Subjects
A total of 125 subjects were evaluated from three cities in Armenia, Spitak, Gumri, and Yerevan, each city located at increasing distances from the epicenter of the earthquake. Spitak, a city a few miles from the epicenter, was almost totally destroyed. Seventeen percent of the population died. Residents experienced extreme threats to their lives and witnessed mutilating injuries and grotesque deaths. These traumatogenic experiences persisted for days after the earthquake. In Gumri, located 20 miles from the epicenter, exposure to trauma was also severe. Destruction was uniform throughout the city, with 50% of the buildings destroyed and 90% substantially damaged. Approximately 7% of the population was killed. The severity of exposure to trauma was only slightly less than that of Spitak. In Yerevan, the capital of Armenia, located 47 miles from the epicenter, damage to buildings was less extensive, and there were no deaths attributable to the earthquake. However, residents had indirect exposure by way of constant media coverage, with highly disturbing images of the death and destruction in the earthquake zone.
The initial study conducted 1.5 years after the earthquake has been described in detail elsewhere
(13). Because of the multiplicity of hardships facing both the victims and the staff working in the earthquake zone, and the lack of available mental health personnel, this study focused on following a subgroup of the original group. For estimation of group size, a power analysis indicated that 21 subjects per study group was the minimum size necessary to obtain significant results (power=0.80, alpha=0.01). For the follow-up, every other untreated subject from the original study was selected. Because the number of treated subjects from the original group was small, all those who had received treatment were targeted for follow-up.
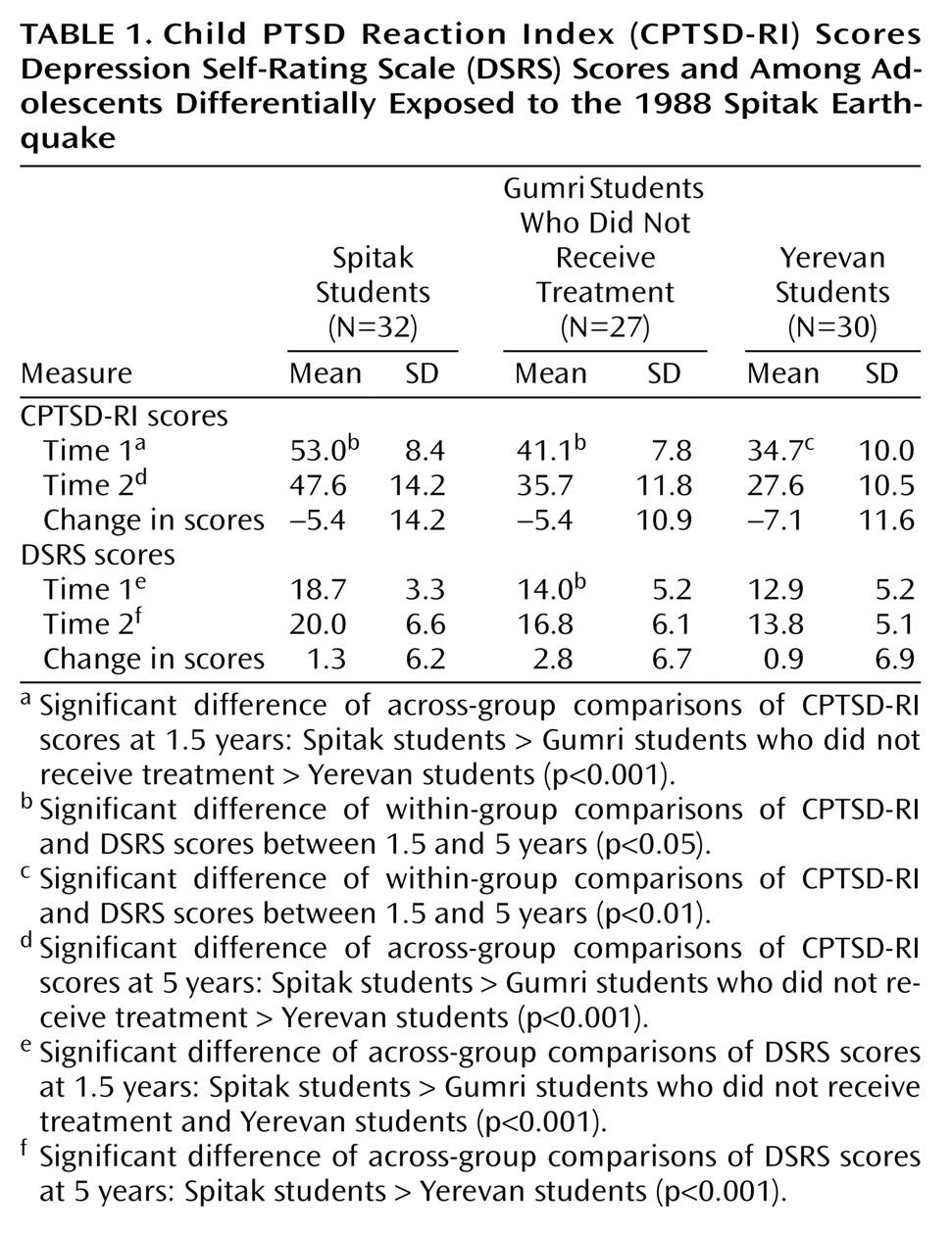
The original group from Spitak that had been previously evaluated at 1.5 years after the earthquake consisted of 63 students. Two subjects were lost at the 5-year follow-up. Thus, the group for this study consisted of 32 students (i.e., every other student from the available 61), with 12 boys of an average age of 16.6 (SD=0.5, range=16–17) and 20 girls of an average age of 16.5 (SD=0.5, range=16–17). The subjects were drawn from two schools from the two main regions of the city. None of the subjects in this group had received psychological treatment. The number of deaths of nuclear family members for the subjects from this group was 11, two of whom were from the same household.
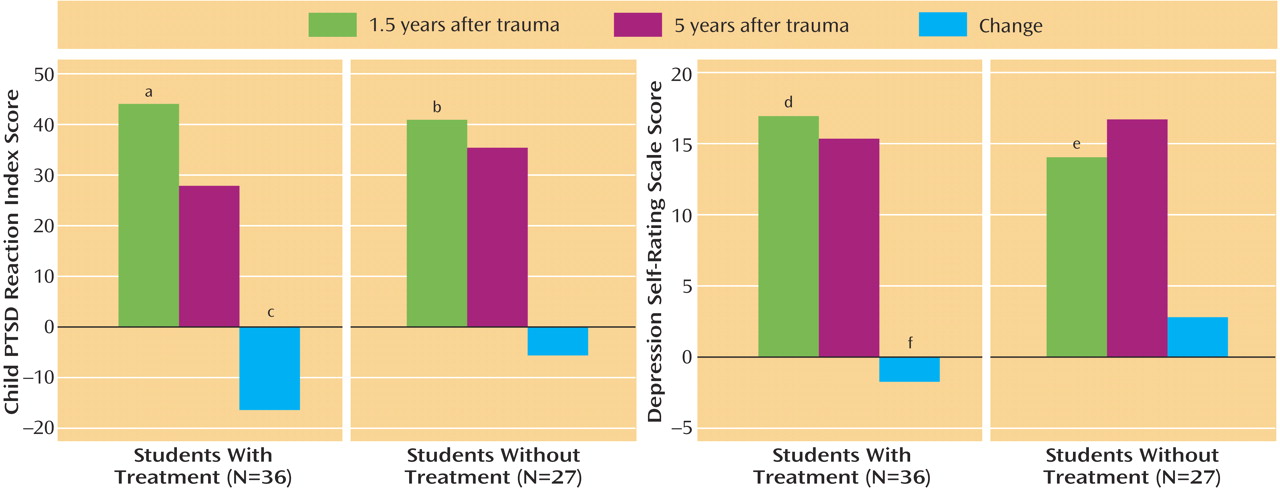
The students from Gumri consisted of two groups: those who had received treatment and those who had not. The original treatment group consisted of 38 students. Two were lost at the 5-year follow-up, leaving 36, with 14 boys of an average age of 16.2 (SD=0.4, range=15–17) and 22 girls of an average age of 16.3 (SD=0.5, range=16–17). The number of deaths of nuclear family members for the subjects in this group was 10, each from a different family. The untreated group originally consisted of 56 students. Two subjects were lost to follow-up. Thus, the group for the present study consisted of 27 students (i.e., every other student from the available 54 students), with 11 boys of an average age of 16.4 (SD=0.5, range=16–17) and 16 girls of an average age of 16.4 (SD=0.5, range=16–17). The number of deaths of nuclear family members for this group was four, each from a different family. The schools in Gumri were selected from the four major regions of the city, where morbidity, mortality, damage, and destruction had been pervasive and uniform. The students who received treatment were from two Gumri schools that were chosen for intervention because of their proximity to our clinic. Because of a lack of clinical resources, we could not provide intervention in the other schools that were screened at 1.5 years after the earthquake in Gumri. Thus, the students in these schools served as comparison subjects for the present study. The fourth group was from Yerevan, the capital of Armenia, located 47 miles from the epicenter. Only one of the original 60 students was lost to follow-up. This group consisted of 30 students (i.e., every other student from the available 59), with 14 boys of an average age of 15.6 (SD=0.5, range=15–16) and 16 girls of an average age of 15.7 (SD=0.5, range=15–16). None of these students had received psychological treatment. There were no deaths of nuclear family members for the subjects in this group.
The principals of the schools that participated gave their approval for the study. The parents were informed of the evaluations and gave written informed consent for their child’s participation. The adolescents who participated gave their assent. None declined to participate.
Statistical Analyses
Skewness coefficients on all groups indicated a normal distribution of data, thereby permitting the use of parametric tests. Even though the ages of the subjects fell within a narrow range, an analysis of covariance was performed with age as a covariate. The results indicated that there was no age-by-city or time effect. Consequently, age groups were collapsed for further analyses. Analysis of variance (ANOVA) was used to analyze differences among the three groups (Spitak, Gumri, and Yerevan) that did not receive treatment on the CPTSD-RI total score, as well as B, C, and D subcategory scores, DSRS scores, and the change in scores between 1.5 and 5 years for both scales. Additionally, repeated-measures ANOVA was used to examine within-group changes over time for these variables. To examine differences on the distress measures between the two Gumri groups (treatment versus no treatment), t tests were used to analyze each of the distress measures. Sex differences were also analyzed with the t test.