Major depression is the most common psychiatric disorder associated with suicide and attempted suicide
(1). The presence of depression may be necessary but is insufficient to explain suicidal behavior in individuals who have major depression, since most patients with major depression never make a suicide attempt. Studies have identified impulsivity and aggression as correlates of a history of suicide attempts
(2–
4). Impulsivity is regarded as a trait that predisposes an individual to engage in self-destructive behavior in response to suicidal thoughts. A diathesis-stress model of suicide has been proposed in which an impulsivity/aggression factor is part of the diathesis that interacts with stressors that trigger the person to act
(2).
The term “impulsivity” has been used in relation to a variety of loosely defined constructs, such as 1) a personality trait or cognitive style characterized by disinhibition, 2) a tendency to act quickly on urges or to stimuli, and 3) a class of psychiatric disorders characterized by behavioral dyscontrol. Impulsivity has been found to be associated with suicidal and self-destructive behaviors within various adult psychiatric populations
(3,
4). In individuals with borderline personality disorder, impulsivity is the personality trait most predictive of suicidal behavior
(3). Moreover, Herpertz and Favazza
(4) found that clinical and biological measures of trait impulsivity were higher in individuals with a history of self-mutilation than in those without such a history. Suicidal behavior has been found in association with impulse control disorders such as compulsive gambling
(5). Low serotonergic activity, a biological correlate of impulsive aggression toward person or property
(6–
8), has also been associated with suicidal behavior
(9–
12). Such studies suggest a common psychopathologic and biologic substrate for impulsivity, impulsive aggression, and suicidal acts.
Early childhood trauma has been associated with self-destructive and suicidal behavior later in life
(13–
15). Although the reason for this association is unclear, the high prevalence of a childhood abuse history among populations with a borderline personality (characterized by impulsivity and self-injury) has stimulated investigation into the mechanism whereby childhood abuse influences personality development
(16–
19). The association between childhood trauma and self-destructive behavior in adulthood may be mediated in part by a relationship between abuse history and the development of the biological underpinnings and the psychological aspects of the trait of impulsivity. Impulsivity and aggression may be personality traits that develop or are more pronounced in response to early childhood experiences of trauma and loss. For example, there is evidence of a relationship between maternal deprivation, low serotonin levels, and aggression in monkeys
(20). However, the relationship between childhood abuse, impulsivity/aggression, and suicidal behavior has received very little study in human psychiatric populations.
This study investigated the relationship of reported childhood trauma to impulsivity, aggression, and suicidal behavior in depressed adults. We hypothesized that impulsivity and aggression would be related to a reported history of childhood abuse and thereby mediate the relationship between childhood abuse and suicidal behavior in adulthood. We hypothesized that a higher frequency of childhood trauma would be reported by depressed adults with higher levels of adult trait impulsivity, aggression, and suicidal behavior. We measured trait impulsivity, aggression history, number of previous suicide attempts, and the medical lethality and intent to die associated with the most lethal attempt in a group of depressed adult inpatients; these variables were then compared between subjects with and those without a reported history of childhood physical or sexual abuse.
Method
Subjects
Patients (N=136) who met DSM-III-R criteria for major depressive episode according to the Structured Clinical Interview for DSM-III-R (SCID) were entered into the study. After complete description of the study to the subjects, written informed consent was obtained. The study protocol was approved by our institutional review board. Exclusion criteria were current substance or alcohol abuse, neurological illness, or other active medical conditions. The presence or absence of physical or sexual abuse before the age of 15 was determined by responses to three direct questions from the Columbia Demographic and Treatment History Interview; lifetime history of suicide attempts was obtained with the Columbia Suicide History Form (both instruments available from J.J.M.). The Columbia Suicide History Form is a semistructured instrument that elicits information about lifetime suicide attempts, the method employed, medical lethality, precipitants, and surrounding circumstances. A suicide attempt was defined as a deliberate self-destructive act with some degree of intent to end one’s life. Lethality was measured by the Suicide Lethality Scale
(21), which assesses objective medical damage and treatment. Suicidal intent at the time of the most lethal suicide attempt was assessed by using the Suicide Intent Scale
(21). Rater reliability (intraclass correlation coefficients [ICCs]) on suicide interview measures was high (ICC=0.94–0.99). Depressive symptoms immediately before admission to the hospital were assessed with the Hamilton Depression Rating Scale
(22). Rater reliability for the Hamilton depression scale was also high (ICC=0.97). Impulsivity was measured with the Barratt Impulsivity Scale
(23), a self-report instrument that has validity and reliability in the measurement of trait impulsivity. Aggression history was assessed with the Brown-Goodwin Aggression Inventory
(24) (reliability ICC=0.96). The Hopelessness Scale
(25) is a self-report scale that was administered to measure state levels of hopelessness. The presence or absence of borderline personality disorder was determined by assessing axis II personality disorder pathology with the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Rater reliability on diagnostic interview measures was adequate (SCID: ICC=0.80; SCID-II: ICC=0.70).
The subjects were recruited at two university hospital sites, one in New York City (N=47) and the other in Pittsburgh (N=89). The study groups from the two sites were comparable in all variables except for a modest difference in age: the New York subjects (mean age=39.5 years, SD=12.9) were 4.6 years older than the Pittsburgh subjects (mean=34.9, SD=11.1) (t=–2.2, df=134, p=0.03).
Data Analysis
Student’s t tests compared demographic, suicide, impulsivity, aggression, and depression measures between abused and nonabused groups. Chi-square analyses compared groups with respect to dichotomous variables.
Analyses were also conducted to estimate effects of a comorbid borderline personality disorder diagnosis. Univariate analyses compared differences in impulsivity, aggression history, reported abuse history, and suicide attempt status between depressed subjects who met criteria for borderline personality disorder and those who did not.
A logistic regression analysis was performed for the dichotomous variable of suicide attempt status, with abuse history, impulsivity, and three other covariates of abuse history (sex, race, and borderline personality disorder diagnosis) as predictor variables. Among the subgroup of patients who had a previous suicide attempt (N=73), a linear regression analysis was performed for the number of previous suicide attempts, with abuse history and impulsivity scores as predictor variables. In order to use parametric tests, the number of previous suicide attempts was transformed by taking the square root to normalize the distribution.
Results
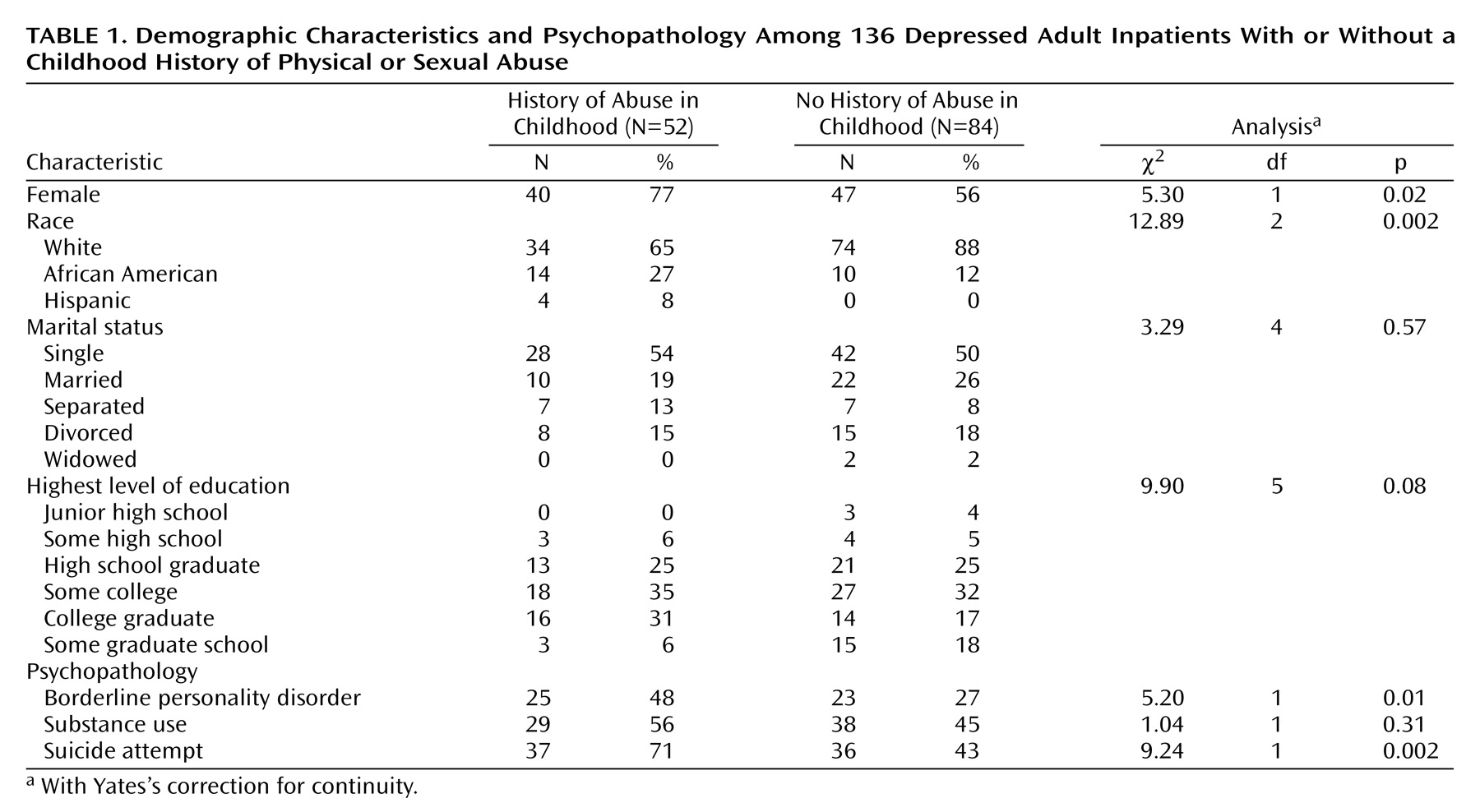
Of the 136 subjects, 52 (38%) reported a history of physical or sexual abuse before the age of 15 years, and 84 (62%) reported no childhood abuse. There was no difference in age between the abused (mean=35.4 years, SD=11.4) and nonabused (mean=37.2 years, SD=11.9) subjects (t=–0.88, df=134, p=0.37). Other demographic characteristics of the abused and nonabused groups are reported in
Table 1. There was no difference in marital status or educational level between abused and nonabused subjects. Subjects reporting a history of childhood abuse were more likely to be female and were more likely to be African American or Hispanic than were those who did not report childhood abuse.
Subjects who reported abuse were more likely to have a comorbid diagnosis of borderline personality disorder than those who did not report abuse and were also more likely to have made a suicide attempt (
Table 1).
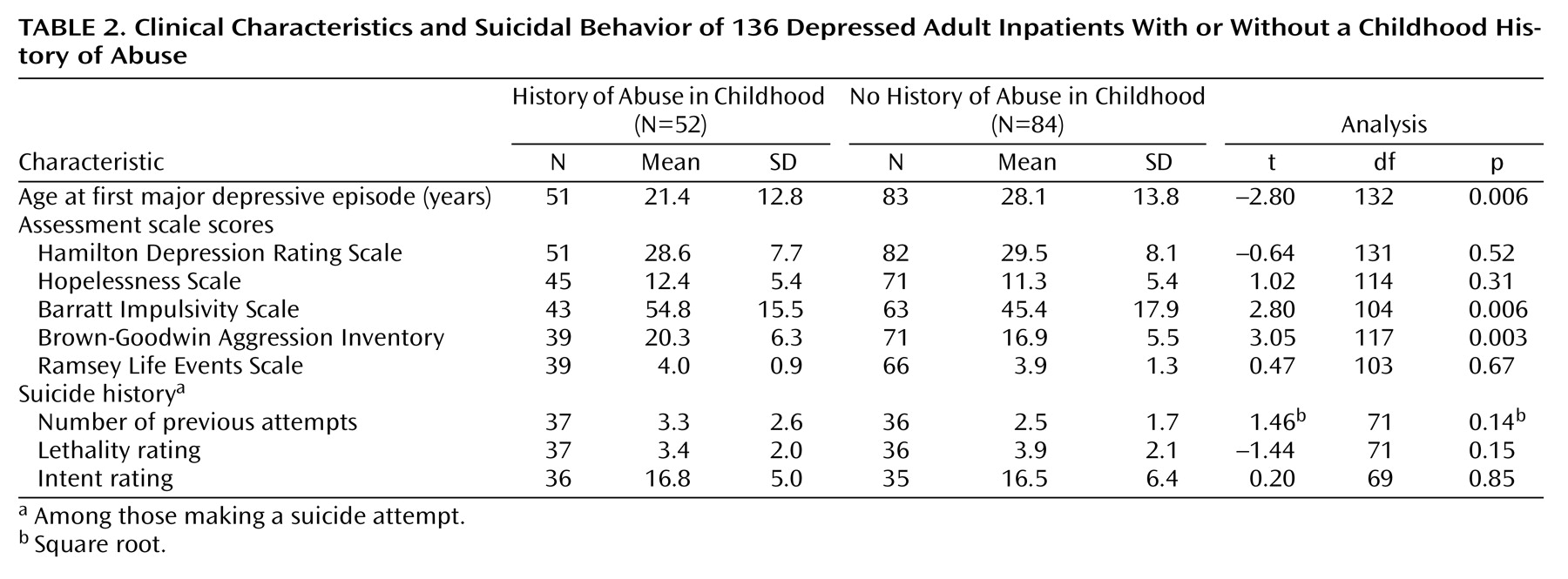
Table 2 lists the differences between abused and nonabused groups on clinical characteristics and other suicidal history variables. Subjects who reported a history of childhood physical or sexual abuse had significantly higher impulsivity and aggression scores than did those with no history of abuse. There was no significant difference in severity of depression or levels of hopelessness at the time of admission between those who reported a history of abuse and those who did not.
Barratt Impulsivity Scale scores were significantly higher in subjects who had a history of at least one suicide attempt (mean=52.3, SD=16.8) than in those who had never attempted suicide (mean=45.7, SD=17.8) (t=–2.17, df=104, p=0.05). Brown-Goodwin Aggression Inventory scores were significantly higher in subjects who had a history of at least one suicide attempt (mean=19.8, SD=6.2) than in those who had never attempted suicide (mean=16.3, SD=5.2) (t=3.30, df=104, p=0.001).
Among the subgroup of patients with a previous suicide attempt (N=73), the number of previous attempts and the lethality and intent to die associated with the most lethal attempt did not differ between those with a history of abuse in childhood and those without (
Table 2). In a linear regression analysis among subjects with previous suicide attempts, the square root of number of previous suicide attempts was not predicted by abuse history (beta [β]=0.13, SE=0.16; t=0.88, df=47, p=0.38), impulsivity (β=0.17, SE=0.005; t=1.09, df=47, p=0.28), or aggression (β=0.00, SE=0.01; t=0.01, df=47, p=0.99). The mean age of the first suicide attempt was lower in the abused group (mean age=22.7 years, SD=11.4) than in the nonabused group (mean=28.7, SD=12.7) (t=–2.1, df=72, p=0.04). Of the 37 suicide attempters who reported a history of childhood abuse, 17 (46%) made their first suicide attempt before the age of 18. Of the 36 suicide attempters without a history of childhood abuse, seven (19%) made their first attempt before age 18 (Yates’s correction for continuity: χ
2=4.67, df=1, p<0.03).
In analyses that compared subjects with and without a comorbid diagnosis of borderline personality disorder, abuse history (χ2=5.15, df=1, p=0.02) and attempt status (χ2=17.83, df=1, p<0.0001) were significantly related to a comorbid borderline personality disorder diagnosis. In a subset of 108 subjects for whom we had measures of borderline personality disorder and impulsivity, Barratt Impulsivity Scale scores were higher among those with borderline personality disorder (mean=55.33, SD=18.12) than in those without the comorbid diagnosis (mean=46.0, SD=16.5) (t=–2.64, df=104, p=0.01). Brown-Goodwin Aggression Inventory scores were higher among those with borderline personality disorder (mean=17.4, SD=6.1) than in those without the comorbid diagnosis (mean=20.1, SD=5.6) (t=–2.34, df=118, p=0.02).
A univariate analysis was performed to examine the relationship between abuse history and suicide attempt status after we controlled for the presence of borderline personality disorder. In the subgroup of depressed subjects that did not meet criteria for comorbid borderline personality disorder (N=88), those who reported a history of abuse were significantly more likely to have made a previous suicide attempt (46%, N=16 of 35) than those without a history of abuse (21%, N=11 of 53) (Yates’s correction for continuity: χ2=5.01, df=1, p=0.03). There was no difference in suicide attempt status between the 25 borderline personality disorder subjects who reported a history of abuse (84%, N=21) and the 23 borderline personality disorder subjects who reported no history of abuse (74%, N=17) (p=0.49, Fisher’s exact test).
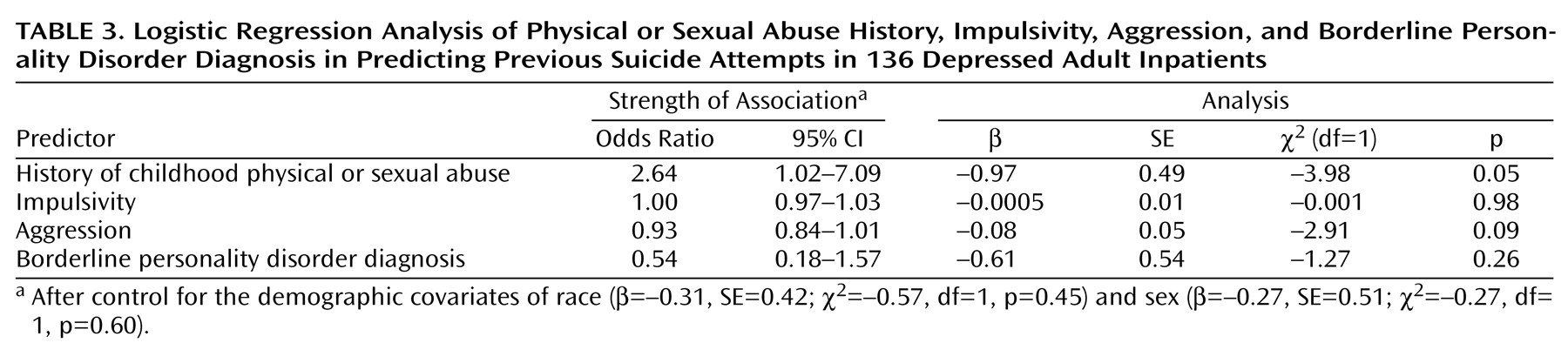
In a logistic regression analysis of abuse history, impulsivity, aggression history, and borderline personality disorder in the prediction of suicide attempt status, we found that after we adjusted for borderline personality disorder, impulsivity, and aggression history, abuse history remained significantly associated with attempter status (
Table 3). Demographic covariates of abuse history (sex and race) did not affect the relationship of abuse history to suicide attempt status. In testing for second-order interactions between abuse history and borderline personality disorder, abuse history and sex, and borderline personality disorder and sex, we found no significant interactions in relation to suicide attempt status. Similarly, no third-order interaction was found among abuse history, borderline personality disorder, and sex in relation to suicide attempt status.
Discussion
Our main finding was that depressed adults who reported a history of either physical or sexual abuse in childhood were more likely to have made a previous suicide attempt than those who did not report a history of abuse. They also had higher levels of trait impulsivity, higher levels of aggression, and a higher rate of comorbid borderline personality disorder. Thus, a childhood abuse history is associated with both suicidal behavior and impulsivity in depressed adults. These findings are comparable to those of other studies that have found associations between childhood abuse history and adult psychopathology
(26–
29) in general and between childhood abuse history and self-destructive behavior (such as self-mutilation) and suicidal ideation, gestures, and attempts in particular
(13,
30,
31).
In addition, our findings indicate that, after we adjusted for impulsivity and aggression, abuse history is still significantly associated with suicide attempt status. Therefore, the presence of impulsivity and aggression do not seem to mediate the relationship between abuse history and suicidal behavior. It is possible that the experience of physical or sexual abuse in childhood constitutes an environmental factor that influences the development of both trait impulsivity/aggression and suicidality.
There is also evidence from this study that childhood abuse contributes to an earlier age at onset of suicidal behavior and that it is related to suicidal behavior beginning in childhood and adolescence. This is similar to findings of Kaplan et al.
(32), who found that victims of abuse were more likely than nonvictim comparison subjects to have been suicidal at a younger age.
Alternatively, there is a possibility that impulsivity is mainly an inherited trait underlying both the childhood abuse (perhaps at the hands of a first-degree relative with trait impulsivity and aggression) as well as the manifestation of adult trait impulsivity and aggression
(33,
34). Despite the fact that impulsivity and aggression levels are higher in depressed adults who report childhood abuse, abuse history is likely to be only one factor contributing to trait impulsivity and aggression. For example, there is evidence from nonhuman primate studies
(20) that both genetic transmission as well as environmental factors such as maternal deprivation contribute to the presence of biological correlates of impulsivity. Peer-raised monkeys reset their CSF 5-hydroxyindoleacetic acid levels at a lower level compared to maternally raised monkeys, and this effect endures for years and is associated with impulsive and aggressive behaviors. Therefore, impulsivity may be an inherited trait that is worsened by environmental experiences of abuse. Along these lines, recent studies of the relationship of hypothalamic-pituitary-adrenal axis dysfunction to posttraumatic stress disorder in psychiatric populations indicate that traumatic experience may have long-lasting neurobiological effects on humans that contribute to psychopathology
(35).
Additionally, abuse history and impulsivity are two of a number of risk factors for suicidal behavior. A history of childhood abuse is possibly associated with other risk factors, such as vulnerability to certain environmental triggers. Furthermore, there is evidence that postabuse protective factors such as the presence of a caring adult
(13) as well as involvement in sports throughout childhood/adolescence and high quality of adult relationships
(36) can mediate between abuse history and adult psychopathology. Thus, a comprehensive approach should view suicidal behavior within a framework of concurrent psychological and biological lines of development
(16,
37).
Another related finding of this study is that level of trait impulsivity and aggression, and not the objective severity of depression, is significantly associated with suicide attempt status. This is consistent with our previous finding that objective severity and duration of depressed mood is not associated with higher risk for suicide among depressed inpatients
(38). Brent et al.
(39) also found that, while psychopathology in first-degree relatives of adolescent suicide victims does not fully account for the familial transmission of suicidal behavior, higher levels of aggression are associated with higher familial loading for suicidal behavior. These findings lend support to a stress-diathesis model of suicidal behavior that considers the biological and personality traits that might lower an individual’s threshold for acting on mood states, suicidal ideation, or other state or environmental triggers
(2).
Although abuse history and impulsivity were predictive of suicide attempt status, they were not associated with differences in severity of suicidal behavior, such as the number of previous suicide attempts or level of intent associated with the most lethal attempt in this group of depressed inpatients. This differs from another report that found a relationship between childhood abuse and multiple suicide attempts in a general outpatient psychiatric population
(32). This difference might be due to the fact that we controlled for the effects of major depression by limiting our study group to depressed inpatients.
Comorbid borderline personality disorder, while strongly associated with both abuse history and suicide attempt status, does not completely account for the relationship between abuse history and suicide attempt status. However, the presence of a comorbid diagnosis of borderline personality disorder does seem to be associated with higher levels of impulsivity and aggression. Thus, as we have found previously
(3), impulsivity is a characteristic of borderline personality disorder that is associated with the risk to attempt suicide.
One weakness of the present study is its reliance on a broadly defined, retrospective report of abuse history that was not validated by other sources. However, two prospective studies of a birth cohort of New Zealand children studied to the age of 16 support the reliability of the retrospective reporting in the present study. In one, early disadvantageous childhood and family circumstances were identified longitudinally as a common pathway to suicidal behavior in adolescence
(40). In the other, when these same subjects were requestioned at age 18–21 about their childhood exposure to physical and sexual abuse, it was found that there was a 50% false negative rate of reporting in those whose abuse had been documented. These inconsistencies were unrelated to the subjects’ psychiatric state. Among those who were not abused, there were no false positive reports
(41). In addition to documenting the childhood trauma closer to the time that it takes place, prospective studies can consider other observable sequelae of abuse that might contribute to suicidal behavior, such as greater vulnerability to environmental events that might trigger memories of abuse and dissociative states that might impair judgment and cognitive processing. However, such studies take years to complete because the cohort must pass through a major part of the age of risk for suicidal behavior.
Although the present study was unable to explore more detailed dimensions of abuse history such as type, perpetrator, duration, or age at onset of abuse, several studies show that sexual abuse and emotional neglect, more than physical abuse, seem to be associated with suicidal behavior
(42–
44). The specific characteristics of abuse history and their relationship to suicidal behavior warrants further study.
Another weakness of this study is that all of the subjects were clinically referred and were therefore more likely to have a history of abuse or suicidal behavior. However, studies of college students
(44–
46), patients in primary care settings
(44), and other nonclinical populations
(47) have also documented a relationship between abuse history in childhood and suicidal behavior later in life.
These findings suggest that clinicians should be aware of the possibility of a history of childhood abuse in depressed patients with a history of suicide attempts and other impulsive behaviors. Additional research is needed to further identify the relative contributions of heredity and environmental experience to the development of impulsivity, aggression, and suicidal behavior.