstrated reliability and validity for the diagnoses of personality disorders, substance use disorders
(7), and mood and anxiety disorders
(8) .
The Alcohol Use Disorder and Associated Disabilities Interview Schedule explicitly addresses the temporal contiguity of manic episodes with substance use when present. Only cases in which bipolar disorder occurred independently of substance use were included in the analyses.
Nonremitting bipolar disorder status was determined by self-reported absence of a symptom-free interval of 2 months or more. Prolonged manic episodes were defined as exceeding 6 months, by which time the large majority of manic episodes can be expected to remit
(9) . Age at onset of bipolar disorder was determined by self-report data from the Alcohol Use Disorder and Associated Disabilities Interview Schedule. Subjects who did not identify an age at onset (4.6%, N=65) were included in the adult-onset group.
One-way analysis of variance (ANOVA) was used to compare differences between groups on dimensional measures, while chi-square analyses were used to detect differences on categorical measures.
Results
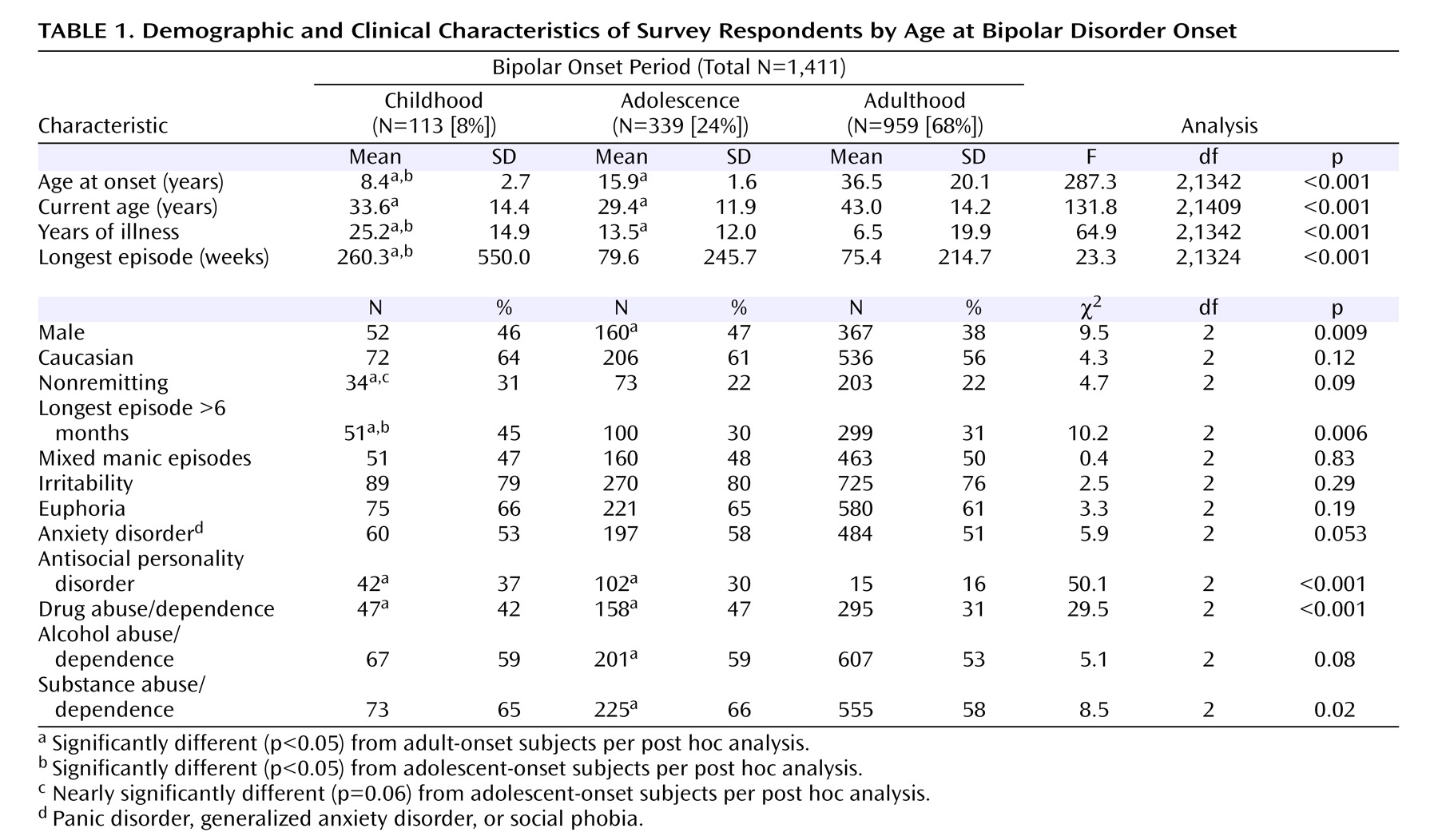
Of the 1,411 subjects with lifetime bipolar disorder, 8% (N=113; 95% CI=6.6%–9.4%) had childhood age at onset, 24% (N=339; 95% CI=21.8%–26.2%) had adolescent age at onset, and 68% (N=959; 95% CI=65.6%–70.4%) had adult age at onset. These groups were significantly different from one another in a number of domains (
Table 1 ). The adolescent-onset group included a significantly greater proportion of males (47%, N=160) than the adult-onset group (38%, N=367). Childhood-onset bipolar disorder was associated with more prolonged longest episode duration (F=23.3, df=2, p<0.0001). However, the childhood-onset group had significantly more mean years of illness. Due to the possibility that this between-group difference confounded the relationship between group and duration of longest episode, number of years of illness was added as a covariate to the ANOVA. Nonetheless, the results regarding longest episode duration remained significant (F=9.1, df=3,1285, p<0.001). An exploratory post hoc analysis of difference in proportion of nonremitting status was conducted on the basis of the tendency toward statistical significance across the three groups. The childhood-onset group had a significantly higher proportion of nonremitting illness than either the adolescent- or adult-onset groups. Both the childhood- and adolescent-onset groups had a significantly higher proportion of drug abuse or dependence as compared with the adult-onset group. The proportion of comorbid antisocial personality disorder was highest in childhood-onset group, and was significantly greater than the proportion in the adult-onset group. There were no between-group differences in proportions of respondents who had attended emergency departments (χ
2 =4.4, df=2, p=0.11) or had been hospitalized (χ
2 =2.4, df=2, p=0.30) as a result of mania. An exploratory cross-tabulation showed the greatest prevalence of lifetime anxiety disorders (
Table 1 ) among adolescent-onset subjects.
Discussion
These data corroborate those of previous reports indicating that bipolar disorder illness characteristics among adults with childhood-onset bipolar disorder resemble those observed among children with bipolar disorder. The primary findings of the study were that childhood-onset subjects were more likely than adult-onset subjects to report prolonged episodes, nonremitting course of illness, comorbid antisocial personality disorder, and comorbid drug use disorders. In addition, approximately one in 10 individuals with bipolar disorder described onset of mania in childhood, and to our knowledge this is the first community-based population study to provide such an estimate. The fact that this estimate is significantly lower than that reported in a recent large-scale clinical sample (27.7%)
(10) could be expected based on the known differences between clinical and community samples.
A limitation of the study was the sole use of retrospective report to determine age at onset, since this may be subject to recall bias. In addition, episode duration, remission, and comorbid substance use disorders were not corroborated by clinical or administrative records. Importantly, the mean number of years of illness in the childhood-onset group was greater than that of the adolescent- and adult-onset groups. However, results remained significant after including years of illness as a variable in the ANOVA.
Longitudinal follow-up data of children with bipolar disorder into adulthood will not be available for several years. In the interim, data such as these lend further support to the assertion that bipolar disorder has its roots in childhood in a significant minority of cases, and that in such cases the nature of bipolar illness is particularly severe. Implications include heightened awareness of the potential prognostic importance of age at onset in the phenomenology, course, and comorbid conditions of bipolar disorder.