Since the late 1800s, researchers have noted that traumatized individuals often experience dissociative symptoms, such as depersonalization, derealization, amnesia, or fugue states
(1,
2). Most theorists suggest that dissociation is a defensive process in which an individual develops the capacity to separate himself or herself from the psychic and physical pain associated with exposure to traumatic events
(3). This dissociative capacity, in turn, is thought to be used by the individual in future painful circumstances (including during activated trauma memories) as a way to down-regulate his or her experience of acute psychological distress
(4–
6).
Researchers have reported a tendency for some individuals to dissociate during or soon after traumatic events, a phenomenon referred to as peritraumatic dissociation
(7,
8). This response, typically involving depersonalization or derealization, has been linked to the subsequent development of posttraumatic stress disorder (PTSD) in a number of studies
(7–
12). A recent meta-analysis
(13), for example, concluded that peritraumatic dissociation may be the largest known psychological risk factor for PTSD. A common explanation for these findings is that dissociation occurring around the time of a traumatic event may interfere with the encoding and immediate processing of traumatic memories, thereby increasing the eventual likelihood of PTSD
(14,
15).
Despite these findings, a smaller group of studies have failed to replicate the relationship between peritraumatic dissociation and PTSD
(16–
18) or have found that the relationship between peritraumatic dissociation and PTSD disappears after other variables are controlled
(19). Such contrary results have led some researchers to question the relevance of peritraumatic dissociation in acute stress disorder
(20), where it is a central symptomatic feature.
Among the possible reasons for conflicting findings in this area, in addition to sampling and measurement differences, are two that are relevant to the current investigation: 1) significant variability in the extent to which studies control for moderating or mediating variables in the presumed dissociation-PTSD relationship and 2) potentially incomplete specification of the temporal boundaries of peritraumatic dissociation. For example, the majority of studies have not examined the extent to which the peritraumatic dissociation they measure persists over time. As a result, it is difficult to determine whether—as some suggest—the time of onset of dissociation is the critical issue or whether the more important risk factor is the persistence of such dissociation into the long term. If peritraumatic dissociation is presumed to increase the likelihood of PTSD by blocking initial processing, it seems likely that ongoing dissociation would have an even larger effect by disrupting such processing over a more extended period.
Inclusion of a measure of persisting dissociation in peritraumatic dissociation research would help resolve the chronology issue. If both peritraumatic and persistent dissociation were evaluated multivariately, the role of peritraumatic dissociation in PTSD could be considered with control for duration. If the peritraumatic aspect of dissociation leads to PTSD, one would expect a measure of this construct to remain a strong predictor of posttraumatic stress regardless of whether persistent dissociation was taken into account. If, however, peritraumatic dissociation is associated with PTSD only to the extent that it continues beyond the trauma, control for persistent dissociation would eliminate all or most of the relationship between peritraumatic dissociation and PTSD while preserving the relationship between persistent dissociation and PTSD.
A relationship between persistent dissociation and posttraumatic stress would not be surprising. Dissociation is a major component of the DSM-IV-TR diagnostic criteria for acute stress disorder, is listed as an associated feature of PTSD, and is described by some as an integral aspect of posttraumatic stress
(21). Notably, however, DSM-IV-TR acute stress disorder criteria require that dissociative symptoms occur “while experiencing or after experiencing the distressing event” [p. 471], yet DSM-IV-TR also states elsewhere that “the disturbance lasts for a minimum of 2 days” [p. 472]. The seeming contradiction between these two criteria—one referring to peritraumatic dissociation and the other to persistent dissociation—no doubt adds to the confusion in this area.
Despite the potentially important role of trauma-specific, persistent dissociation (however defined) in the etiology of PTSD, only a few studies have examined sustained posttraumatic dissociation as a specific phenomenon
(22–
24). Furthermore, there are few published reports to date discriminating persistent dissociation from peritraumatic (but not necessarily persistent) dissociation in the prediction of posttraumatic stress
(20). Of interest, these few studies suggest that persistent dissociation is more related to acute stress disorder or PTSD than is peritraumatic dissociation.
Sustained dissociation alone may not be sufficient to explain the relationship between peritraumatic dissociation and PTSD. Although persisting dissociation may be a potential risk factor for PTSD because it blocks the processing of trauma-specific memories, it is also possible that the presence of any dissociation may be a marker for an increased likelihood of PTSD, including dissociation that an individual experienced before the index trauma. This is referred to as “generalized dissociation” for the purposes of this study and may be especially relevant for individuals who have a history of exposure to multiple traumas.
Finally, an additional predictor of PTSD is the extent of negative emotionality that an individual experiences at the time of the trauma
(25,
26). It has been hypothesized that peritraumatic dissociation serves as a way to avoid the painful feelings immediately evoked by exposure to trauma
(9,
10). Therefore, the negative emotional impact of a given trauma may produce both an increased likelihood of PTSD and peritraumatic dissociation. In this instance, the causal link between peritraumatic dissociation and PTSD might be smaller or nonexistent, and as a result, any statistical relationship between theses two variables might attenuate or disappear once peritraumatic distress was taken into account. Unfortunately, beyond one early investigation
(27), the multivariate relationship between peritraumatic distress and peritraumatic dissociation has rarely been studied, especially in relation to a heightened risk for PTSD.
Given these potential complexities, two studies were conducted to evaluate the relationship between PTSD and a number of potential predictors that were multivariately considered: exposure to trauma, peritraumatic dissociation, peritraumatic distress, trauma-specific persistent dissociation, and generalized dissociation.
Method
Study 1
A group of 52 trauma-exposed residents of a southern U.S. community were recruited through newspaper advertisements and flyers for a study on the effects of traumatic life events. After approval was obtained from the institutional review board at Auburn University, the participants were individually interviewed with the Clinician-Administered PTSD Scale
(28) and administered a series of instruments. Among these were the Peritraumatic Dissociative Experiences Questionnaire
(10), the Dissociative Experiences Scale
(29), and the Detailed Assessment of Posttraumatic Stress
(30).
The Clinician-Administered PTSD Scale interview has very good test-retest reliability, internal consistency, and predictive validity with respect to a Structured Clinical Interview for DSM-IV diagnosis of PTSD
(31). The Peritraumatic Dissociative Experiences Questionnaire is a reliable and valid 10-item research measure that evaluates self-reported dissociative symptoms that occurred at the time of the traumatic event
(9,
10). The Dissociative Experiences Scale is a widely used, 28-item measure of general dissociative symptoms with demonstrated reliability and strong evidence of various types of validity
(32). The Detailed Assessment of Posttraumatic Stress is a 104-item, standardized clinical test that includes information on an individual’s history of exposure to trauma, immediate reactions to a traumatic event, and diagnostic status for PTSD and acute stress disorder
(30,
33). Relevant to the current research, the peritraumatic distress subscale of the Detailed Assessment of Posttraumatic Stress specifically asks about negative emotional responses at the time of the trauma. Another component, the trauma-specific dissociation subscale, evaluates persistent dissociation, i.e., responses such as depersonalization and derealization that reportedly occurred immediately after the trauma and have persisted to the point of the current assessment.
The average age of this convenience sample was 35.9 years (SD=1.8), and 45 (86.5%) were women. The racial breakdown was 80.8% (N=42) Caucasian, 13.5% (N=7) African American/black, 3.8% (N=2) Hispanic, and 1.9% (N=1) “other.”
Discriminant function analysis with the Statistical Package for the Behavioral Sciences (version 11.5) (SPSS Inc., Chicago) was performed on the participants’ Clinician-Administered PTSD Scale PTSD status as a function of gender, their Peritraumatic Dissociative Experiences Questionnaire score, their Dissociative Experiences Scale score, and their peritraumatic distress and trauma-specific dissociation subscale scores from the Detailed Assessment of Posttraumatic Stress.
Study 2
Data for study 2 consisted of all 386 participants from the general population from the normative study of the Detailed Assessment of Posttraumatic Stress who had a history of exposure to at least one DSM-IV criterion A trauma. Analysis of this data set provided a more fine-grained replication and extension of study 1 employing a larger and potentially more representative sample of the general population and newer psychological measures of posttraumatic stress and dissociation. Approved by the institutional review board of the University of Central Florida, this study was a random mailed survey of individuals with cars or telephones in the United States and had a response rate of 11.4%. The average age of this traumatized subsample of the Detailed Assessment of Posttraumatic Stress normative study was 45.2 years (SD=16.7), 209 (52.3%) were men, and the racial breakdown was 83.2% (N=321) Caucasian, 6.5% (N=25) African American/black, 3.6% (N=14) Hispanic, 3.1% (N=12) Asian, 2.1% (N=8) Native American, and 1.6% (N=6) “other.”
Posttraumatic stress disorder in study 2 was determined with the Detailed Assessment of Posttraumatic Stress. Its diagnosis of PTSD has been shown to have good sensitivity (0.88) and specificity (0.86) relative to the Clinician-Administered PTSD Scale PTSD diagnosis
(31). Peritraumatic dissociation was measured with the peritraumatic dissociation subscale of the Detailed Assessment of Posttraumatic Stress, persistent dissociation was evaluated with the Detailed Assessment of Posttraumatic Stress trauma-specific dissociation subscale, and generalized dissociation was measured with the six subscales of the Multiscale Dissociation Inventory
(34). The Multiscale Dissociation Inventory is a psychometrically valid measure of various dissociative responses
(33–
35) that yields six subscale scores: depersonalization, derealization, disengagement, emotional constriction, memory disturbance, and identity dissociation.
Logistic regression analysis was used in study 2, also with use of the Statistical Package for the Behavioral Sciences, version 11.5. Variables were entered in the following order, based on the assumed chronological sequence of response to trauma. At step 1, the demographic variables of age and sex were entered. At step 2, three types of trauma exposure history, as measured by the trauma-specification section of the Detailed Assessment of Posttraumatic Stress, were added to the equation. These were sexual violence (history of childhood or adult sexual victimization), physical violence (a history of childhood or adult physically violent assaults), and accident or disaster (history of childhood or adult motor vehicle accidents, accidents occurring at home or at work, or disasters). At step 3, the participants’ scores on the peritraumatic distress subscale of the Detailed Assessment of Posttraumatic Stress were entered, followed by scores from the Detailed Assessment of Posttraumatic Stress peritraumatic dissociation subscale at step 4 and the Detailed Assessment of Posttraumatic Stress trauma-specific dissociation subscale at step 5. Finally, at step 6, all six subscales of the Multiscale Dissociation Inventory were added to the equation as a block. After all variables had been entered, the final equation was examined to determine the relative contribution of each variable to PTSD status, with control for all other variables. Of the initial 386 participants, 20 had incomplete demographic or test data, resulting in a final sample size of 366 for this analysis.
Results
Study 1
Fourteen (26.9%) of 52 trauma-exposed subjects in this group were found to have PTSD on the Clinician-Administered PTSD Scale. Discriminant analysis of participant gender and scores on the Peritraumatic Dissociative Experiences Questionnaire, the Dissociative Experiences Scale, and the trauma-specific dissociation and peritraumatic distress subscales predicting PTSD diagnosis revealed a significant multivariate relationship (R
c=0.58, χ
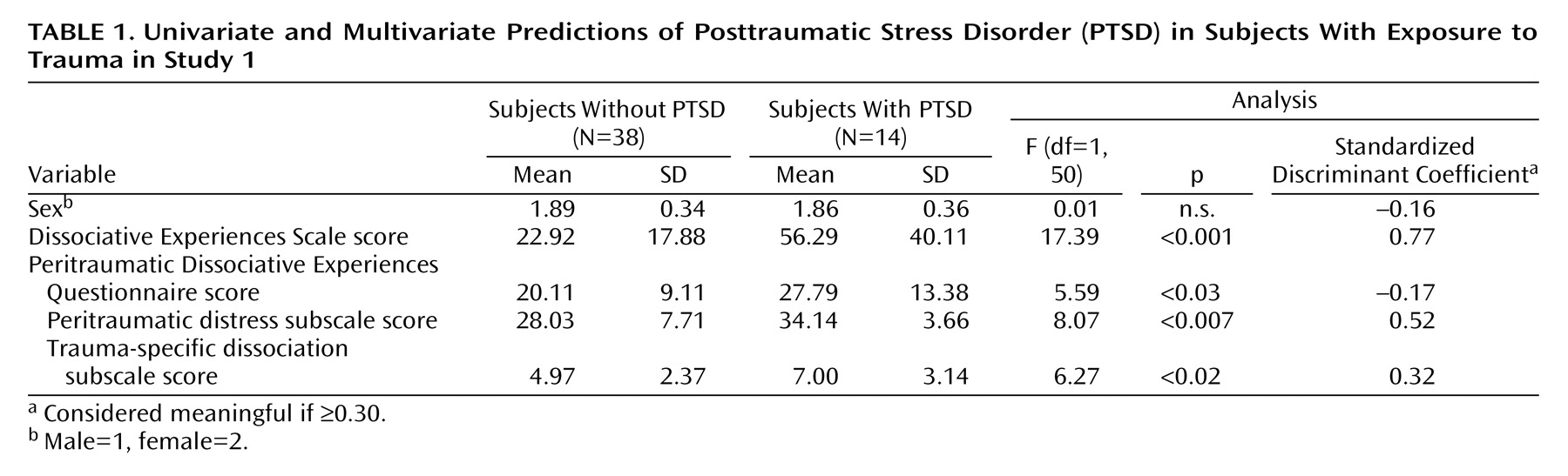
2=19.69, df=5, p<0.001). As shown in
Table 1, the standardized discriminant function coefficients and post hoc analysis of variance (ANOVA) results indicate that several variables discriminated PTSD-positive versus PTSD-negative status. The univariate ANOVA results revealed that when they were considered individually, scores on the Peritraumatic Dissociative Experiences Questionnaire, the Dissociative Experiences Scale, and the subscales for peritraumatic distress and trauma-specific dissociation all were associated with PTSD. When the unique contribution of each variable was evaluated by discriminant analysis, i.e., with control for all other variables in the equation, all but one of these variables emerged as meaningful discriminators. The discriminant function coefficients indicated that although scores on the Dissociative Experiences Scale and the peritraumatic distress and trauma-specific dissociation subscales continued to be meaningful discriminators of PTSD, scores on the Peritraumatic Dissociative Experiences Questionnaire were no longer related.
Study 2
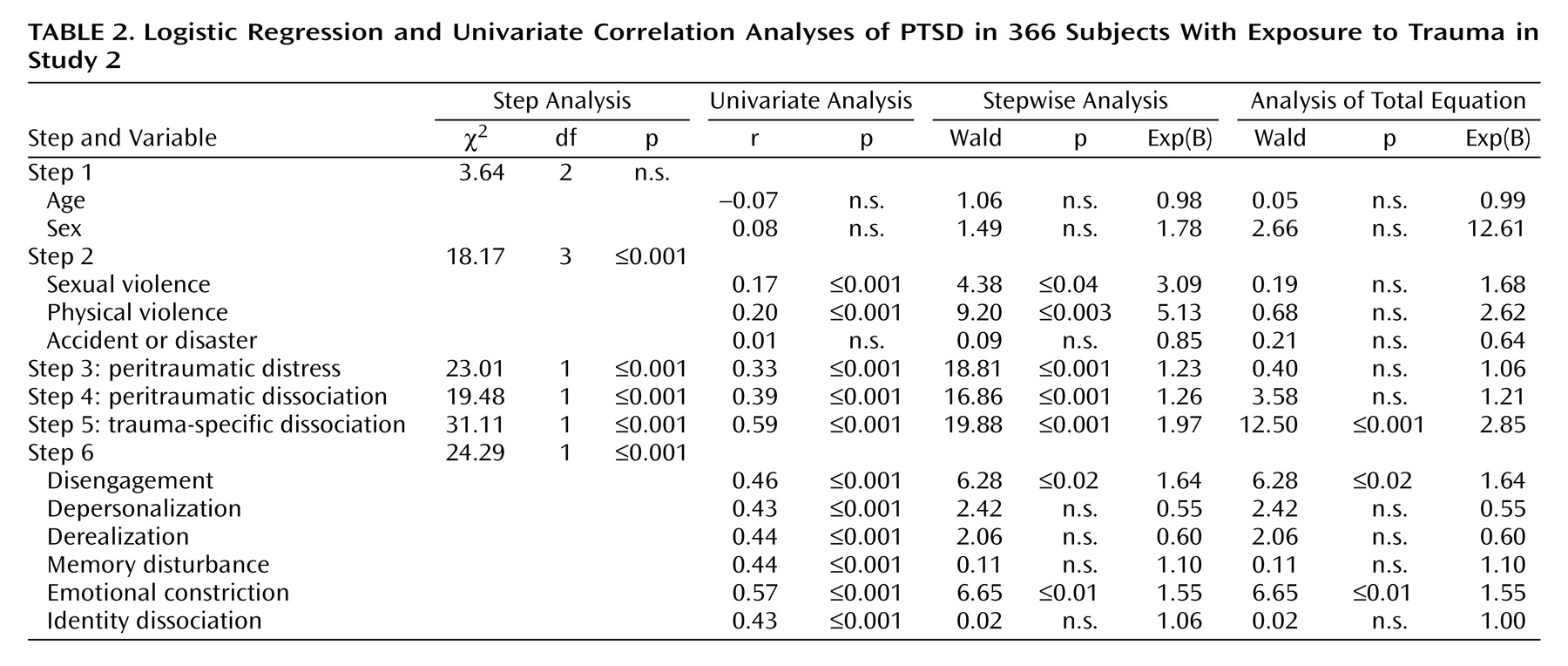
A total of 22 (6.0%) of 366 trauma-exposed participants from the general population sample endorsed symptoms on the Detailed Assessment of Posttraumatic Stress that met DSM-IV criteria for PTSD. Univariate correlation analysis indicated that PTSD was associated with exposure to physical and sexual violence on both of the Detailed Assessment of Posttraumatic Stress dissociation subscales (trauma-specific dissociation and peritraumatic dissociation), peritraumatic distress, and all six subscales of the Multiscale Dissociation Inventory (
Table 2). Perhaps most noteworthy of this first set of findings is the substantial univariate relationship between persistent dissociation (as tapped by the trauma-specific dissociation subscale) and PTSD, which accounted for 34.8% of the variance in PTSD diagnosis. In contrast, 15.2% of the variance in PTSD was accounted for by peritraumatic dissociation.
As shown in
Table 2, stepwise logistic regression analysis revealed that PTSD was unrelated to demographic variables at step 1 but was associated with exposure to sexual and physical violence at step 2; peritraumatic distress, peritraumatic dissociation, and persistent dissociation at steps 3, 4, and 5; and disengagement and emotional constriction at step 6. In other words, the stepwise results indicated that each variable made a significant contribution to the prediction of PTSD, even when all variables entered at prior steps were taken into account. Significantly, peritraumatic dissociation remained a significant predictor at step 4 even after there was control for trauma exposure and posttraumatic distress. When all variables were considered simultaneously (i.e., after step 6), however, peritraumatic distress and peritraumatic dissociation were no longer related to PTSD, whereas persistent dissociation, disengagement, and emotional constriction continued to be significant predictors.
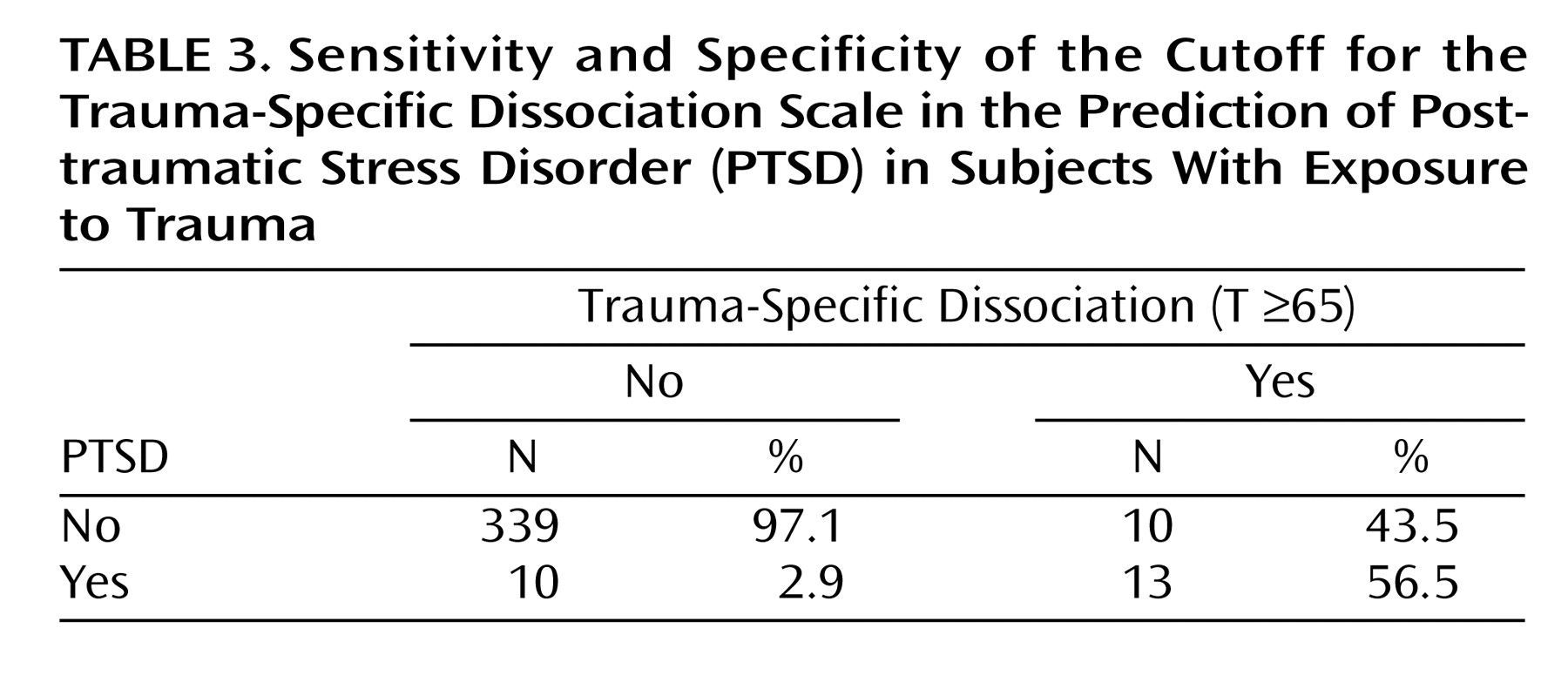
Because persistent dissociation was a major predictor of PTSD status in both studies, a final analysis was conducted to evaluate the use of the Detailed Assessment of Posttraumatic Stress trauma-specific dissociation subscale as a stand-alone predictor of PTSD. This analysis included six additional participants who had missing scores on other scales but whose data were complete for PTSD and the trauma-specific dissociation subscale. When the standard clinical cutoff (a T score of 65 or higher)
(34) was used to index the presence or relative absence of persistent dissociation on the trauma-specific dissociation subscale, cross-tabulation with PTSD status indicated a specificity of 0.97 and a sensitivity of 0.57. Examination of
Table 3 reveals that trauma-exposed individuals with nonclinical levels of persistent dissociation had a 2.9% likelihood of PTSD, whereas those with clinical levels had a 56.5% likelihood of PTSD (χ
2=107.10, df=1, p<0.001).
Discussion
As reported in other investigations, univariate analyses in studies 1 and 2 indicated that peritraumatic dissociation is a significant predictor of PTSD status. However, this relationship ceased to be significant in both studies once persistent dissociation was taken into account by multivariate analyses. In contrast, a substantial relationship was found between persistent dissociation and PTSD at both univariate and multivariate levels. Univariate analyses in study 2 indicated that the persistence of dissociative symptoms after trauma predicted over a third of the variance in PTSD diagnosis, compared to approximately one-sixth of the PTSD variance accounted for by peritraumatic dissociation. This relationship remained in studies 1 and 2 even when the variance associated with peritraumatic and generalized dissociation had been statistically removed. Cross-tabulation of the participants’ trauma-specific dissociation scores with their PTSD status revealed that those with subclinical levels of persistent dissociation were unlikely to experience PTSD, whereas those with clinically elevated levels had more than a 50% likelihood of developing PTSD.
Of interest, the stepwise logistic results of study 2 indicated that although peritraumatic dissociation did not predict PTSD when all other variables were taken into account, it was a significant predictor at step 4, i.e., before persistent dissociation was added but after control was added for trauma exposure and peritraumatic distress. These results suggest that peritraumatic dissociation may not be simply an avoidance response to trauma-related emotional distress, at least in terms of its relationship to PTSD. Removing any variance in peritraumatic dissociation that was associated with exposure to trauma and peritraumatic distress did not eliminate the association of this variable with PTSD. Explanations for this result include the possibility that 1) although peritraumatic dissociation may arise, in part, from peritraumatic distress, other variables not monitored in this study (e.g., reduced capacity for affect regulation) also may be relevant, or 2) peritraumatic dissociation has little to do with a defensive response to trauma-related distress but instead may reflect other processes, for example, the effects of overwhelming autonomic arousal on perception and awareness.
Overall, the findings of studies 1 and 2 suggest that the primary risk for PTSD is less whether one dissociates during (or soon after) a traumatic event than whether such dissociation persists over time. Although it is possible that peritraumatic and persistent dissociation reflect the same underlying phenomenology and function, the temporal component of this response appears to be critical. At the same time, a high level of persistent dissociation is apparently not necessary to produce all cases of PTSD: nearly half of the PTSD-positive individuals in study 2 did not have clinically elevated scores for trauma-specific dissociation. Future research is indicated 1) to determine the specific causal role of persistent dissociation in PTSD, including at what level it may become contributory (for example, persistent dissociation may increase the likelihood of PTSD at lower levels than what is indexed by the established clinical cutoff for trauma-specific dissociation on the Detailed Assessment of Posttraumatic Stress) and 2) to further examine other variables that increase the likelihood of PTSD in the context of persistent dissociation. In any event, the current findings support the contention of Harvey and Bryant
(20) that peritraumatic dissociation may have a less powerful relationship to PTSD than initially thought.
The current findings do not directly explain why persistent dissociation is more related to PTSD than is transient (i.e., solely peritraumatic) dissociation, although there are several possibilities. First, persistent dissociation may be an underrecognized “part” of PTSD, in which case it may constitute early evidence of an emerging posttraumatic stress syndrome in a given individual. Second, event-specific dissociation that persists over time may occur as a function of trauma severity, which, in turn, is associated with the likelihood of PTSD
(36). The current study attempted to control for this possibility through multivariate analysis in which the relationship between persistent dissociation and PTSD was examined after control was added for trauma type (sexual versus physical violence versus accidents or disasters) and how upsetting the individual found the trauma (peritraumatic distress). At a minimum, the current findings do not contradict existing clinical theory, i.e., that persisting trauma-specific dissociation increases the likelihood of PTSD by blocking normal trauma processing, perhaps by decreasing the individual’s ongoing exposure and desensitization to traumatic memories and associated affects over time
(37–
39).
The current study also examined the association between generalized dissociation and PTSD. In both study 1 and study 2, overall dissociation, indexed by the Dissociative Experiences Scale and the Multiscale Dissociation Inventory, respectively, predicted variance in PTSD independent of that predicted by peritraumatic and persistent dissociation. However, study 2 suggests a smaller role for generalized dissociation once other forms of dissociation are taken into account. Although all six Multiscale Dissociation Inventory subscales were significant univariate predictors, only two (disengagement and emotional constriction) were associated with PTSD at the multivariate level. Of these two, emotional constriction would be expected to correlate with PTSD by virtue of its similarity to the emotional numbing criteria of that diagnosis.
Although generalized dissociation may represent an additional—albeit perhaps limited—predictor of PTSD, it is possible that the symptoms measured by the Dissociative Experiences Scale or the Multiscale Dissociation Inventory are the sum total of all forms of persisting posttraumatic dissociation that a given individual has experienced across multiple events. A participant’s score on the trauma-specific dissociation subscale reflects dissociation in response to a single specified trauma—not all traumas that the participant ever has encountered. Thus, it may be hypothesized that if trauma-specific dissociation scores were collected for all major trauma exposures per individual, scores on the Dissociative Experiences Scale or the Multiscale Dissociation Inventory might not account for additional variance in PTSD. This supposition is an empirical question, however, that deserves additional research attention.
Interpretation of the findings reported here must be tempered by the limitations of the present study. The recruitment of participants in study 1 was subject to self-selection bias because those who responded to newspaper or other media advertisements may have differed from those who did not volunteer. Further, the mailing method used to collect the general population sample in study 2 omitted, by definition, those who did not have mailing addresses (e.g., incarcerated, hospitalized, or homeless people), as well as those who could not read English. In addition, the response rate for this sample was below that considered optimal for mailed studies and thus may represent another example of self-selection bias. The effects of these convenience sample characteristics on the generalizability of the current results cannot be fully determined. However, the fact that studies 1 and 2 produced similar results, despite different participants, measures, and statistical approaches, suggests a significant degree of external validity.
The implications of these findings are several. First, the oft-cited notion that peritraumatic dissociation predicts PTSD may overlook the important question of whether such dissociation is sustained over time. The current results suggest that transient peritraumatic dissociative responses predict little independent variance in PTSD relative to persistent dissociation. To the extent that the persistence of dissociation is a more important variable, those studying the effects of dissociation during (or immediately after) a traumatic event may need to inquire further as to the duration of whatever dissociative symptoms have been identified. Second, the fact that peritraumatic dissociation does not make a unique contribution to the prediction of PTSD suggests that the criteria for acute stress disorder might be sharpened by discriminating between peritraumatic and persistent dissociation and by weighing the latter to a greater extent than the former.