Recent epidemiologic surveys in the general population have demonstrated that posttraumatic stress disorder (PTSD) is nearly twice as prevalent among women as men
(1). Furthermore, women exposed to trauma are more than twice as likely as men to develop PTSD
(1), even when history of multiple traumatic events
(2) or sex differences in the type of trauma
(1) are taken into account.
In contrast to community survey respondents, psychiatric patients have not shown gender differences in rates of PTSD
(3,
4). Studies of psychiatric patients have been limited owing to extremely small study groups
(3) or lack of standardized diagnostic assessments of PTSD
(3,
4). Data on gender differences in PTSD among psychiatric patients are scarce because most clinical studies of PTSD have focused on patients seeking treatment for a specific trauma that is predominantly gender related, such as combat or rape.
Another neglected area of research has been the impact of gender on the clinical manifestations of PTSD, such as comorbidity. Data from the National Comorbidity Survey found several differences between men and women with lifetime PTSD in rates of comorbid panic disorder (men: 7.3%; women: 12.6%), substance use (men: 43.2%; women: 27.4%), conduct disorder (men: 43.3%; women: 15.4%), and mania (men: 11.7%; women: 5.7%)
(1). A preliminary study of gender differences in comorbidity with current PTSD among 14 Cambodian young adults found no gender differences in the frequency or number of comorbid diagnoses received, although comorbid somatoform pain disorder was found almost exclusively in women with current PTSD
(5). Another study that compared axis II personality disorders of women with PTSD related to childhood sexual abuse and of male Vietnam veterans with PTSD found strong similarities between the two groups in the pattern of personality disorder features
(6).
The present report from Rhode Island Hospital’s Methods to Improve Diagnostic Assessment and Services project involved treatment-seeking outpatients with current PTSD and used rigorous definitions of axis I and axis II disorders to address the following questions: Do male and female outpatients differ in 1) the frequency with which they meet criteria for PTSD, 2) the index traumas they report, 3) the clinical correlates of PTSD, 4) patterns of comorbid psychiatric disorders, or 5) the proportion of comorbid disorders that are secondary to PTSD?
Method
Semistructured diagnostic interviews were administered to 1,132 patients who sought treatment at an outpatient private practice that is part of a general hospital. This private practice group treats predominantly individuals with medical insurance (including Medicare but not Medicaid) on a fee-for-service basis. Exclusion criteria for the study were age less than 18 years, a history of a developmental disability, or difficulty with the English language.
The patients were interviewed by a diagnostic rater who administered the Structured Clinical Interview for DSM-IV (SCID)
(7) and the antisocial and borderline sections of the Structured Interview for DSM-IV Personality
(8). For all axis I disorders, “current” was defined as meeting the DSM-IV diagnostic criteria for each disorder at the time of the evaluation. The hospital’s institutional review committee approved the research protocol, and all patients provided informed, written consent.
Throughout the Methods to Improve Diagnostic Assessment and Services project, ongoing supervision of the raters included weekly diagnostic case conferences involving all members of the team. During the study, joint interview diagnostic reliability information was collected on 26 patients. These 26 patients were randomly selected for reevaluation from the larger study group of 1,130 patients. For disorders diagnosed at least two times, kappa coefficients were: major depressive disorder (kappa=1.00), dysthymic disorder (kappa=1.00), bipolar disorder (kappa=1.00), depressive disorder not otherwise specified (kappa=0.45), panic disorder (kappa=1.00), social phobia (kappa=0.87), obsessive-compulsive disorder (kappa=1.00), specific phobia (kappa=1.00), generalized anxiety disorder (kappa=0.64), and PTSD (kappa=1.00).
The PTSD section of the SCID begins with the question, “Sometimes things happen to people that are extremely upsetting or life-threatening—like a major disaster, very serious accident, combat, fire, being physically assaulted or raped, seeing another person killed or dead or badly hurt. Have any of these kinds of things happened to you?” Patients who reported more than one trauma were asked which trauma affected them the most, and they were asked about symptoms of PTSD related to the event they identified as most traumatic. Patients were not specifically asked about the presence or absence of each type of trauma mentioned in individual questions in the PTSD section of the SCID; rather, they were asked the SCID’s initial screening question and the traumatic events they reported were classified into 13 categories. PTSD was assigned as either the primary diagnosis or as an additional diagnosis. The DSM-IV convention for distinguishing between primary and additional diagnoses is based on the reason for presenting for treatment.
Results
Of the 1,130 patients seeking treatment, 99 women (8.8% of the patients) and 39 men (3.5% of the patients) received a diagnosis of current PTSD. Of these 138 patients (12.2% of all patients), most were Caucasian (N=117, 84.8%); their mean age was 35.48 years (SD=10.42). The majority of the 138 patients with current PTSD had completed high school or had some college education (N=116, 84.1%), and 43.5% were married or cohabiting (N=60). Among the patients seeking treatment, a significantly higher proportion of women than men received a diagnosis of PTSD (women: N=99 of 700, 14.1%; men: 39 of 430, 9.1%) (χ2=5.93, df=1, p<0.05, with Yates’s correction). No demographic differences between men and women with PTSD were found.
Overall, 137 participants with PTSD reported experiencing a variety of index traumatic events, including serious accidents (6.6%, N=9), nonsexual assaults (27.7%, N=38), sexual assaults (40.1%, N=55), military combat (2.2%, N=3), life-threatening illness (2.9%, N=4), witnessing a death or violent assault (10.2%, N=14), or some other traumatic experience (10.2%, N=14) (data missing for one woman with PTSD). Of the two most frequently reported types of trauma (i.e., sexual assault and nonsexual assault), sexual assault was significantly more likely to be reported by women than by men (N=46, 46.5%, compared with N=9, 23.1%) (χ2=5.45, df=1, p<0.05, with Yates’s correction).
Of the 138 patients with current PTSD, 37 (26.8%) had PTSD as their primary diagnosis. Only major depressive disorder was identified as a primary disorder more frequently (N=55, 39.9%) than PTSD. Of the remaining disorders identified as a primary disorder, bipolar disorder had the third highest frequency (N=13, 9.4%), after PTSD. There were no differences in the proportion of male and female patients that received a primary diagnosis of PTSD, major depressive disorder, or bipolar disorder.
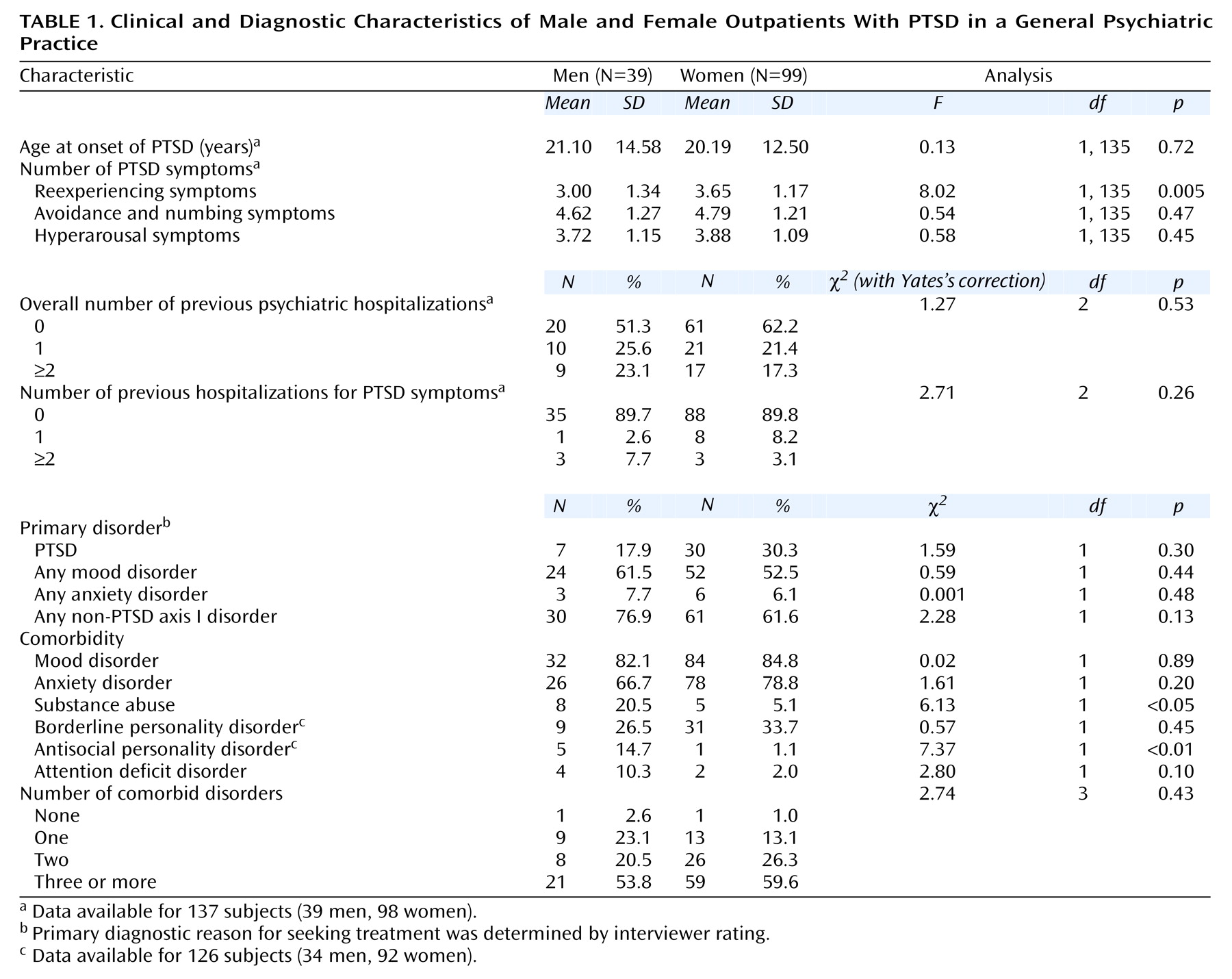
Among the range of clinical variables examined in this report, only one variable showed a significant difference between men and women with PTSD: in a multiple regression analysis that controlled for sexual assault, women were found to report a greater number of reexperiencing symptoms than men (mean=3.65, SD=1.17, compared with mean=3.00, SD=1.34) (F=5.32, df=2, 134, p=0.005). As for gender differences in the comorbidity profiles of patients with PTSD, men were significantly more likely than women to meet criteria for a substance abuse disorder and antisocial personality disorder (
Table 1). Although other specific current axis I disorders were examined for evidence of gender differences, this report found no other significant differences.
A power analysis using an alpha level of 0.05 showed that the size of the study group had acceptable power (80%) for at least medium effects to be detected, as defined by Cohen
(9), in each of the analyses in our report.
Discussion
This report is the first, to our knowledge, to systematically examine gender differences in patients with current PTSD and a broad range of trauma exposure. The present report found that female patients compared to male patients were more likely to meet criteria for PTSD and to report sexual trauma as their index trauma and that female patients with PTSD experienced a greater number of reexperiencing symptoms than male patients with PTSD. These findings are generally consistent with findings in community-based research that PTSD is twice as prevalent in women than in men
(1) and that women are more likely to experience sexual trauma than men
(1).
Other findings were that men with PTSD were significantly more likely than women with PTSD to meet criteria for a substance use disorder and antisocial personality disorder. These results are similar, in part, to the findings of the National Comorbidity Survey
(1), in which men with lifetime PTSD reported higher rates of substance use disorder and conduct disorder than women with lifetime PTSD.
The present report found no gender differences in the number of comorbid disorders or the presence of PTSD as the primary disorder in this group of outpatients with current PTSD. Studies with depressed patients have also found few differences between male and female patients in depressive symptoms
(10). Despite theoretical formulations about gender differences in response to trauma, including gender differences in brain morphology or in social interpretations of trauma
(11), empirical evidence from our report suggests that the manifestations of PTSD among male and female patients are more similar than different. Obviously, our results need to be replicated before definitive conclusions can be drawn.