Schizophrenia may be associated with hyperthermic syndromes such as febrile catatonia, neuroleptic malignant syndrome, and heatstroke; therefore, schizophrenic patients might exhibit abnormal heat tolerance. Heat tolerance is defined as an individual’s ability to adapt appropriately to heat stress, and it is assessed clinically by an exercise-heat tolerance test. Individuals whose rectal temperature starts rising earlier and at a faster rate than that of normal comparison subjects under similar environmental conditions are categorized as heat intolerant
(1,
2).
Numerous factors have been suggested to compromise an individual’s tolerance to heat, including antipsychotic drugs
(2). However, the data on thermoregulation in schizophrenia and the possible effects of antipsychotic drugs on the regulation of body heat are contradictory and mostly based on studies of animal models
(3,
4). There is no information in the literature on the ability of schizophrenic patients maintained on antipsychotic drugs to regulate body temperature under controlled heat stress conditions.
The aim of the present study was to investigate the tolerance of male schizophrenic patients to moderate heat stress in comparison to healthy matched subjects.
Method
The patient group consisted of eight outpatient men with remitted schizophrenia (Brief Psychiatric Rating Scale [5] score less than 35 on the day of the heat tolerance test) who met the DSM-III-R criteria for chronic schizophrenia. Six of the patients had never smoked, and the other two had ceased smoking at least 2 years before. The patients had been maintained on haloperidol decanoate (N=6) or fluphenazine decanoate (N=2) for at least 12 consecutive months before the study.
The comparison group consisted of eight men without an apparent psychiatric disorder. None of them had smoked for at least 3 years before testing.
All participants were considered physically healthy on the basis of past history, ECG recordings, and physical examinations; none was obese (body mass index less than 29 kg/m2), and the results of routine laboratory tests were within normal ranges in all cases.
All of the participants did not formerly engage in any regular sports activity, and none had a history of febrile catatonia, neuroleptic malignant syndrome, or heatstroke.
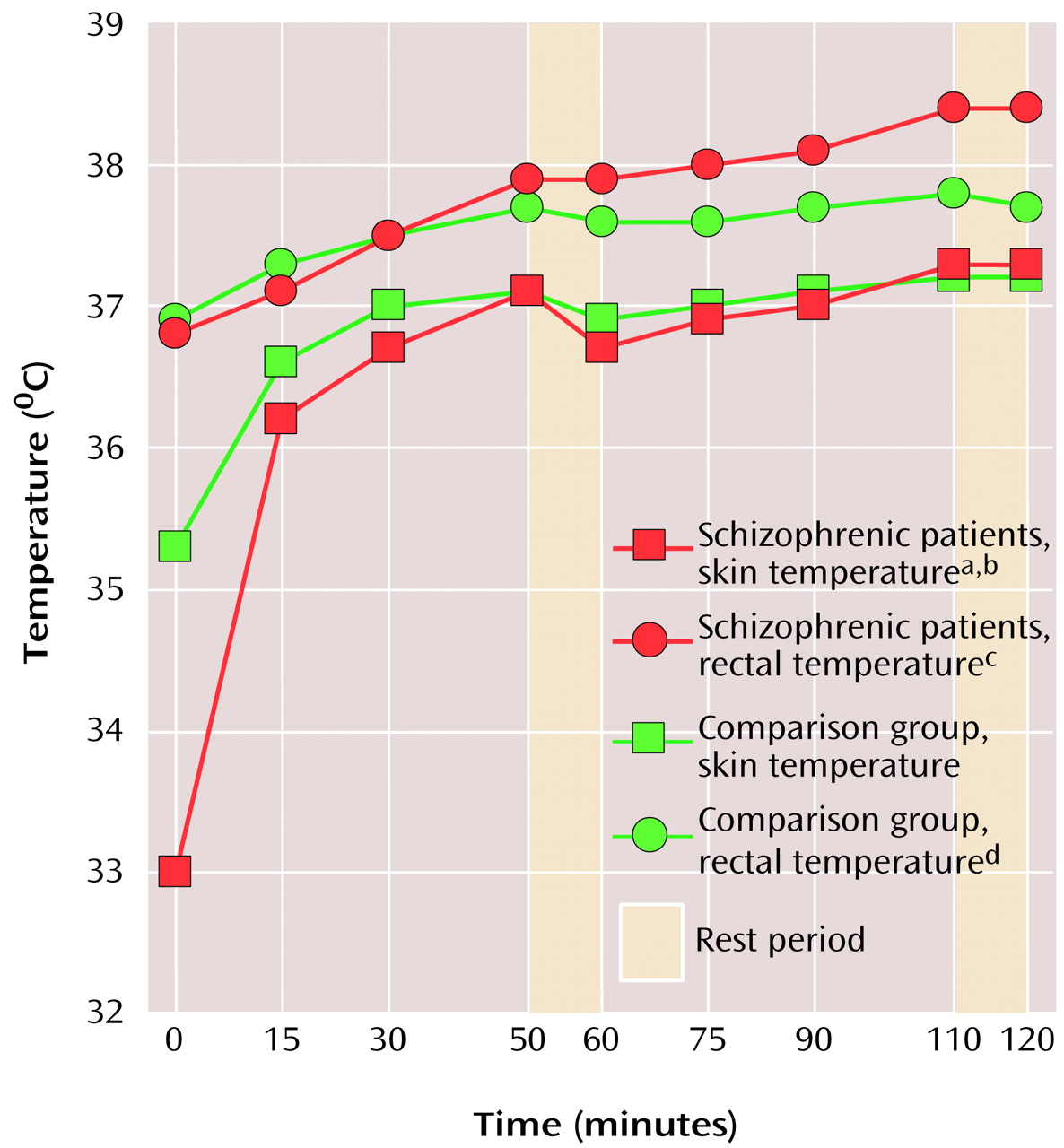
Testing took place in a climate chamber and was performed at an ambient temperature of 40°C and a relative humidity of 40%. The subjects were attired in T-shirts, shorts, and sneakers. The heat tolerance test consisted of two 50-minute bouts of walking on a motor-driven treadmill at a pace of 3.2 miles per hour up an incline of 2%. There was a 10-minute rest period after each exercise phase (
Figure 1). A rectal temperature of 39°C and a pulse rate of 180 bpm were set as the upper safety limits.
The Geha Psychiatric Hospital’s review board approved the study, and written informed consent was obtained from all participants after the procedures had been fully explained.
Rectal temperature and skin temperature (at three locations: chest, arm, and leg) were measured by using suitable thermistors (Yellow Springs Inc., Yellow Springs, Ohio). Weighted skin temperature was calculated according to Burton
(6). Heart rate was monitored continuously with a heart rate monitor (Polar Electro Oy, Kempele, Finland). Blood pressure and body weight were measured before and at the end of the test. Fluid balance was calculated according to weight difference corrected for fluid intake and urine output.
Statistical analysis was carried out by means of univariate analysis of variance (ANOVA), with repeated measures and covariates when needed for the two exertion phases and separately for the two rest intervals. The probability values were adjusted by the Geisser-Greenhouse test. The grouping factors were schizophrenic patients versus comparison group and the two factors of repeated measures: phase (two levels) and time (four levels for exertion and two levels for rest phases). The interaction of the groups with time was considered the main effect of the test. The unpaired, two-tailed Student’s t test was used as appropriate. Data are given as means and standard deviations.
Results
The schizophrenic and comparison groups had similar mean ages (mean=31.5 years, SD=6.5, versus mean=31.6 years, SD=4.9, respectively), body weights (mean=78.7 kg, SD=14.1, versus mean=79.5 kg, SD=10.8), heights (mean=173.6 cm, SD=9.7, versus mean=174.0 cm, SD=4.0), body surface areas (mean=1.92 m2, SD=0.19, versus mean=1.94 m2, SD=0.12), and body mass indexes (mean=26.1 kg/m2, SD=1.4, versus mean=26.3 kg/m2, SD=2.5) (all nonsignificant). All participants completed the heat tolerance test except one patient whose rectal temperature reached the upper safety limit (39°C) after 90 minutes.
Neither the initial heart rate nor the rate of increase in heart rate during the exertion and rest phases of the heat tolerance test differed significantly between the groups; this was also true for blood pressure. All three possible interactions with group (phase and group, time and group, time and phase and group) during exertion and rest were nonsignificant when ANOVAs were performed.
Initial skin temperature was significantly lower in the patient group (mean=33.0°C, SD=1.9) than in the comparison group (mean=35.3°C, SD=1.1) (t=2.85, df=14, p=0.013) (
Figure 1). The rate of increase in skin temperature was significantly higher in the patient group than in the comparison group (time and group interaction: F=7.29, df=3, 39, p=0.0005) (time, group, and phase interaction: F=5.43, df=3, 39, p=0.004). The phase and group interaction was nonsignificant, as was the decrease in skin temperature during the rest periods.
The rise in rectal temperature during exertion was significantly greater in the patient group than in the comparison group. This was demonstrated by the significant phase and group (F=10.61, df=1, 12, p=0.007) and time and group (F=8.20, df=3, 39, p=0.0002) interactions, whereas the interaction of phase, time, and group was nonsignificant. During the rest intervals, there was a significant interaction of phase and group (F=38.97, df=1, 13, p=0.0001), but the interaction of time and group and the interaction of phase, time, and group were nonsignificant (
Figure 1).
Sweat production did not differ between the patients and the comparison subjects (mean=1307 ml, SD=356, versus mean=1387 ml, SD=267, respectively).
Discussion
Our study indicates that male schizophrenic patients in long-term treatment with high-potency neuroleptics are less tolerant to exercise heat stress than are healthy comparison subjects. These results are consistent with those of some previous animal studies indicating thermoregulatory dysfunction in neuroleptic-treated animals
(3,
4).
This finding might be explained by an impaired ability in neuroleptic-treated schizophrenic patients to conduct heat from the body’s core to the periphery. This possibility is supported by the combination of significantly greater increases in rectal temperature and skin temperature during the exertion phases and the greater decrease in rectal temperature during the rest intervals in the comparison group (
Figure 1). The impaired thermoregulation may be related to a failure of the vascular system, the main system that conveys heat to the periphery
(7). Indeed, previous studies have suggested the presence of vascular bed dysfunctioning in treated schizophrenic patients
(8,
9). However, the possibility that schizophrenic patients may also produce excessive heat during physical exertion (because of decreased work efficiency) has not been ruled out.
The putative thermoregulatory dysfunction in schizophrenic patients might be involved in their susceptibility to risky hyperthermic syndromes (e.g., febrile catatonia, neuroleptic malignant syndrome, or heatstroke). It is as yet unclear if the hyperthermic response of schizophrenic patients to the heat tolerance test reflects a specific pathophysiology in schizophrenia, a neuroleptic-induced effect, or both. Further studies with drug-free schizophrenic patients are needed to substantiate our findings.