Psychiatric comorbidity is defined as the presence, either simultaneously or in succession, of two or more specific disorders in an individual within a specified period
(1,
2). Comorbidity is substantial in the general population. The Epidemiologic Catchment Area study and the National Comorbidity Study, both in the United States, found that 54% and 56%, respectively, of respondents with a lifetime history of at least one DSM-III/DSM-III-R disorder also met criteria for some other mental disorder
(3,
4). The somewhat lower figure of 45% found in the Netherlands Mental Health Survey and Incidence Study
(5) is probably related to differences in the definition of samples and diagnostic categories used. In the National Comorbidity Study, more than half (59%) of all 12-month disorders occurred in the 14% of the population with a history of three or more disorders
(3). These subjects were more likely to be female, 15–24 years old, and residents of major metropolitan areas and to have lower income and educational attainment levels, compared with subjects without a history of three or more disorders.
Comorbidity has major consequences. In all three surveys
(3,
6,
7), subjects with comorbid disorders had higher service utilization rates than those with pure disorders. Comorbidity has also been linked to more severe symptoms
(8–
10), greater functional disability
(9,
11–13), and longer illness course
(3,
14). In primary health care, comorbidity increases the chances that mental disorders will be recognized and increases the likelihood of receiving treatment
(15).
In view of the prevalence and consequences of psychiatric comorbidity, it is important to promote its prevention and cure. To meet that goal, information about the distribution of psychiatric comorbidity in the general population is necessary. Since much research on determinants of mental disorders has not distinguished between pure and comorbid conditions
(3,
16)—although mental disorders could have different determinants in their pure and comorbid forms—little such information is available. Using data from the National Comorbidity Study, Blazer et al.
(17) found clear differences between the risk factor profiles of pure major depression and of major depression co-occurring with other disorders. The pure disorder was associated with female gender, being separated, widowed or divorced, and being a homemaker; the comorbid condition showed additional associations with lower educational level and lower age.
In the present study, which is based on data from the Netherlands Mental Health Survey and Incidence Study, we first assessed the risk factor profiles in the general population for 12-month pure mood, anxiety, and substance use disorders and for comorbid conditions. We limited the investigation to the main DSM groupings. Since long-term vulnerability factors can potentially be associated with comorbidity
(18), we included parental psychiatric history and childhood traumas as potential predictors along with several sociodemographic variables. We expected to encounter different patterns of risk factors for pure and comorbid disorders and expected that parental psychiatric history and childhood traumas would be more strongly associated with comorbid conditions than with pure disorders. Next, among subjects with a diagnosis of a mood, anxiety, or substance use disorder, we investigated which factors determine whether the disorder was pure or comorbid. Because patterns of comorbidity can differ dramatically by gender
(19,
20), we tested for interaction with gender to identify differences between the risk profiles of men and women.
Method
Sample
The Netherlands Mental Health Survey and Incidence Study was based on a multistage, stratified, random sampling procedure
(16,
21). First, a sample of 90 Dutch municipalities, stratified on the basis of urbanicity and with adequate distribution over the 12 Dutch provinces, was drawn. The second step was to draw a sample of private households from post office registers. The number of households selected in each municipality was determined by the size of its population. The third step was to choose which individuals to interview. The selected households were sent a letter of introduction signed by the national minister of public health asking them to take part. Shortly thereafter, they were contacted by telephone by the interviewers. Households with unlisted numbers or no telephone (18%) were visited in person. In each household, the member with the most recent birthday was selected, on the condition that he or she was between 18 and 64 years old and sufficiently fluent in Dutch to be interviewed. Persons who were not immediately available (because of travel, hospitalization, imprisonment) were contacted later in the year. To establish contact, the interviewers made a minimum of 10 phone calls or visits to a given address at different times of the day and week, if necessary. In the initial data collection phase, from February through December 1996, a total of 7,076 persons were interviewed. The response rate was 69.7%. Of the nonresponders, 22.1% could not be contacted and 77.9% refused to participate
(16). The participants in the survey well reflected the Dutch population in gender, civil status, and urbanicity
(21). Only the 18–24-year age group was underrepresented.
Composite International Diagnostic Interview
The diagnoses of psychiatric disorders were based on DSM-III-R axis I. The Composite International Diagnostic Interview, version 1.1 (computerized version)
(22) was used to determine the diagnoses. The Composite International Diagnostic Interview is a structured interview developed by the World Health Organization (WHO)
(23,
24) and based on the National Institute of Mental Health Diagnostic Interview Schedule and the Present State Examination. It was designed for use by trained interviewers who are not clinicians. Version 1.1 of the Composite International Diagnostic Interview contains two diagnostic programs to compute diagnoses according to the criteria and definitions of either DSM-III-R or ICD-10. The Composite International Diagnostic Interview is used worldwide, and WHO field trials have documented acceptable reliability and validity
(25–
29). The following DSM-III-R diagnoses were recorded in the Netherlands Mental Health Survey and Incidence Study: mood disorders (depression, dysthymia, bipolar disorder); anxiety disorders (panic disorder, agoraphobia, simple phobia, social phobia, generalized anxiety disorder, obsessive-compulsive disorder); psychoactive substance use disorders (alcohol or drug abuse and dependence, including abuse of sedatives, hypnotics, and anxiolytics); eating disorders; and schizophrenia and other nonaffective psychotic disorders.
Dependent Variables
We distinguished two types of dependent variables. The first was the presence of a mood, anxiety, or substance use disorder, either pure or comorbid, at any point within the 12 months preceding the interview (0=absence; 1=presence) in the entire sample. A pure mood disorder was defined as any mood disorder present in a specified 12-month period in a subject who did not exhibit any anxiety disorder, substance use disorder, eating disorder, or schizophrenia within the same period. A comorbid mood disorder was defined as a mood disorder present in the 12-month period in a subject who also had an anxiety disorder (anxiety-comorbid mood disorder), a substance use disorder (substance use-comorbid mood disorder), or both (the most comorbid condition) at some time in the same period. We determined the presence of pure anxiety disorder and pure substance use disorder in a similar fashion. In addition to the comorbid conditions just mentioned, substance use-comorbid anxiety disorder could also be distinguished. We did not address comorbidity between separate disorders within the same category.
The second type of dependent variable was whether subjects with a diagnosis of mood, anxiety, or substance use disorder had a pure (score=0) or a comorbid (score=1) disorder.
Independent Variables
The potential predictors used in analyzing both types of dependent variables included current sociodemographic variables and chronic somatic disorders. Since long-term vulnerability could be associated with the presence of comorbidity, we also included the historical factors of parental psychiatric history and childhood traumas and adversities in the analyses.
Sociodemographic variables
The sociodemographic variables were gender, age, educational attainment, urbanicity (municipalities with fewer than 500 addresses per square kilometer were considered rural, and larger municipalities were considered urban), cohabitation status (living with a partner or not, irrespective of children), and employment status (paid employment or not).
Chronic somatic disorders
From a list of 31 chronic somatic disorders, subjects self-reported the presence of one or more conditions being treated or monitored by a physician in the 12 months before baseline. Examples included asthma, emphysema, arthritis, rheumatism, heart disease, heart attack, peptic ulcer, and diabetes.
Parental psychiatric history
Respondents were asked whether one or both biological parents had ever been treated by a psychiatrist, hospitalized in a mental institution, or exhibited one of the following problems: depression, delusions or hallucinations, anxiety disorders or phobias, alcohol abuse, or suicide.
Childhood traumas and adversities
Respondents were asked whether they had experienced before age 16 emotional neglect, psychological abuse or physical abuse on two or more occasions, or sexual abuse on one or more occasions. Respondents were prompted to report these adversities with questions such as: “Before you reached the age of 16, were you ever psychologically abused? —physically abused? —sexually abused?” Psychological abuse was described to respondents as follows: “You were cursed, unjustly punished, your brothers and sisters were favored—but no bodily harm was done.” Physical abuse was explained as follows: “You were kicked, hit with or without an object, or you were physically maltreated in any other way.” Sexual abuse was defined as follows: “You were sexually stimulated against your will, or you were forced to sexually stimulate the perpetrator against your will.”
Statistical Analysis
We first investigated the determinants of 12-month pure and comorbid mood, anxiety, and substance use disorders by means of multiple logistic regression analysis among all respondents. We then performed a similar analysis with data from those subjects with a diagnosis of a mood, anxiety, or substance use disorder to identify the factors that were associated with whether the disorder was pure or comorbid. To test for linear trends, ordinal determinants (education, age) were modeled as continuous variables.
Further analyses were performed to detect interactions between gender and the other variables. This second series of multivariate models included the main effects, the interaction terms, and all other potential predictors.
All separate disorders were diagnosed without applying DSM-III-R hierarchy rules. Because we focused on associations, we made no use of sample weighting to generalize to the general population, except in estimating prevalence rates of the disorders. In the latter case, we used poststratification to weight the data to make them representative of the general Dutch population in terms of gender, age, marital status, and urbanicity.
Results
Sample Characteristics
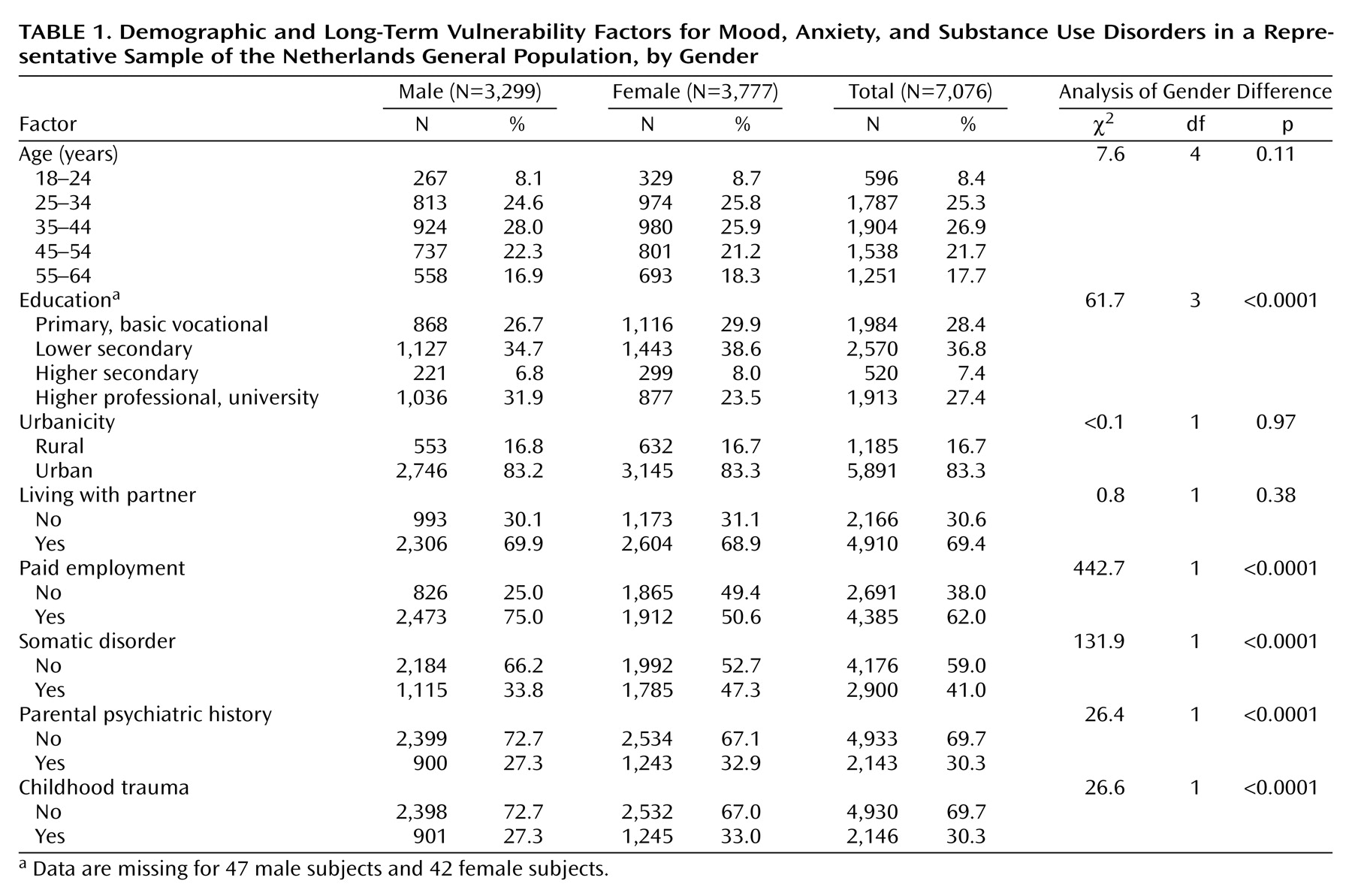
Table 1 shows the demographic and long-term vulnerability characteristics of the subjects. Compared with men, women had less education, were less likely to have paid employment, and were more likely to report somatic disorders, parental psychiatric history, and childhood trauma.
Prevalence Rates
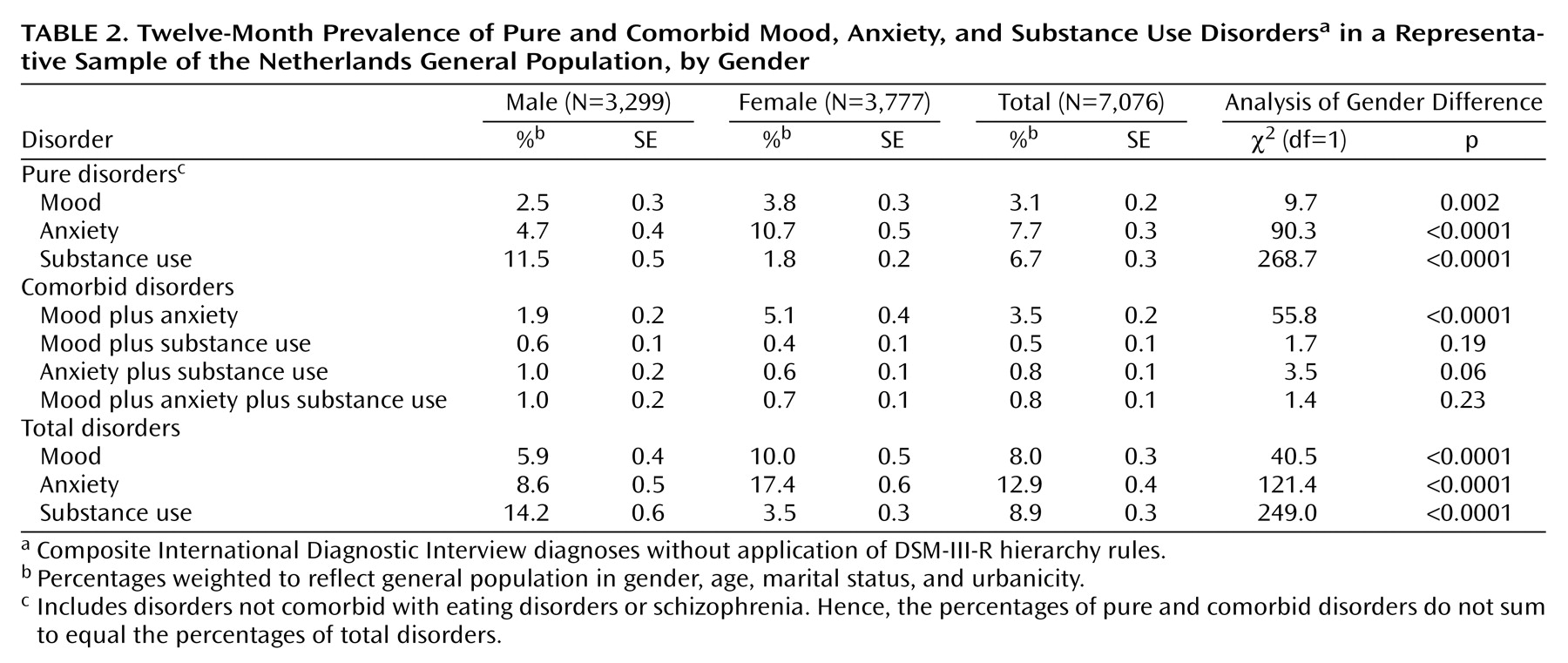
Anxiety-comorbid mood disorder was the most prevalent comorbid condition (
Table 2). This comorbid condition was even more prevalent than pure mood disorder. Pure mood disorder and pure anxiety disorder were more prevalent in women, and pure substance use disorder in men. Among the comorbid conditions, the only significant gender difference was for anxiety-comorbid mood disorder, which was more common among women.
A total of 60.5% of the subjects with a mood disorder also had at least one other comorbid disorder, usually an anxiety disorder (54.3%) (not in table). A relatively small percentage of the subjects with a mood disorder had a comorbid substance use disorder (16.7%).
Anxiety disorder was less likely to be comorbid with other disorders (40.7%). The proportion of subjects with an anxiety disorder who had a comorbid mood disorder (33.4%) was smaller than the proportion of subjects with a mood disorder who had an anxiety disorder (54.3%). Only a small minority of subjects with an anxiety disorder had a comorbid substance use disorder (13.0%).
Comorbidity was not common among subjects with a substance use disorder. Only 24.6% of subjects with a substance use disorder had a comorbid disorder. Only small minorities of subjects with a substance use disorder met criteria for a mood disorder (14.9%) or an anxiety disorder (18.9%).
Predictors of Prevalence
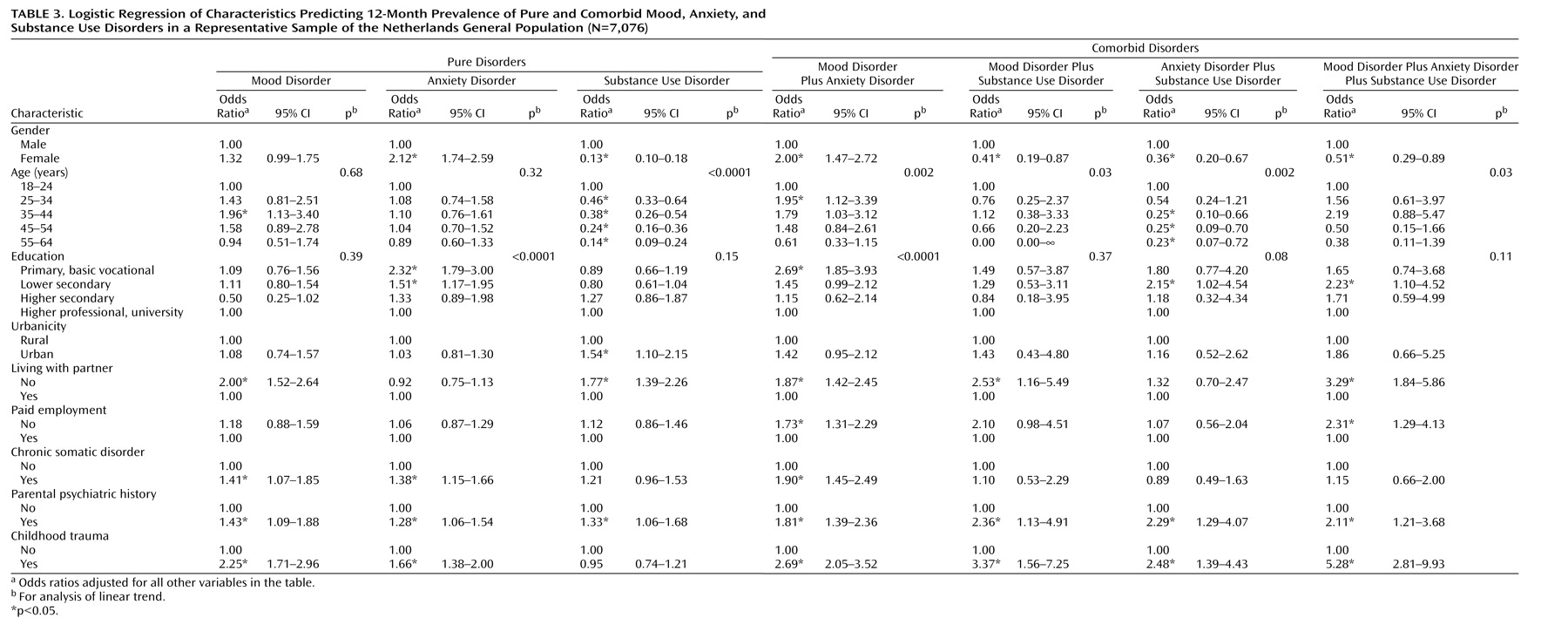
Table 3 shows the determinants of the 12-month prevalence of pure and comorbid disorders. The patterns of odds ratios for comorbid disorders differed considerably from those for pure disorders. Anxiety-comorbid mood disorder was significantly linked to all but one of the determinants investigated, but pure mood disorder and pure anxiety disorder were linked to just about half of the determinants. The other comorbid conditions showed fewer associations than anxiety-comorbid mood disorder.
Gender was associated with all pure and comorbid conditions, although its relationship with pure mood disorders was not significant. Women were more likely than men to have a pure anxiety disorder and anxiety-comorbid mood disorder, and men were more likely to have a substance use disorder, either pure or in one of the three comorbid conditions. The gender difference was largest for pure substance use disorder. The risk for pure substance use disorder and for all four comorbid conditions was reduced with increasing age. With rising educational attainment levels, there was a diminishing risk of pure anxiety disorder and anxiety-comorbid mood disorder. Urban residency was a significant predictor of pure substance use disorder only. Living without a steady partner was associated with all disorders except pure anxiety disorder and substance use-comorbid anxiety disorder; and the association was highest for the subjects with comorbid mood, anxiety, and substance use disorders. People without paid employment were about twice as likely as employed people to have anxiety-comorbid mood disorder, either with or without a co-occurring substance use disorder.
Subjects with a somatic condition had a somewhat greater chance of exhibiting pure mood disorder, pure anxiety disorder, and anxiety-comorbid mood disorder. Having a parent with a psychiatric history increased the probability of all conditions. The same was true of childhood trauma, with the exception of pure substance use disorder. The magnitude of the significant odds ratio for childhood trauma ranged from 1.66 to 5.28; it was higher for comorbid than for pure conditions, and highest for the most comorbid condition (comorbid mood, anxiety, and substance use disorders).
In a second series of models, we investigated interactions between gender and the other variables (not in table). The gender-by-education interaction term was significant for pure substance use disorder (odds ratio=1.33, 95% confidence interval [CI]=1.04–1.70; p=0.74 for male subjects, p=0.01 for female subjects) and for anxiety-comorbid mood disorder (odds ratio=0.65, 95% CI=0.50–0.85; p=0.70 for male subjects, p<0.0001 for female subjects). Only women had an increased risk of the former disorder with higher educational level, and only women had a reduced risk of the latter condition with higher educational level. Not cohabiting with a steady partner increased the likelihood of pure mood disorder among female subjects only (odds ratio=1.90, 95% CI=1.08–3.34).
Predictors of Comorbid Versus Pure Disorders
Among subjects who exhibited some disorder, what factors predicted whether it would be a pure or comorbid disorder?
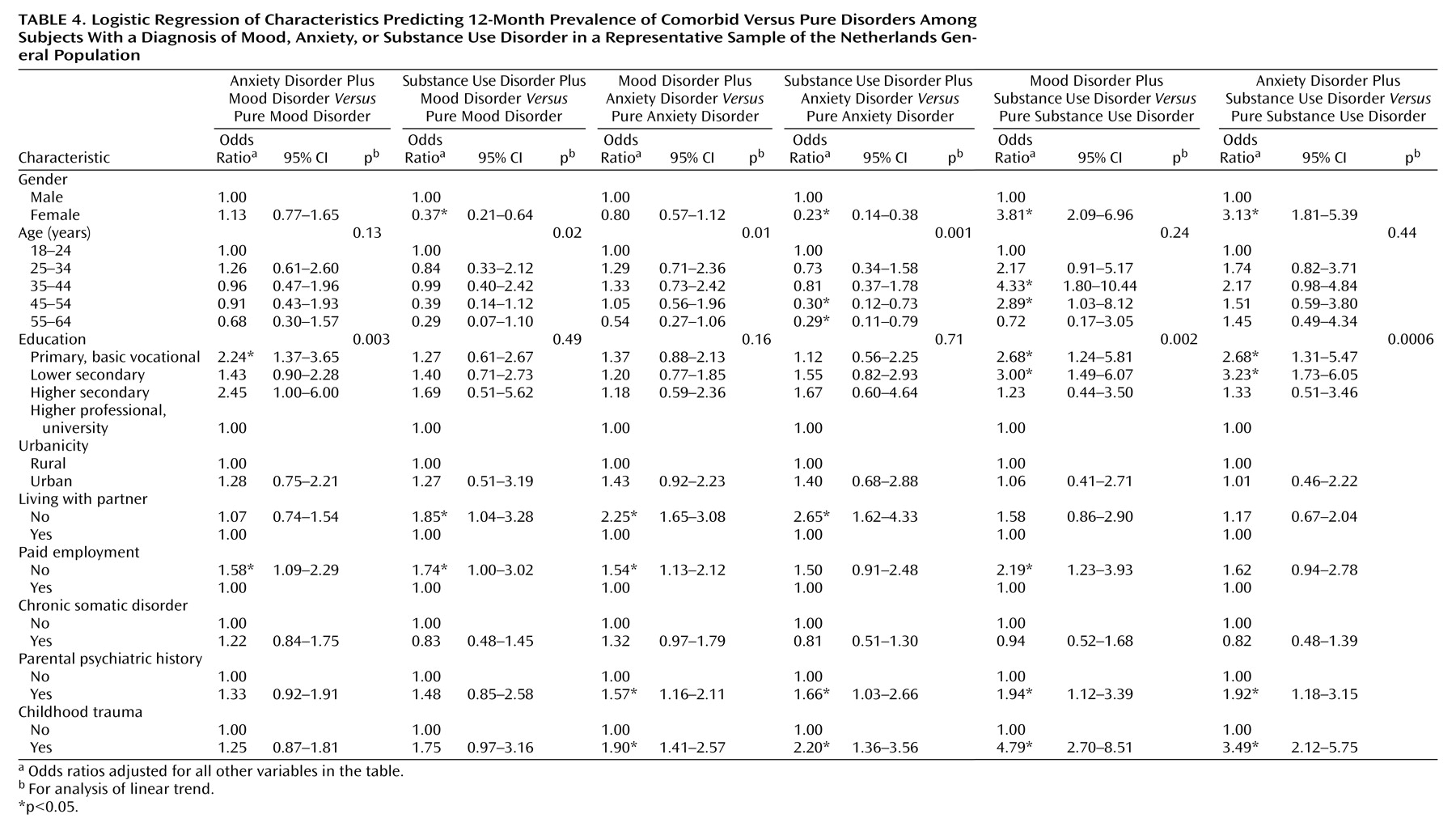
Table 4 shows, for subjects with each type of disorder, the odds ratios indicating the likelihood that the disorder is comorbid and not pure. To limit the number of comparisons, we incorporated the most comorbid condition into the other comorbidity categories. Mood disorder was more likely to be comorbid with anxiety disorder than pure in less educated and unemployed subjects. For unemployed subjects, mood disorder was also more likely to be substance use-comorbid than pure. The same applied to men, younger people, and subjects who were not living with a partner.
Anxiety disorder was more likely to be mood-comorbid than pure in subjects who were younger, were not living with a partner, were unemployed, had a parent with a psychiatric history, and had experienced childhood traumas. The same factors, except employment status, predicted that the anxiety disorder was substance use-comorbid rather than pure. Anxiety disorder in men was also more likely to be substance use-comorbid than pure.
Substance use disorder was more likely to be mood-comorbid than pure in women, less educated subjects, unemployed subjects, those with parental psychiatric history, and those with a childhood trauma. The same variables, except employment status, predicted that the substance use disorder was anxiety-comorbid rather than pure. Childhood trauma was an especially strong predictor of comorbidity in substance use disorder.
The following interaction terms between gender and the other variables were significant (not in table). Gender-by-education was significant for anxiety-comorbid versus pure mood disorder (odds ratio=0.63, 95% CI=0.45–0.88; p=0.90 for male subjects, p=0.001 for female subjects). Women with a mood disorder showed a diminishing risk of comorbidity with higher educational level. Gender-by-employment status was significant for mood-comorbid versus pure anxiety disorder (odds ratio=0.30, 95% CI=0.15–0.61). Unemployment was associated with comorbidity only in male subjects with an anxiety disorder. Gender-by-childhood trauma was significant for mood-comorbid versus pure substance use disorder (odds ratio=0.28, 95% CI=0.08–0.90). Although the overall odds ratio relating this type of comorbidity to childhood trauma was high (odds ratio=4.79) (
Table 4), the association was significant for male subjects only.
Discussion
In interpreting the results of this study, one should be aware of its limitations. Diagnoses were made by using fully structured diagnostic interviews administered by lay interviewers. Although diagnoses made with the Composite International Diagnostic Interview have shown acceptable reliability and validity, they do not match the accuracy of diagnoses by clinicians. For example, self-reported Composite International Diagnostic Interview substance use disorders might be limited. Second, the data were based on retrospective recall. Although this approach can be a source of considerable recall bias in recording lifetime disorders
(17,
30), recall bias is less probable for the 12-month disorders dealt with in this study. A third limitation is that our predictors of disorders were recorded at baseline, whereas the onset of the disorders could have occurred long before that. Thus, when variables such as employment or cohabitation status are found to be linked to psychopathology, the causality is not clear: a respondent’s living or working situation could have been part of the cause of the disorder, but it cannot be ruled out that this situation partly resulted from the disorder itself. A fourth limitation could lie in the fact that people currently experiencing a disorder may attach more importance to past life events in their attempts to understand its origins
(31) and thus would be more likely to report experiences such as childhood trauma and parental psychiatric history. However, we believe that the high odds ratios found for childhood trauma cannot be attributed exclusively to such increased awareness. A fifth limitation is that we do not know whether nonresponders differ from responders in having a pure or comorbid disorder.
Consistent with other studies, we found mood disorders to be highly comorbid with other mental disorders, most often with anxiety
(18,
19,
32). In our study, only 40% of the 12-month mood disorders were pure, but anxiety disorder (59%) and substance use disorder (75%) were more often pure. Anxiety-comorbid mood disorder was the most prevalent comorbid condition among both genders but was more common in women.
The patterns of odds ratios for pure and comorbid disorders were distinctly different. Anxiety-comorbid mood disorder proved to be significantly associated with all but one of the investigated determinants, whereas pure mood disorder and pure anxiety disorder showed only four or five such associations. All risk factors associated with pure mood disorder (noncohabitation, somatic comorbidity, parental psychiatric history, and childhood trauma) were also linked to anxiety-comorbid mood disorder, but the comorbid condition was further linked to female gender, younger age, lower educational attainment, and unemployment. Moreover, the odds ratios for parental psychiatric history and childhood trauma were higher for anxiety-comorbid mood disorder than for pure mood disorder and pure anxiety disorder. The distinctive risk factor profile we found for those with mood disorder in conjunction with anxiety disorder may mean that they represent people with a more severe condition. The further combination of these two types of disorder with substance use disorder was similarly associated with a large number of the investigated variables. The high association with childhood trauma is noteworthy.
Few studies have addressed the differential risk factor profiles between pure and comorbid disorders. The National Comorbidity Study compared the risk factors for 30-day pure major depression and major depression comorbid with any other disorder
(17). Our analyses generated reasonably comparable risk factor profiles for 12-month pure and comorbid mood disorders, with comorbidity differentiated by diagnostic grouping. Three-quarters (74.3%) of the mood disorder cases in the Netherlands Mental Health Survey and Incidence Study involved major depression. With these differences in mind, we compared the results of these studies (30-day versus 12-month prevalences). In the Netherlands Mental Health Survey and Incidence Study, gender was associated with all comorbid mood conditions—female subjects were more likely to have an anxiety-comorbid mood disorder, and male subjects were more likely to have the other comorbid mood conditions—and just not with pure mood disorder. In the National Comorbidity Study, gender was associated with both pure and comorbid major depression. Individuals in the National Comorbidity Study sample were younger (ages 15–54) than those in the Netherlands study (ages 18–64). Neither study found a diminishing risk of pure major depression or mood disorders with increasing age, but risk diminished with age for comorbid major depression in the National Comorbidity Study and for all comorbid mood conditions in the Netherlands study. Neither study found a reduced risk for the pure condition with higher levels of education, but with higher educational levels risk was significantly reduced for comorbid major depression in the National Comorbidity Study and anxiety-comorbid mood disorder in the Netherlands study. Urbanicity showed no association with risk in either study. In the Netherlands study, those not living with a steady partner had a greater probability of both pure mood disorder and all comorbid mood conditions than those who did. In the National Comorbidity Study, only subjects living with someone other than a spouse or parent were found to have a greater chance of both pure and comorbid major depression, compared to those living with a spouse. In both studies, unemployment was not associated with pure conditions, but it was associated with two of the mood-comorbid conditions in the Netherlands study and with comorbid major depression in the National Comorbidity Study.
The importance of distinguishing between pure and comorbid conditions when investigating determinants of mental disorders is underlined by the following findings. Although we did not present these data here, we found distinct differences between the risk factor profiles for 12-month pure mood disorder and overall mood disorders (both pure and comorbid conditions), but the risk factor profile of comorbid mood disorder was very similar to that for overall mood disorders. The risk factors of gender, age, education, urbanicity, and employment, which were associated with overall mood disorders
(16), also applied to comorbid, but not to pure, mood disorder.
Beekman et al.
(18) reported that when major depression is accompanied by anxiety disorder in elderly subjects, the comorbid disorders have a stronger association with long-term vulnerability factors than do the pure disorders. In our sample, which did not include elderly people, we similarly found that the odds ratios for parental history and childhood trauma were higher for all comorbid conditions than for the pure disorders, as we had hypothesized. It is worth noting that we found no association between childhood trauma and pure substance use disorder. One explanation might be that the Composite International Diagnostic Interview diagnosis of alcohol abuse, which comprises the bulk of substance use disorders, does not necessarily reflect a form of psychopathology
(31). Young male subjects frequently receive a diagnosis of alcohol abuse
(16), and it is the only disorder that is not widely associated with other psychiatric disorders
(5). In the general population of young adults, a Composite International Diagnostic Interview diagnosis of substance use disorder probably does not reflect psychopathology but rather behavior specific to a particular phase of life in which many people use considerable amounts of alcohol.
What implications do our findings have for prevention and clinical practice? Since mental disorders often have certain risk factors in common, similar primary interventions may be effective against different disorders
(33–
35). For example, childhood trauma, which was found in 30% of the population, was a common risk factor for nearly all disorders investigated in our study. Thus, prevention of childhood traumas and effective aid to childhood trauma victims might help to forestall the later onset of a range of pure and comorbid psychiatric disorders. Different types of interventions will be needed for disorders whose risk factors are not communal with those of other disorders. For example, special preventive interventions for substance use disorder could especially target young men. Interventions for mood disorder could focus on 25–54-year-old women, with special attention to comorbidity because mood disorder is more often comorbid than pure among women. The most effective approach is probably a mix of generalized and focused interventions. Comorbidity can have major consequences in terms of functional disabilities for individuals
(11), but it can also seriously affect their social environment and the broader society. Therefore, Kessler and Price
(36) emphasized the importance of primary prevention of secondary disorders and have proposed preventive trials in groups of people with a history of a primary disorder, who are thus at risk for comorbid disorders. Early intervention before the onset of comorbidity is a strategy that could reduce the complexity of treatment. In primary care and treatment settings, clinicians should be aware that patients could have a second disorder in addition to the primary disorder that is the focus of treatment or that a second disorder could surface at some time in the future.