The risk of depressive disorders occurring during the puerperium is thought to contribute to the higher rate of mood disorders among women than men in the United States
(1–
3). The combined period prevalence of postpartum major and minor depressive disorders is estimated to be between 5% and 25%
(2,
4–
12). Although the prevalence rates for postpartum depression have received substantial attention
(13,
14), little research has evaluated the prevalence and risk in ethnic minority groups or in women of lower socioeconomic status
(1,
4,
7,
15). The only U.S. study of low-income postpartum women found a point prevalence of 23% for postpartum depression, including 7% for major depressive disorder and 16% for minor depressive disorder. These rates are about twice those published for postpartum women from a middle-class sample in the United States (4% and 6% for major depressive disorder and minor depressive disorder, respectively)
(13), suggesting that lower income level or minority status may increase the risk of postpartum depression
(1).
An ongoing problem in depressed populations is the low rate of detection and treatment
(16–
18). Less than half of women suffering major depressive disorder will be identified and treated
(19), which makes detection a major public health problem. Several factors may identify women at greater risk for depression during the postpartum period, including, but not limited to, a history of major depressive disorder, depressive symptoms during pregnancy, obstetrical complications, unstable marital (or other significant) relationships, stressful life events, low income, low educational attainment, and not breast-feeding
(4,
9,
20–
27). Many of these factors also contribute to vulnerability to depression in women at times other than the postpartum period
(28,
29).
It is important to evaluate whether these risk factors for major depressive disorder are salient for ethnic minority women, an inadequately studied group. In a busy, publicly funded inner-city clinic, the amount of information predictive of risk for mood disorders may be limited, but it would be helpful to clinicians if commonly available information could be used to identify postpartum women at particular risk for major depressive disorder.
This study estimates the rate and persistence of depression during the postpartum period in a multiethnic, largely Hispanic population of lower socioeconomic status culled from four publicly funded inner-city maternal health clinics. Given earlier findings, we hypothesized that the rate of depressive symptoms and the rate of major depressive disorder would be higher among Latina and African American women, who are socioeconomically disadvantaged, than the reported rates for non-Hispanic white, middle-class women in the United States. Second, on the basis of commonly available medical and demographic information as well as previous work
(4,
9,
10,
26), we hypothesized that women living with their extended families rather than with a spouse or significant other would be at greater risk for both depressive symptoms and the syndrome of major depressive disorder. Third, we hypothesized that women with more severe depressive symptoms immediately after delivery would be more likely to maintain these symptoms and have a diagnosis of major depressive disorder several weeks later
(10,
14,
30–
33).
Method
Participants
Potential subjects included all women who came for their initial postpartum appointments on selected days at four inner-city maternal health clinics in Dallas. Of 890 women consecutively approached, 802 agreed to participate; 88 (10%) of the patients declined to participate or were unavailable. This constitutes a systematic sample of about 13% of postpartum patients from these four clinical sites. Subjects were eligible for participation if they had completed their pregnancies or miscarried. Participants had a mean age of 24.2 years (SD=5.6, range=14–48); most had some secondary school but had not completed high school; 20 (2%) were white non-Hispanic, 162 (20%) were African American, 604 (75%) were Hispanic, 5 (1%) were immigrants from Asian countries, and 11 (1%) were of other ethnic backgrounds; 489 (61%) of the participants spoke Spanish only. Four of the women had experienced spontaneous abortions; the remainder had live births; five of the live births were twin pairs.
Procedure
The protocol called for assessing the participants three times during the puerperium: about 3 weeks (time 1), about 4 weeks (time 2), and 4–5 weeks (time 3) postpartum. At the initial postpartum visit (at about 3 weeks), patients were met by a bilingual (English/Spanish-speaking) master’s-level psychologist (C.A.N.), who described the project and obtained written informed consent. At this time the women completed a screening packet consisting of demographic and medical history questionnaires and three self-report forms: the 30-item Inventory of Depressive Symptomatology
(34), the Edinburgh Postnatal Depression Scale
(3,
35), and the Quality of Life in Depression Scale
(36,
37). The women were also interviewed verbally because some women may have been embarrassed to admit that they were unable to read. Each woman was given a free package of diapers for her participation.
Approximately 1 week after the initial assessment (time 2), women whose scores exceeded either the threshold for substantial depressive symptoms (a score of 18 on the Inventory of Depressive Symptomatology or a score of 12 on the Edinburgh Postnatal Depression Scale) at time 1 were contacted by telephone and the questionnaires were repeated. Women who continued to score above either threshold at time 2 were seen about 1 week later for a third assessment and given the Structured Clinical Interview for DSM-IV, Clinician Version (SCID)
(38). Women who participated in the third clinical interview received a $20 gift certificate to a grocery store in the area.
Participants whose scores were below both of the thresholds for depressive symptoms during the initial assessment (time 1) were not included in the time 2 or time 3 assessments. Consequently, 463 women who had no substantial symptoms at the initial assessment concluded their participation after the first assessment. To affirm our assumption that women screening negative initially at about 3 weeks postpartum would not subsequently develop depression over the next month, the first 42 participants who screened negative for depressive symptoms during the initial assessment were followed for both a time 2 and a time 3 assessment. No woman in this group subsequently developed depressive symptoms (i.e., crossed either of the stated thresholds).
A concern was that depressed women would be less likely to keep their postpartum clinic appointments. Therefore, we investigated a second subgroup of 50 randomly selected patients who did not go to the clinics at the appointed times. These women were contacted and screened by telephone with the same instruments. Analysis of this subgroup revealed no differences in initial screening results from the study participants (data available upon request).
Questionnaires
Every participant completed a demographic information form that included the following: age, ethnicity, language(s), gravidity, parity, date of parturition, current pregnancy status, familial environment, employment status of participant and partner (if applicable), enrollment in government assistance programs, educational level (1=elementary school, 2=some secondary school, 3=high school diploma or General Equivalency Diploma, 4=some college, 5=college degree), and breast-feeding status. A brief medical history form requesting information regarding current medical problems, obstetric complications, current medications, and contraceptive methods was also administered.
Two scales were used to evaluate depressive symptoms. The Edinburgh Postnatal Depression Scale
(3,
35) is a 10-item, multiple-choice self-report scale developed specifically for the assessment of postnatal depression. This scale was previously translated into Spanish
(39); we field-tested the form and made minor modifications that would optimize its use with Latina women in Dallas County. Scores on this scale range from 0 to 30; higher scores indicate more depressive symptoms. The Inventory of Depressive Symptomatology
(34) is a 30-item scale designed to assess the severity of depression for either inpatients or outpatients. Possible scores range from 0 to 84, and it requires approximately 15 minutes to complete. This form was previously translated into Spanish and used among Spanish-speaking patients in Dallas County.
Quality of life and functional impairment were evaluated with the Quality of Life in Depression Scale
(36,
37). Results from these questionnaires will be presented elsewhere.
Finally, the SCID
(38) was used to assign psychiatric diagnoses at the third assessment in women who still had elevated scores on either the Edinburgh Postnatal Depression Scale or the Inventory of Depressive Symptomatology at their second assessment. Questionnaires and interviews were administered either in English or Spanish by a bilingual master’s-level clinician (C.A.N.). Both were trained in the administration of the SCID and achieved interrater reliability greater than 0.80. These individuals were not blind to patients’ scores on the Edinburgh Postnatal Depression Scale and Inventory of Depressive Symptomatology.
Statistical Analysis
Using previously conducted validity studies, we set the threshold for declaring clinically significant depressive symptoms at time 1 at 12 or higher on the Edinburgh Postnatal Depression Scale
(35,
39) or 18 or higher on the Inventory of Depressive Symptomatology
(34). Major depressive disorder at time 3 was defined as meeting DSM-IV criteria on the SCID. Differences in the onset of depressive symptoms among different ethnic groups were explored with chi-square analysis. The following variables were used to compare depressed women (i.e., those scoring above the two thresholds at the initial and second interviews) with the nondepressed women: age, breast-feeding (yes or no), education (level 0 or 1, 2, 3, 4, or 5), race (white, African American, Hispanic, other), language (English or Spanish), number of pregnancies, receiving government assistance (yes or no), number of children, number of babies, employment (yes or no), employment of spouse (yes, no, or no spouse), living at home with spouse (yes or no), living at home with parents (yes or no), living at home with extended family (yes or no), living at home with significant other (yes or no). All variables that were significant at a 0.05 level were entered into multiple regression models to test the association between each measure and depressive symptoms. Since the two screening instruments may have performed differently, models for women who scored higher than the threshold for either were also investigated.
Logistic regression analysis was used to predict risk for depressive symptoms at time 1 or persistent depressive symptoms at time 2 according to threshold definitions on the Edinburgh Postnatal Depression Scale or Inventory of Depressive Symptomatology. Women whose scores were below threshold at time 1 were designated as euthymic at time 2, since no women in our subgroup of women scoring below threshold at time 1 subsequently had a score above threshold on either scale at time 2. Demographic data and scores at time 1 were used to develop a model for predicting the full syndrome of major depressive disorder, defined by the SCID at time 3. We repeated this model using time 2 scores. A model for predicting the onset of major depressive disorder in women with postpartum illness was also investigated. Finally, receiver operating characteristic curve analysis was used to compute curves that could establish thresholds for the Edinburgh Postnatal Depression Scale and Inventory of Depressive Symptomatology for women evaluated at time 2. Again, we assumed that women who initially scored negative would remain negative for the syndrome of major depressive disorder. Sensitivity, specificity, positive predictive value, and negative predictive value were computed for the optimal thresholds. The quality index of efficiency was determined by weighted averages of sensitivity and specificity estimates
(40).
Results
Depressive Symptoms at Time 1 or Time 2
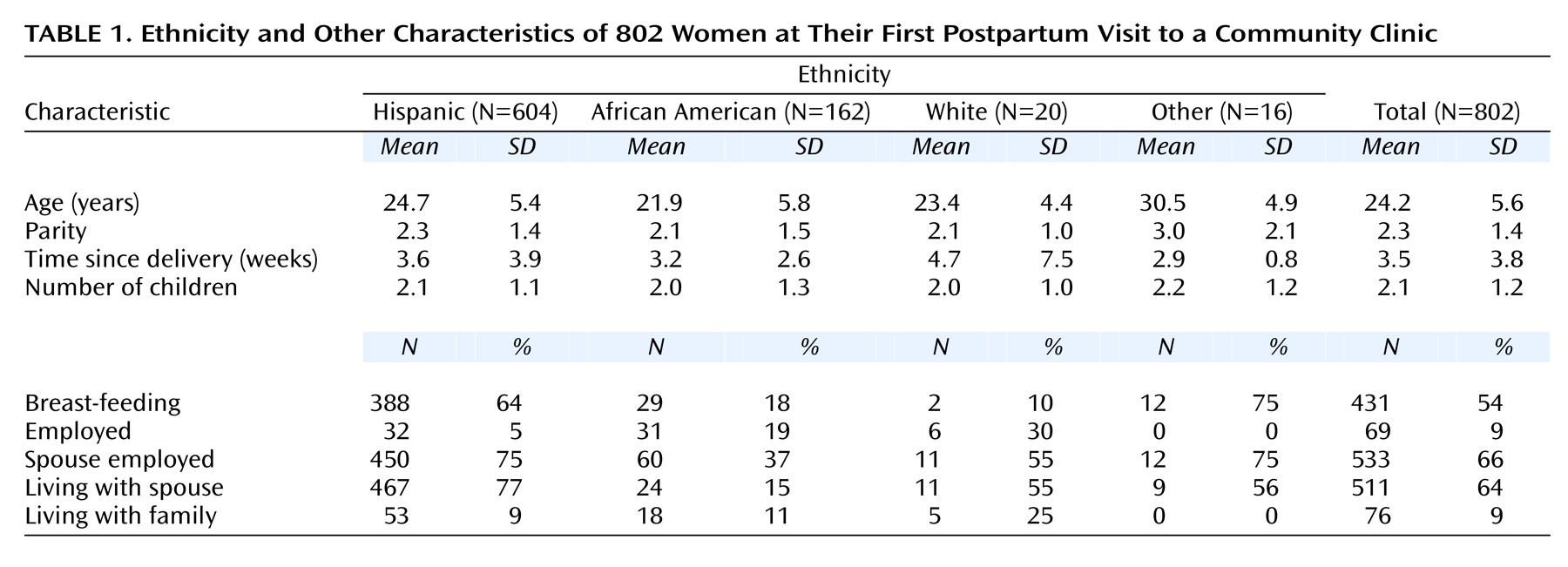
Table 1 shows the patients’ demographic characteristics.
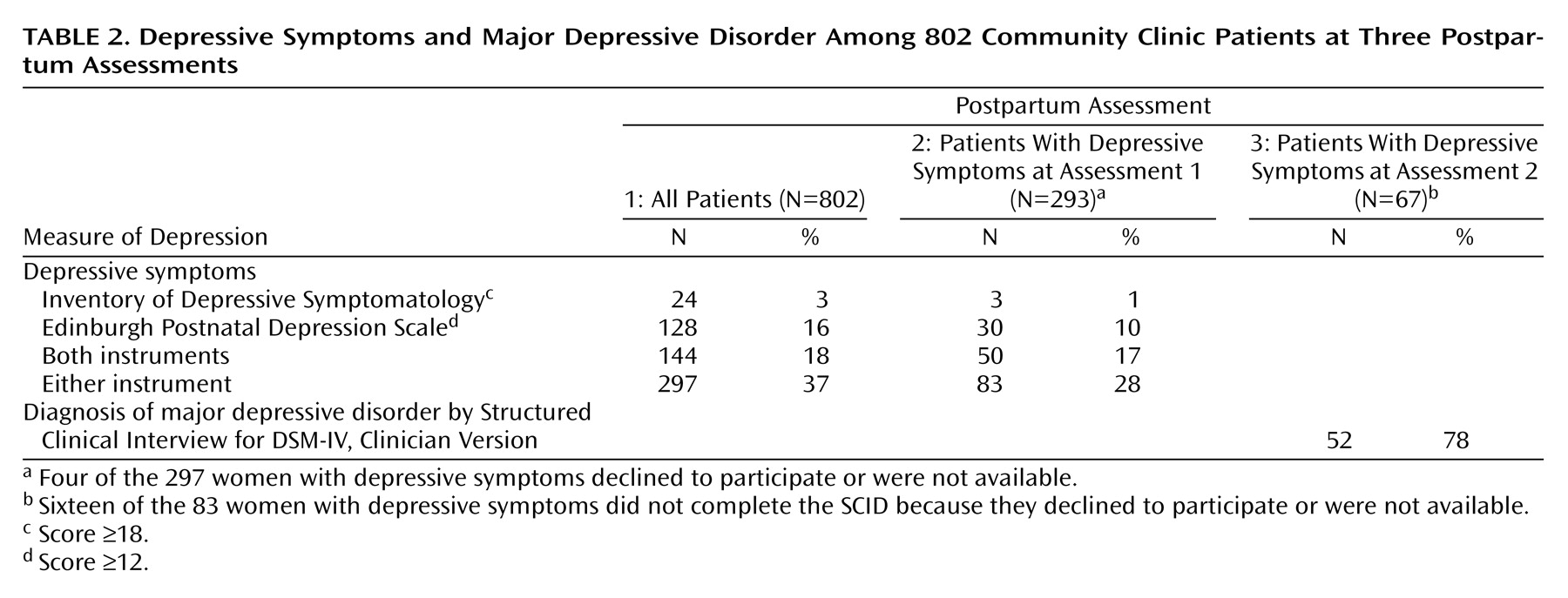
Table 2 shows the percentages of women with symptoms of depression at time 1 and time 2 or the diagnosis of major depressive disorder at time 3.
Table 2 also shows how many patients met criteria for depressive symptoms on the Edinburgh Postnatal Depression Scale or the Inventory of Depressive Symptomatology.
Only four of the 297 women with depressive symptoms at the first visit were not available or declined to participate in the second evaluation. Eighty-three (28%) of the 293 depressed women evaluated at time 2 continued to report depressive symptoms above threshold on one or both of the instruments (
Table 2).
At time 3, 67 (81%) of the 83 women who had depressive symptoms at time 2 completed the SCID; 52 (78%) of these 67 women met DSM-IV criteria for major depressive disorder. However, only 26 (50%) of the 52 women reported onset of depressive symptoms during the postpartum period; 13 (25%) reported onset during pregnancy, and 13 (25%) reported onset before pregnancy. In addition, six women met criteria for minor depressive disorder, and one was diagnosed as having bipolar disorder, depressed phase. Thus, the rate of major depressive disorder in the entire group of women during the first month postpartum was from 6.5% (if no woman lost to follow-up was depressed) to 8.5% (if all women lost to follow-up were depressed). For postpartum-onset major depressive disorder the rate would be between 3.2% and 5.2%.
There were substantial differences between ethnic groups in the rates of depressive symptoms at time 1 and time 2 and in the rates of the syndrome of major depressive disorder at time 3. For this analysis, only the African American (N=162) and Hispanic (N=604) groups were compared because there were too few women in the other ethnic groups. Among African American women, 72 (45%) and 24 (34%) of those evaluated had clinically significant depressive symptoms at time 1 and time 2, respectively. Eleven (46%) of the 24 African American women who participated in SCID interviews at time 3 had major depressive disorder. Given that nine women were lost to follow-up, the overall rate of major depressive disorder in African American women was between 6.8% and 12.3%.
The corresponding rates of depression in the Hispanic women differed slightly: 214 (35%) and 55 (26%) had significant depressive symptoms at time 1 and time 2, respectively. Twenty-nine (53%) of the 55 Hispanic women referred for interview at time 3 had major depressive disorder. Sixteen Hispanic women were lost to follow-up, which yields an estimate for major depressive disorder between 4.8% and 7.4%. The difference between the African American and Hispanic groups in depressive symptoms was significant at time 1 (χ2=5.4, df=1, p=0.02) but not at time 2 or time 3.
The capacity to speak English may be a rough measure of acculturation. Therefore, we compared Spanish-only speakers (N=489) with those who also spoke English (N=115) among the Hispanic women. The difference was significant at time 1 between Spanish-only-speaking and bilingual women; 162 (33%) of Spanish-only-speaking women had depressive symptoms, but 50 (43%) of the bilingual Hispanic women were depressed (χ2=4.04, df=1, p=0.04). No differences in rates of depressive symptoms at time 2 or in rate of major depressive disorder at time 3 were found between Hispanic women who could or could not speak English.
Factors Predicting Depressive Symptoms or Major Depressive Disorder
For the women who met either threshold definition (i.e., on the Edinburgh Postnatal Depression Scale or the Inventory of Depressive Symptomatology) at time 1, the following factors significantly predicted depressive symptoms: being more highly educated (odds ratio=1.65, confidence interval [CI]=1.10–2.50, p=0.01), having some secondary school education (odds ratio=1.96, CI=1.27–3.02, p=0.002), and having graduated from high school or some college education (odds ratio=1.80, CI=1.01–3.20, p=0.05). On the other hand, women who were breast-feeding were less likely to have depressive symptoms (odds ratio=0.60, CI=0.44–0.81, p=0.008).
The risk of persistent depressive symptoms exceeding the threshold on either the Edinburgh Postnatal Depression Scale or the Inventory of Depressive Symptomatology at time 2 was lower among women having some college education (odds ratio=0.22, CI=0.06–0.76, p=0.02) and those living with their spouse or significant other (odds ratio=0.49, CI=0.28–0.84, p=0.01). When women were defined by threshold depression scores on the Edinburgh Postnatal Depression Scale only, women who had additional babies at home had a greater risk of having depressive symptoms (odds ratio=1.40, CI=1.06–1.77, p=0.01).
The first model for predicting major depressive disorder at time 3 used time 1 data. The predictors of major depressive disorder were the time 1 Edinburgh Postnatal Depression Scale score, time 1 Inventory of Depressive Symptomatology score, and living at home with extended family. For every point increase in the time 1 score on the Edinburgh Postnatal Depression Scale, the chance of having the syndrome of major depressive disorder at time 3 was increased by 15% (95% CI=1.06–1.25, p=0.0008), and a 1-point increase in the time 1 score on the Inventory of Depressive Symptomatology increased the chance of major depressive disorder by 9% (95% CI=1.05–1.14, p=0.0001). Also, living at home with extended family (rather than living with a spouse or significant other) resulted in a three-fold increase in the chance of major depressive disorder at time 3 (95% CI=1.23–7.17, p=0.02).
In regard to the prediction of major depressive disorder with postpartum onset (N=26), for every point increase in the time 1 score on the Edinburgh Postnatal Depression Scale, the chance of having postpartum-onset major depressive disorder at time 3 was increased by 15% (95% CI=1.04–1.27, p=0.006). In addition, a 1-point increase in the time 1 score on the Inventory of Depressive Symptomatology increased the chance of postpartum-onset major depressive disorder by 6% (95% CI=1.02–1.11, p=0.006). Also, living at home with a spouse or significant other resulted in a 3.3 times greater chance of postpartum-onset major depressive disorder (95% CI=1.10–10.12, p=0.03). The predictive value of the Edinburgh Postnatal Depression Scale was significant, even when both Edinburgh Postnatal Depression Scale scores and Inventory of Depressive Symptomatology scores were included in the model.
The second model used the time 2 data. The Edinburgh Postnatal Depression Scale was still predictive: a 1-point increase in score on the Edinburgh Postnatal Depression Scale increased the odds of major depressive disorder by 14% (95% CI=1.01–1.30, p=0.03). In addition, the Inventory of Depressive Symptomatology was also predictive: each additional point scored on this measure increased the risk by 13% (95% CI=1.06–1.20, p=0.0001). When the outcome was major depressive disorder with postpartum onset, only the Inventory of Depressive Symptomatology was predictive at time 2 (odds ratio=1.09; 95% CI=1.06–1.13, p=0.0001).
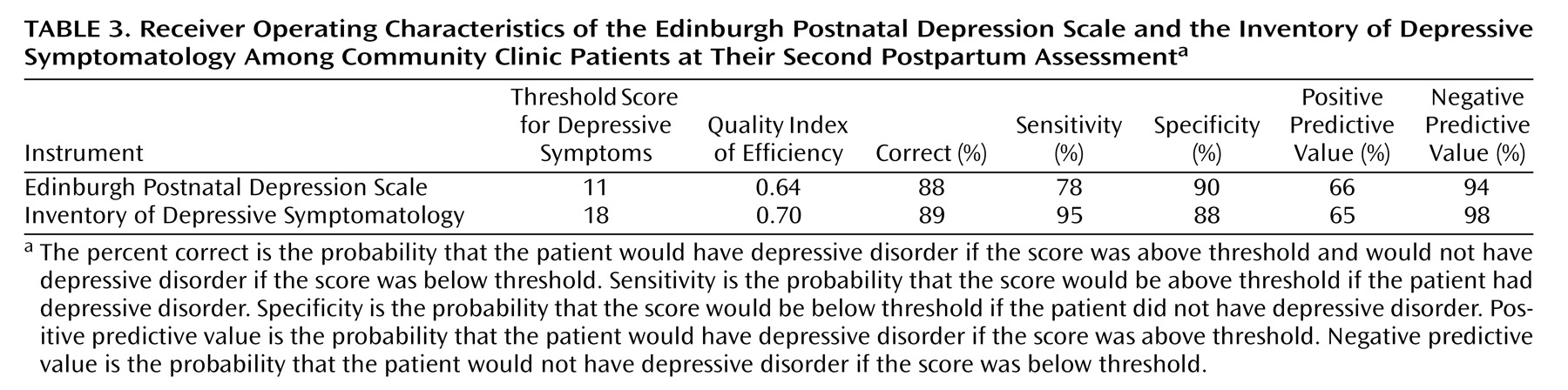
The receiver operating characteristics of each scale were investigated by using the time 2 data. As shown in
Table 3, the quality index of efficiency was highest for Inventory of Depressive Symptomatology scores, suggesting slight superiority for this screening scale when used at about 4 weeks postpartum. The optimal threshold for screening with the Edinburgh Postnatal Depression Scale was 11; for the Inventory of Depressive Symptomatology the optimal threshold was 18.
Discussion
This study reports the point prevalence of postpartum major depressive disorder among ethnic minority women, most of whom were Hispanic, who were receiving care in a large publicly funded maternal health system. As such, to our knowledge, it is the largest study group of women in the United States screened from such a setting and represents the largest database on the prevalence and risk of postpartum depression in minority women. We found that the rate of major depressive disorder during the postpartum period was between 6.5% and 8.5%. Surprisingly, only 50% of the women with major depressive disorder developed the current episode following delivery; 25% developed the episode during pregnancy.
Our hypothesis that the rate of postpartum major depressive disorder would be higher in this multiethnic, socioeconomically disadvantaged group compared with rates reported in the literature among predominately white, middle-class groups was not supported. The rate for major depressive disorder with postpartum onset in the United States reported by O’Hara and colleagues
(14,
31) was 4%, which is similar to our rate for postpartum onset (3.2%–4.2%). Even though the study group size was smaller, the rate found by O’Hara et al. is particularly strong because they followed women longitudinally during pregnancy and the postpartum period
(14). These rates are well below the point prevalence reported by Hobfoll and colleagues
(1), but we do not know the number of women in that report who had onset of illness after delivery. It is interesting to note that researchers from the United Kingdom found rates as high as 15% for major depressive disorder in postpartum women
(41). Rates for major depressive disorder vary among countries, however, making comparisons with other countries and cultures difficult
(42).
The finding that half of the women who were experiencing a major depressive episode postpartum actually had the onset of the disorder before delivery is important and confirms work conducted in smaller groups
(4,
13,
14,
24,
31,
32,
43). The rates of major depressive disorder for ethnic minority women who are not necessarily postpartum reported in epidemiologic studies
(44) are similar to our rates for ethnic minority women with major depressive disorder (between 4.8% and 7.4% in Hispanic women and 6.8% and 12.3% in African American women). This means that either the postpartum period is not a time of substantial increase for risk of depression
(19) or that the duration of illness episodes is brief. Health care professionals should conduct broad screening for major depressive disorder and include pregnant women in screening efforts. Ethnic minority groups appear to be at high risk for major depressive disorder, whether or not they are postpartum, a fact that has not received adequate attention
(44).
Even though the rates of major depressive disorder and minor depressive disorder during the postpartum period in this study are no higher than for women in general, the rates of clinically significant depressive symptoms are impressive. More than one-third of women endorsed clinically significant mood symptoms at their 3-week postpartum visit, which decreased but remained high (nearly 10%) during the second postpartum assessment. The resolution of normative postpartum symptoms that overlap with the symptoms of depression (e.g., fatigue) in the first few weeks may have contributed to the decrease from the first to the second assessment
(23,
45). This may also be the reason that the performance on the Inventory of Depressive Symptomatology, which includes questions about the physical symptoms associated with depression, improved at the second screening. Alternatively, this change in rate of depressive symptoms between the first and second postpartum assessment may be attributable to a resolution of biological changes that lead to mood symptoms. In this sense, depressive symptoms within the first few weeks may result from changing hormone levels during the immediate postpartum period and may be viewed as an extended period of the “maternity blues.” Yet another possibility is that concern and anxiety over mothering tasks contributed to depressive symptoms and that this diminished over the first few weeks postpartum.
Since clinically significant depressive symptoms will improve over the course of several weeks postpartum for many women, it would be useful to determine which women are likely to stay symptomatic so that early interventions can be employed and premature interventions can be avoided for those with only transient symptoms. Our models found that women with more severe depression at 3 weeks were likely to remain persistently depressed. Receiver operating characteristic curve analysis suggests that a score over 11 on the Edinburgh Postnatal Depression Scale or over 18 on the Inventory of Depressive Symptomatology at 4 weeks postpartum can be very helpful in identifying women likely to have a syndrome of major depressive disorder. These tools can easily be implemented in busy clinical settings.
Depressive symptoms at the first postpartum visit, 3 weeks after delivery, were predicted by higher levels of education, which was an unexpected finding but may also indicate a higher degree of acculturation among Hispanic women, who were the predominant group in our cohort. Along these lines, Hispanic women who spoke both English and Spanish were at higher risk of depressive symptoms. On the other hand, being in the group of women who were breast-feeding was associated with a lower likelihood of symptoms, a finding observed by some
(46,
47), but not others
(48). There may be protective psychosocial and biological factors that accompany breast-feeding. Alternatively, positive feelings toward the pregnancy appear to function as a buffer against postpartum depression
(12,
49), and the interest and motivation to breast-feed may reflect such a positive attitude.
Having other small children at home increased the likelihood that depressive symptoms would persist into the second postpartum assessment. Other work
(50) suggests that having small children at home increases the risk of depression in socioeconomically disadvantaged women, but one study
(5) failed to show this was predictive of postpartum depression. Our findings are not inconsistent with either view, since half of our patients developed major depressive disorder before delivery.
In the univariate analyses, we saw a protective effect against persistent symptoms for women who were living with a spouse or significant other. Living with extended family may indicate the absence of a confidant or spouse, which is consistent with findings from others on the risk of postpartum depression
(10,
51). However, other explanations may be operative because we did not specifically ask our patients about disruptions in marital or other significant relationships; for example, the need to live with other family members may have indicated more dire financial circumstances.
Several methodological limitations in this study are noteworthy. Although women reported an onset of depression before parturition, all of our assessments were conducted after delivery and are liable to retrospective reporting bias. However, we saw women within weeks after delivery, thus minimizing the chance of inaccurate reports. Further, given the valence associated with an event like parturition, it is likely that women would overreport rather than underreport the postpartum onset. Second, our time frame of 1 month for assessing the point prevalence for depression is much briefer than that in many reports in the literature (3–6 months). However, it is consistent with the DSM-IV definition and probably encompasses women in whom the biology of parturition influenced illness onset. Moreover, our rate is consistent with rates found by others in the United States, suggesting that the rate in minority women is reliable. Finally, we did not screen all women at these four clinics. However, we systematically screened all women during selected days, and we investigated a subgroup of women who failed to keep their appointments. This suggests that our findings are representative of the group as a whole.