Schizophrenia is marked by poor social role performance, a complex phenomenon that is influenced by a number of affective, motivational, and environmental factors. One of the critical ingredients is
social skill, a behavioral construct that reflects the smooth application of a repertoire of specific verbal and nonverbal abilities and cognitive capacities (i.e., social cognition, social problem solving). Social skill, as measured by role play (simulated conversations), has been reliably shown to predict community functioning
(1). Conversely, social functioning is only weakly related to symptomatic improvements and is not substantially responsive to traditional antipsychotic medications
(2).
The impact of new-generation medications on social skill and social role functioning has not yet been determined. There is good evidence that neurocognitive deficits are strongly linked to functional outcomes such as social competence and the capacity for work
(3,
4), and there is evidence that newer antipsychotic medications may have benefits on some aspects of cognitive functioning
(5). While the effects of the newer agents on neurocognition have often been modest, the consistency of these findings suggests that new-generation medications might improve social outcomes as well. We examined the impact of clozapine and risperidone on social skill as part of a multisite trial (unpublished 2002 study of N.R. Schooler et al.). Problem-solving capacity and cognitive flexibility, as measured by the Wisconsin Card Sorting Test
(6), has been related to social competence
(7,
8), and there have been mixed results for the effects of clozapine and risperidone on these aspects of executive functioning. Hence, we also assessed patients with the Wisconsin Card Sorting Test.
Method
The parent study was a 6-month, double-blind trial comparing clozapine (target dose: 500 mg/day) and risperidone (target dose: 6 mg/day). Subjects met criteria for DSM-IV schizophrenia or schizoaffective disorder as determined by a diagnostic checklist based on a structured interview. They were representative of community samples and included those requiring adjunctive medications or who had a history of poor compliance and substance abuse. Approximately 23% lived with parents, 23% lived independently, and 54% lived in supervised housing. Inclusion criteria were at least one previous trial of a conventional antipsychotic at a dose equivalent to 600 mg/day of chlorpromazine, a second trial at a dose equivalent to 250–500 mg/day of chlorpromazine, and a rating of at least moderate on one of the BPRS psychotic items or on one of subscales from the Scale for the Assessment of Negative Symptoms (SANS). After complete description of the study to the subjects, written informed consent was obtained.
Treatment was continued for up to 29 weeks, and doses could be increased to 800 mg/day for clozapine and 16 mg/day for risperidone after 5 weeks. Subjects treated with clozapine were significantly less likely to discontinue treatment for lack of efficacy (15%) than were those treated with risperidone (38%) and showed significantly more improvement globally and in asociality. However, there was no statistically significant difference in proportions of subjects meeting an a priori criterion of psychosis symptom improvement (risperidone: 57%; clozapine: 71%).
Social skill was evaluated with the Maryland Assessment of Social Competence
(1,
9). This structured behavioral assessment measures the ability to resolve interpersonal problems through conversation. It employs a series of 3-minute simulated conversations with a live confederate who portrays the protagonist in the situation (e.g., a landlord, boss). It is an abbreviated version of an empirically developed procedure that has proven to be reliable and to have good discriminant validity
(1,
9). In order to control for multiple administrations, we employed three parallel sets of four scenarios. A randomization schedule ensured that each set appeared equally at each assessment point at each site. Results were equivalent across sets and they were collapsed for subsequent analyses.
Patient responses were videotaped for subsequent coding by blinded raters on five specific dimensions of verbal behavior (clarity, focus, negotiation, persistence, and overall conversation) and two nonverbal dimensions (fluency, affect). Intraclass correlations (ICC) indicated good agreement between primary and reliability raters on all categories (ICC mean=0.74, range=0.56–0.88). Ratings were collapsed into verbal and nonverbal domains for data analysis.
Cognition was evaluated by using the Wisconsin Card Sorting Test
(6), a widely used measure of executive functioning that assesses problem solving, ability to shift set, and working memory. A computerized, 128-card version was administered at each assessment.
Results
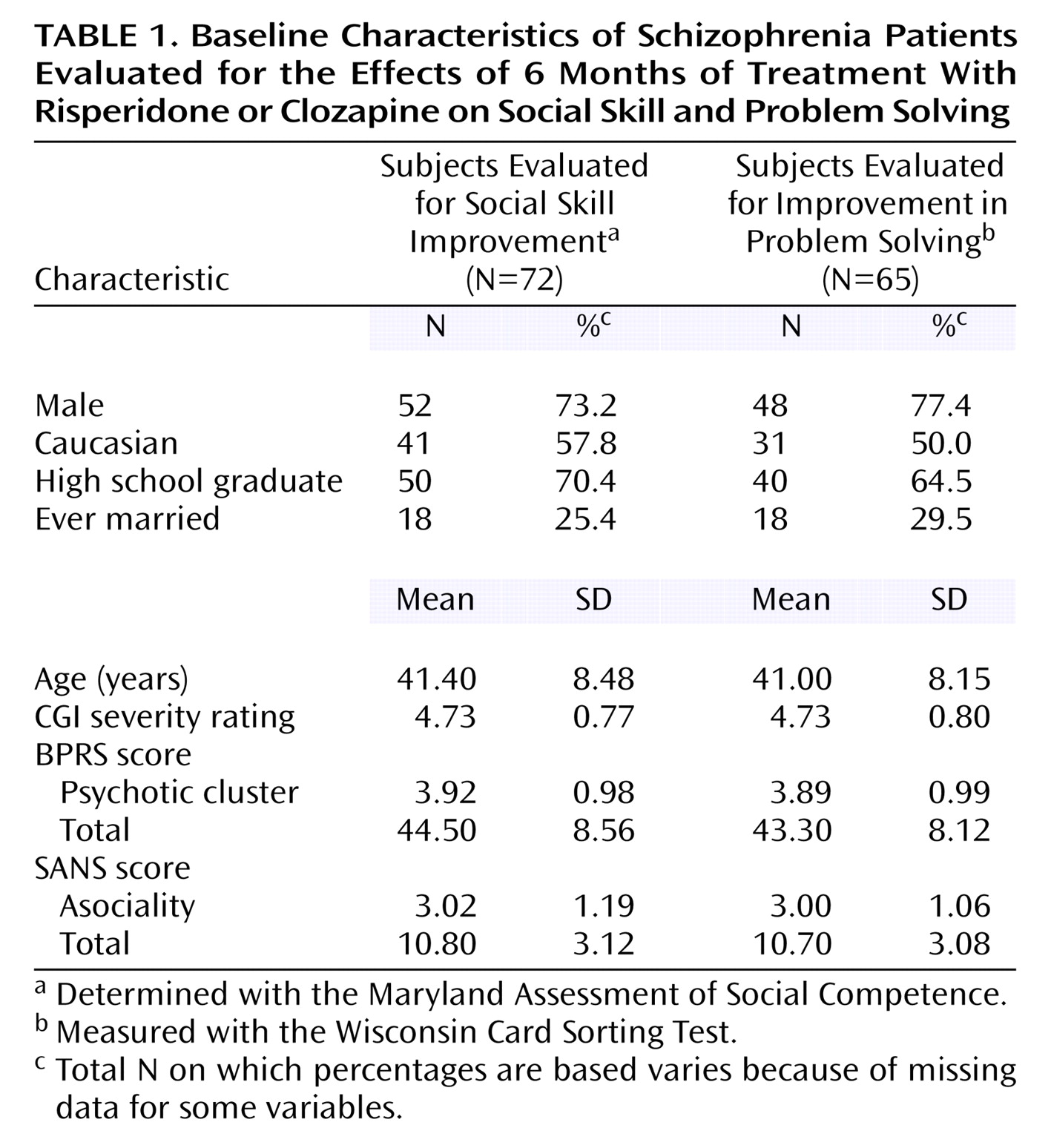
A total of 107 subjects were recruited for the parent trial, of whom 72 were assessed at baseline with the Maryland Assessment of Social Competence, and 65 were assessed with the Wisconsin Card Sorting Test. Demographic data for the two groups are presented in
Table 1. Missing data resulted from scheduling problems (different raters administered the Maryland Assessment of Social Competence, Wisconsin Card Sorting Test, and symptom ratings) or patients being too impaired to complete assessments. Overall, the sample was representative of the full study sample. Subjects completing the Maryland Assessment of Social Competence had significantly lower Clinical Global Impression (CGI) severity ratings and lower scores on the SANS affective and SANS overall scales than subjects who were not tested on this instrument; there were no other differences in demographic or symptom variables. Subjects given the Wisconsin Card Sorting Test had significantly less education, lower CGI severity ratings, and lower SANS alogia scores than did subjects who were not tested.
The Maryland Assessment of Social Competence, Wisconsin Card Sorting Test, and symptom ratings were conducted again at weeks 17 and 29. Sample sizes at those time points were 44 and 38, respectively, for the Maryland Assessment of Social Competence, 28 and 22 for the Wisconsin Card Sorting Test, and 60 and 55 for symptom ratings. Almost all subjects lost to the two follow-up assessments were removed from the parent study because of lack of efficacy (36%), subject discontinuation or refusal of treatment (32%), or adverse reactions (17%). Of those subjects who remained in the trial (e.g., completed symptom ratings), there were no significant differences on any demographic or symptom measure between subjects who completed the Maryland Assessment of Social Competence and Wisconsin Card Sorting Test and those who did not.
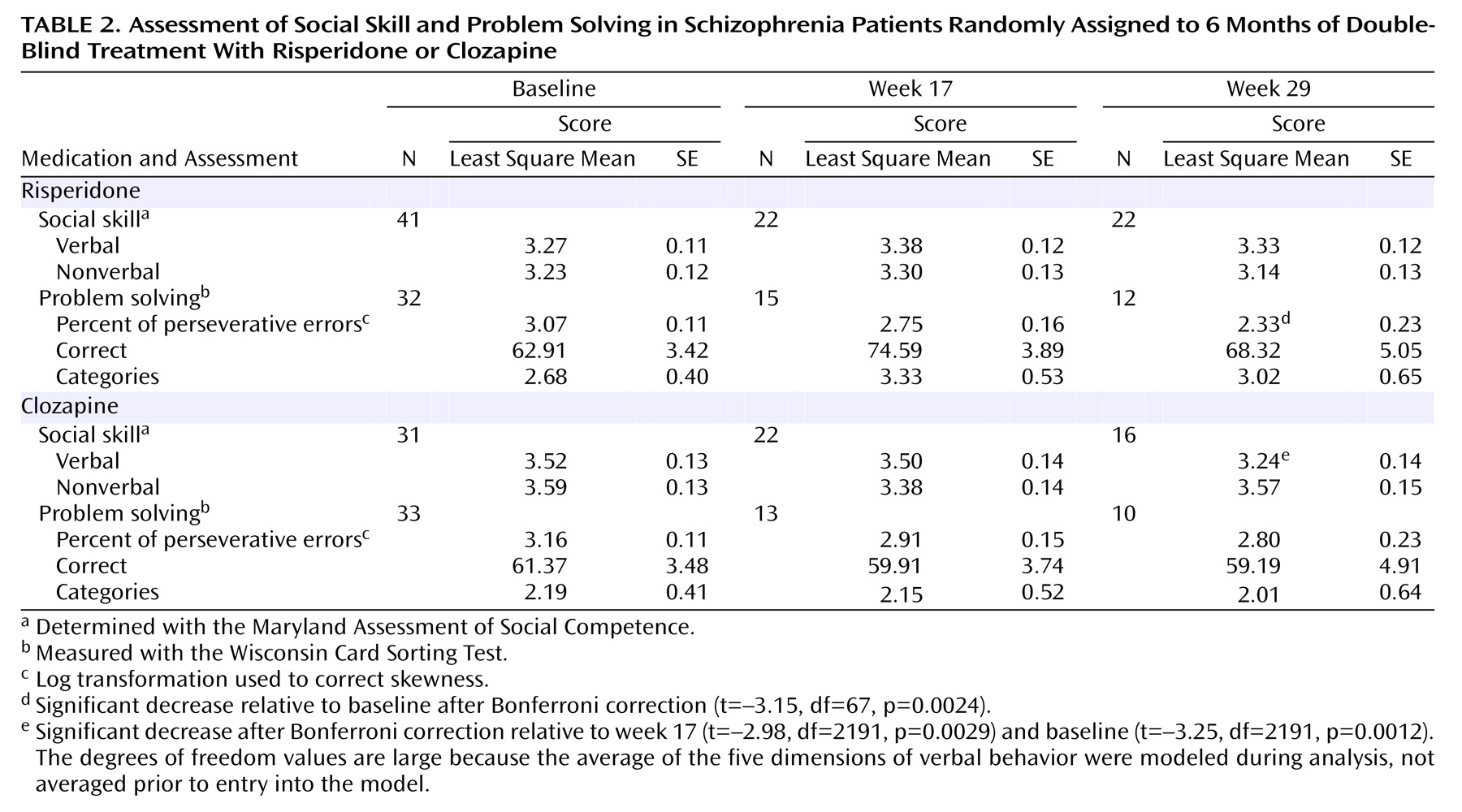
Each Maryland Assessment of Social Competence and Wisconsin Card Sorting Test outcome variable was analyzed with a separate mixed-effects regression model, and pairwise comparisons across the three assessment points were tested for significance. Bonferroni corrections were applied (separately) to the Maryland Assessment of Social Competence and Wisconsin Card Sorting Test analyses to control for multiple tests, and the criterion for significance was set at 0.004 and 0.0028, respectively. The results are displayed in
Table 2. There was no significant change in social skill for patients given risperidone, and there was a small but significant decrease in verbal skill for patients given clozapine by week 29. The group-by-time interactions were not significant. There was a small decrease in percent of perseverative errors for the risperidone group by week 29, but there were no other statistically significant changes in Wisconsin Card Sorting Test performance for either drug. The data in
Table 2 reflect all available scores at each time point. It is possible that a subset of patients showed consistent improvement even though the sample as a whole did not. That was not the case. Only four (of 27) subjects had meaningful improvements (greater than 0.5 standard deviations) on both verbal and nonverbal scores on the Maryland Assessment of Social Competence at week 17, and six had such improvements by week 29. The comparable numbers for improvement across all three Wisconsin Card Sorting Test variables were two at week 17 and one at week 29. In contrast, 22 of the 27 subjects with Maryland Assessment of Social Competence data had decreases of 0.5 standard deviations or more in CGI scores, and 20 had comparable decreases in BPRS psychotic cluster at both weeks 17 and 29.
Given the small and decreasing samples available at weeks 17 and 29, one could question whether some of the small differences would have reached significance if the trial had greater power. The answer to this question cannot be determined with certainty. However, effect sizes for the Maryland Assessment of Social Competence and Wisconsin Card Sorting Test from baseline to week 17 (among those assessed at both time points) were generally very modest. For example, effect sizes (increases) for verbal behavior were 0.33 (95% confidence interval [CI]=0.01 to 0.79), and –0.037 (95% CI=–0.47 to 0.30), respectively, for the risperidone and clozapine groups. This is in sharp contrast to the effect sizes (reductions) for symptom variables. For example, effect sizes for CGI severity were –1.42 (95% CI=–1.93 to –0.99) and –1.48 (95% CI=–2.11 to –0.99), respectively.
Observed effect sizes for the Wisconsin Card Sorting Test were all negative for the clozapine group, but the effect sizes in the risperidone group were 0.30 and 1.25 for categories and correct responses, respectively. A larger sample may or may not have resulted in statistically significant effects. Nevertheless, these effects at week 17 reflect changes of only 11.68 correct responses (62.91 to 74.59) and 0.65 categories (2.68 to 3.33), neither of which are clinically meaningful. Moreover, even these modest improvements were attenuated by week 29.
Another question is raised by the fact that some of the most severely ill subjects could not be assessed: would there have been larger effects if the most highly symptomatic subjects were included? Correlations between BPRS psychotic cluster at baseline and change in Maryland Assessment of Social Competence and Wisconsin Card Sorting Test scores for subjects who were assessed ranged from –0.44 (Wisconsin Card Sorting Test categories) to 0.24, suggesting that within our assessed sample, highly psychotic patients did not change more than those with less severe illness. Similarly, there were no significant correlations between SANS asociality and change on either the Maryland Assessment of Social Competence or the Wisconsin Card Sorting Test.
Discussion
Clozapine and risperidone both had significant effects on symptoms, but neither had an appreciable impact on either social skill or problem-solving ability. These findings are consistent with a prior study we conducted comparing clozapine and haloperidol
(10) and underscore the independence of social role performance from symptoms. There was a significant advantage for clozapine in terms of improvement on the SANS asociality scale, but this interview rating does not reflect the quality of social performance or the ability to deal with social problems, key issues for effective role functioning that are reliably assessed by the Maryland Assessment of Social Competence. The power for this trial was limited, given the small sample size and attrition across assessments. Hence, the generalizability of the findings is uncertain, and replication is warranted. This is especially true for risperidone, which did result in medium to large effects on some variables. However, the effects were all small in an absolute sense, and would not have been clinically significant even if they had reached statistical significance with a larger sample. In contrast, McGurk et al.
(11) reported that risperidone produced large effects on spatial working memory in the same sample, suggesting that subjects were not so ill that they performed poorly on all tests.
Overall, the results speak to the need for the integration of psychosocial and pharmacological interventions. Social skills training has proved to be highly effective in improving social skills
(2) and has been shown to have a facilitative interaction with antipsychotic medication
(12). There are also promising results from innovative cognitive rehabilitation programs
(13) that might be effective in improving social problem solving. Further research is also warranted on the potential benefits of targeted adjunctive medications that may enhance cognitive functioning, such as cholinergic and adrenergic agents.