In the United States, the annual prevalence of major depressive episode is about 17%
(1), and 1.3% of adults ages 18–54 years experience posttraumatic stress disorder (PTSD) during the course of a year
(2). Between 14% and 25% of individuals exposed to catastrophic trauma develop PTSD
(3–
5), and as many as one-half of them have at least one additional axis I diagnosis. In 26%, the additional diagnosis is major depressive episode
(6). Indeed, within 8 months of a traumatic event, 23% of exposed adults develop major depressive episode, with or without PTSD, often within days of the event
(7).
Preexisting major depression increases susceptibility to the effects of traumatic events as well as ordinary stressful life events
(8). At the same time, PTSD increases the risk for the first onset of major depression
(9,
10). Thus, these two disorders are common and often comorbid, and the presence of one diagnosis compounds risk for the development of the other.
Both PTSD and major depressive episode are associated with risk for suicidal behavior. Lifetime prevalence of suicide attempts in major depressive episode is approximately 16%
(11). In a community survey, patients with PTSD were 14.9 times more likely to attempt suicide than subjects without PTSD
(12). Although suicide rates are higher in Vietnam-era veterans than in the general population, studies of these veterans have yielded conflicting results regarding the degree of the difference in risk for suicide attempts and the extent of suicidal ideation in trauma victims. Some suggest that the risk of suicidal behavior in veterans with PTSD, while greater than that of nonveterans, has been overestimated
(13). However, others find that specific symptoms within PTSD, such as guilt or anxiety, not the presence of PTSD in general, are responsible for higher suicide risk
(14,
15)Some
(16–
18) but not all
(19) studies of suicidal ideation and behavior in subjects with comorbid PTSD and major depressive episode found that PTSD and major depressive episode interact to increase the level of suicidal ideation and behavior, compared with that in subjects with PTSD or major depressive episode alone. However, the relationship between major depressive episode, PTSD, and suicidal behavior is likely to be influenced by other factors. For example, child abuse increases the risk for PTSD, major depression, and suicidal behavior. About one-third of those who have been abused or neglected during childhood develop PTSD
(20), and a history of childhood abuse more than doubles the odds of developing major depressive episode
(21). Early childhood trauma, including abuse, has also been associated with self-destructive and suicidal behavior later in life
(22,
23).
Both suicidal behavior and a childhood history of abuse and trauma are also associated with borderline personality disorder
(24,
25), and some researchers have conceptualized borderline personality disorder as a form of chronic PTSD
(26). In addition, borderline personality disorder is often comorbid with major depression
(27). Thus, the influence of PTSD on suicidal ideation and behavior requires attention to a constellation of risk factors, including major depressive episode, personality disorder, and childhood history of abuse, as well as concomitant traits such as impulsivity and aggression that are often part of the clinical picture in cluster B personality disorders and are associated with suicidal acts.
We recently reported that patients presenting for treatment of major depression who had PTSD were more likely to have exhibited suicidal behavior and that the effect of PTSD was independent of the presence of cluster B personality disorders, childhood history of abuse, and aggressive behavior
(17). We sought to replicate these findings, and in this study we examine the relationship between suicidal behavior and PTSD, while taking into account known risk factors for suicidal behavior, including cluster B personality disorders, childhood sexual or physical abuse, and history of aggression/impulsivity. We report the findings from this larger, mostly independent group of adults with a history of a major depressive episode. We hypothesize that in patients with a history of major depressive episode, those with PTSD will be more likely to attempt suicide and will differ from those without PTSD in other measures of suicidal behavior.
Method
Subjects
Subjects were recruited from inpatient units in New York (New York State Psychiatric Institute and Payne Whitney Clinic) and in Pittsburgh (Western Psychiatric Institute and Clinic and St. Francis Hospital) and in both cities by advertisement. About one-half of the subjects were inpatients at the time of assessment (N=108 [49%]). Subjects (N=230) with current or past major depressive episode were entered into the study after giving written informed consent. Thirty-one subjects with a lifetime history of major depressive episode in this group were included in the study group described in our previous report (total N=156)
(17), of whom six had a history of lifetime PTSD.
Assessment
Subjects were assessed for the presence of lifetime and current DSM-IV psychiatric disorder with the Structured Clinical Interview for DSM-IV (SCID)
(28). Patients were assessed for severity of depressive symptoms by a research clinician using the Hamilton Depression Rating Scale
(29) and by means of patients’ self-report with the Beck Depression Inventory
(30). Suicide attempts were defined as self-inflicted injury with intent to end one’s life. Lifetime history of suicidal behavior was gathered by using the Columbia University Suicide History form
(31). The degree of medical injury from suicide attempts was measured with the Lethality Rating Scale
(32). Suicidal intent and ideation were measured with the Suicide Intent Scale
(32) and the Scale for Suicidal Ideation
(33), respectively. Hopelessness was assessed with the Beck Hopelessness Scale
(34). Lifetime aggression was measured by using the Brown-Goodwin aggression history scale
(35), hostility with the Buss-Durkee Hostility Inventory
(36), and impulsivity with the Barratt impulsivity scale
(37). Axis II disorders were diagnosed with the Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II)
(38). Subjects were assessed for a history of physical and sexual abuse during childhood by using a series of screening questions in the demographic questionnaire.
Diagnostic Procedure
All interviewers were master’s- or doctoral-level clinicians or psychiatric nurses who received extensive training in the administration of semistructured interviews. Best-estimate diagnoses were made by consensus on the basis of all available data sources at diagnostic consensus conferences attended by research clinical staff, including psychiatrists. Within- and cross-site reliability for the SCID and SCID-II, suicide history, and the Brown-Goodwin aggression history scale were high (intraclass correlation=0.82–0.98, kappa=0.86–0.95).
Statistical Analysis
Frequencies and associations between variables were examined. Demographic and clinical variables were compared in subjects with and without a lifetime history of PTSD by using Student’s t test for continuous variables and the chi-square test or Fisher’s exact test for categorical variables. Because not all subjects were experiencing a major depressive episode at the time of assessment, state-dependent clinical variables were compared by analysis of variance, with adjustment for Hamilton depression scale scores. We compared the age at onset of PTSD and the age at first suicide attempt of all suicide attempters with a history of PTSD. Then, a stepwise backward logistic regression was constructed with lifetime suicide attempter status as the dependent variable and lifetime PTSD, childhood history of abuse, cluster B personality disorder, impulsivity score, and aggression score as the independent variables.
Results
Subjects’ Demographic Characteristics
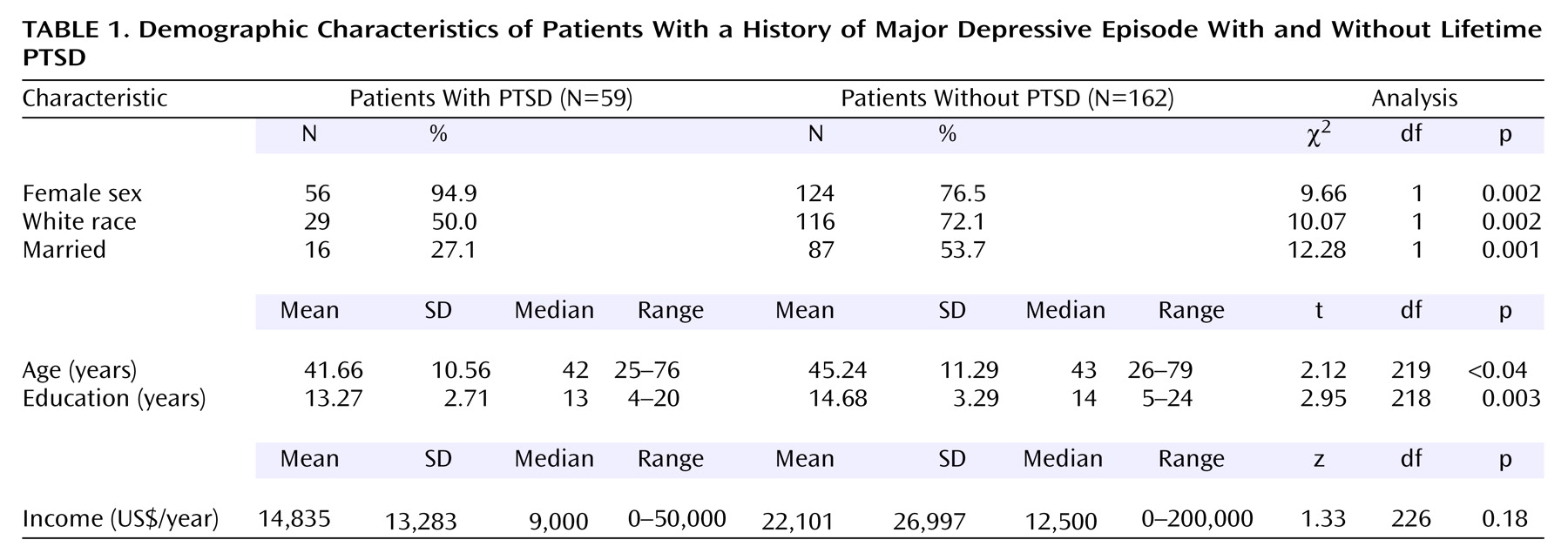
Fifty-nine subjects (25%) had a lifetime history of PTSD. Subjects with lifetime PTSD and subjects without PTSD did not differ significantly in age or income. Compared to subjects without PTSD, subjects with lifetime PTSD were significantly more likely to be female, nonwhite, and unmarried and to have fewer years of education (
Table 1).
Severity of Acute Psychopathology
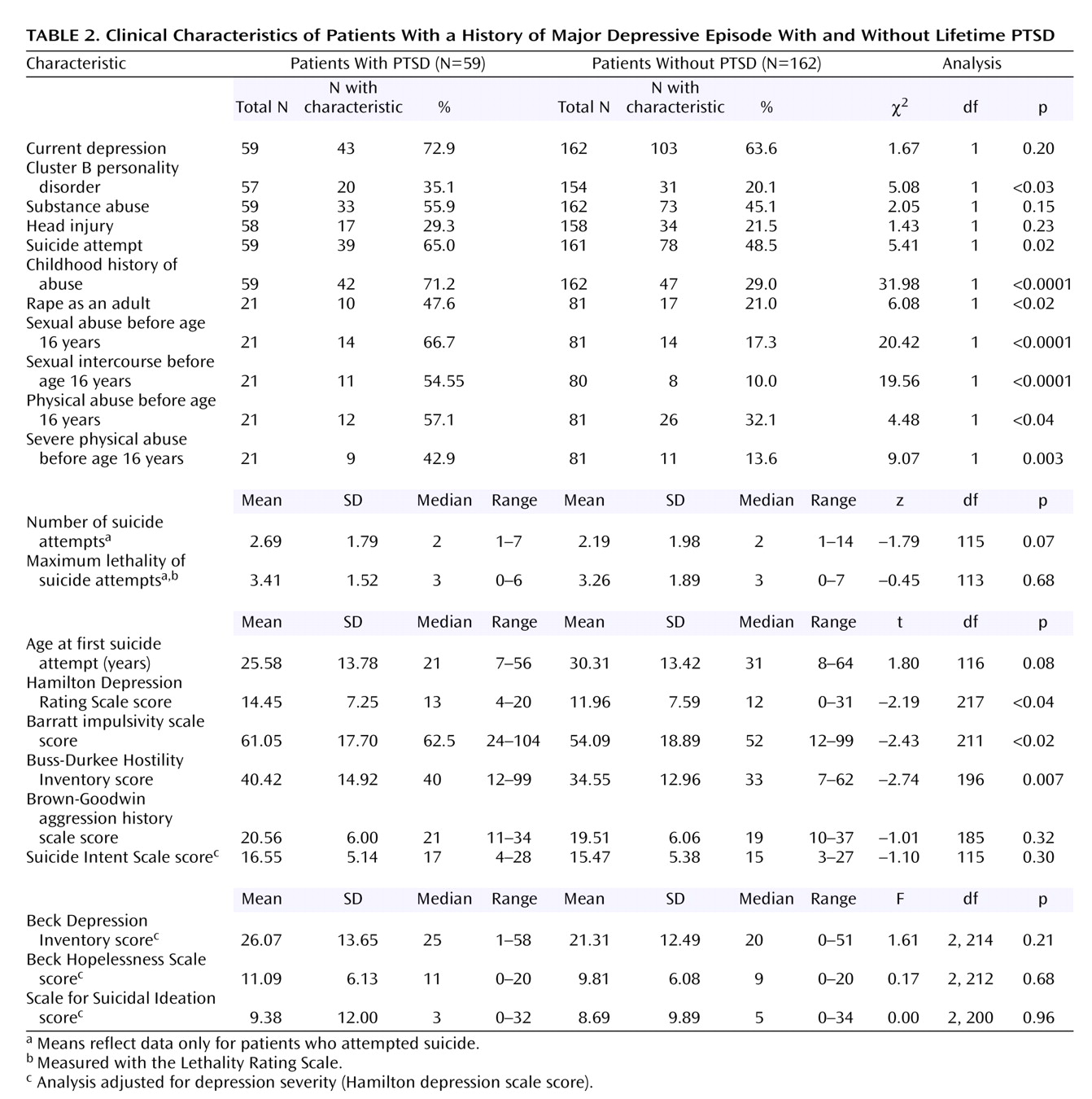
The group with lifetime PTSD had significantly higher objective depression ratings (Hamilton depression scale), compared to the group with no history of PTSD (
Table 2). There were no significant differences between the groups in the level of subjective depression (Beck Depression Inventory) or hopelessness (Beck Hopelessness Scale) or in presence of a current depressive episode (
Table 2).
Comorbid Conditions and Character Traits
Subjects with lifetime PTSD had significantly higher rates of comorbid cluster B personality disorders, but not of substance abuse or head injury (
Table 2). Higher impulsivity (Barratt impulsivity scale) and hostility scores (Buss-Durkee Hostility Inventory), but not higher lifetime aggression scores (Brown-Goodwin aggression history scale), were found in the group with lifetime PTSD.
Suicidal Behavior
Patients with lifetime PTSD were significantly more likely to have made a suicide attempt. However, contrary to our hypothesis, the groups did not differ in suicidal ideation, after adjustment for depression severity, or suicidal intent at the time of the most lethal attempt. Among subjects with a history of suicide attempt, there was no difference between the lifetime PTSD group and the group without PTSD in the number of attempts made or the maximum level of lethality of the suicide attempts. The first suicide attempt occurred at an earlier age for attempters with PTSD than for attempters with no PTSD, but the difference did not reach statistical significance (
Table 2).
Trauma History
A significantly greater number of subjects with lifetime PTSD than of those without PTSD reported a childhood history of abuse. Lifetime PTSD subjects were more likely to have experienced sexual abuse (including intercourse) before age 16 years, physical abuse before age 16 years, severe physical abuse before age 16 years, and rape as an adult (
Table 2).
Age at Onset of PTSD
For subjects with comorbid PTSD, the mean age at PTSD onset was 19.2 years (SD=14.2). Subjects with PTSD who attempted suicide (N=33) were a mean of 26 years old (SD=14) at the time of first attempt. For the most part, PTSD preceded the first suicide attempt (in 24 subjects [72%]), and the age at onset of PTSD and at first suicide attempt showed a positive correlation (Pearson’s r=0.52, N=33, p<0.002).
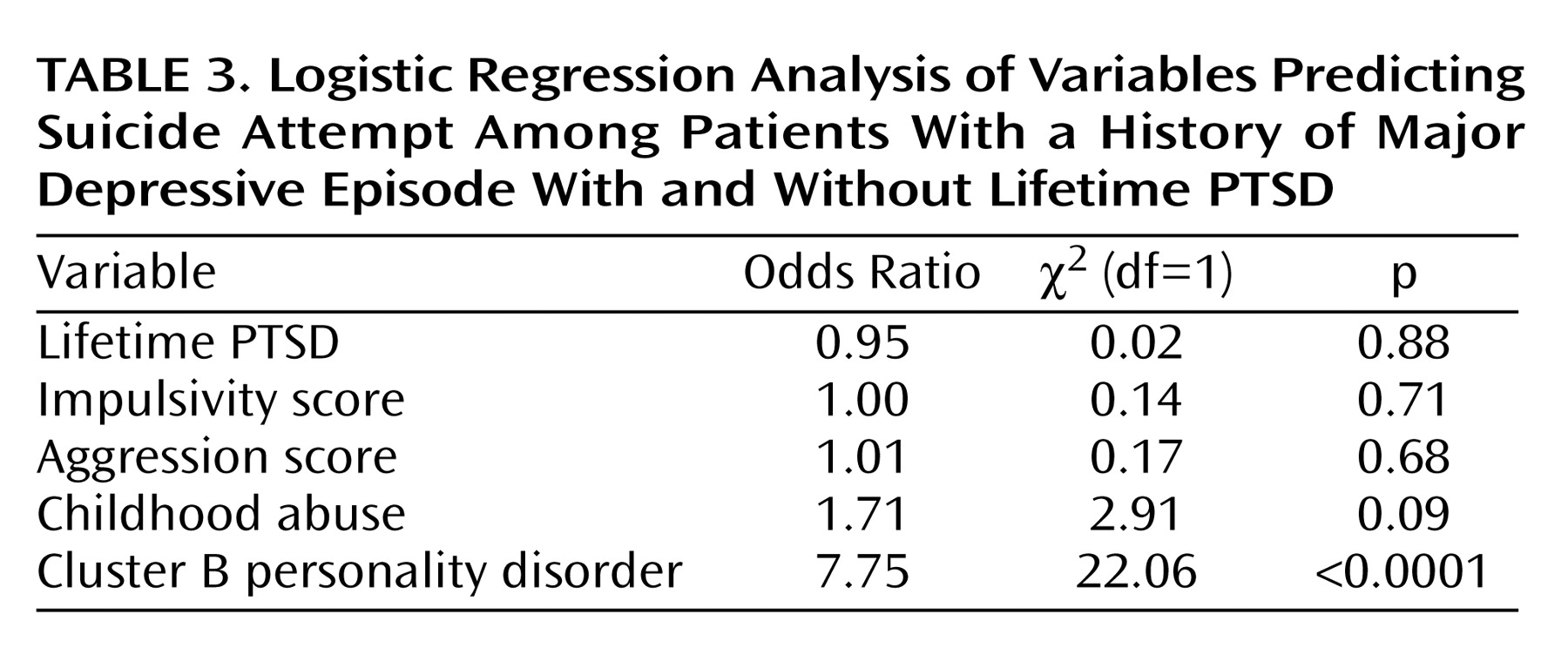
Multivariate Analysis
In a stepwise backward logistic regression with lifetime suicide attempter status as the dependent variable and lifetime PTSD, childhood history of abuse, cluster B personality disorder, impulsivity, and aggression as the independent variables, only cluster B personality disorder was significantly associated with suicide attempt (odds ratio=8.23, 95% confidence interval [CI]=3.41–19.84, χ
2=22.06, df=1, p<0.0001). The association between suicide attempt and a history of childhood abuse approached statistical significance (χ
2=2.91, df=1, p=0.09) (
Table 3).
In multivariate analyses, subjects with major depressive episode and cluster B personality disorder (N=29) were more likely to be suicide attempters than those with major depressive episode and lifetime PTSD (N=39) (p<0.01). However, these two groups did not differ in suicidal ideation. This finding held true when we examined the data for suicide attempters only (N=24 and N=20, respectively), and the number, lethality, and suicidal intent of attempts were similar in the two groups.
Discussion
PTSD, Major Depressive Episode, and Suicidal Behavior
We
(17) and others
(16) have reported that when PTSD is comorbid with major depressive episode, it is associated with higher rates of suicidal acts. In this larger group of subjects with major depressive episode, those with a lifetime history of PTSD were also significantly more likely to be suicide attempters. As in our previous study, we detected no differences in the suicidal behavior exhibited by suicide attempters—regardless of whether they had a lifetime history of PTSD—in terms of suicidal intent, number of previous attempts, age at first suicide attempt, and lethality of previous attempts.
Our previous study reported that acutely depressed subjects who currently also had PTSD had more suicidal ideation than subjects with no history of PTSD. However, no difference in suicidal ideation was seen in depressed individuals with a lifetime history of PTSD, compared to those with no PTSD ever. The present study examined subjects with a lifetime history of PTSD and major depressive episode and likewise detected no difference in suicidal ideation between those with a lifetime history of PTSD and those without PTSD. Perhaps suicidal ideation is heightened only while depressed patients are experiencing PTSD, and ideation lessens once PTSD remits. Marshall et al.
(18) reported that, in subjects with symptoms of PTSD, for each additional symptom that was present, suicidal ideation was likely to occur in a larger proportion of the study group, even when the analysis controlled for the presence of major depression. However, not all studies agree. For example, Shalev et al.
(19) found no difference in suicidal ideation in patients with PTSD and major depressive episode, compared to those with major depressive episode only, although the subjects were recruited from emergency services after experiencing trauma and possibly represented more acutely ill individuals. Whether suicidal ideation increases with PTSD over and above the risk conferred by depression requires further study.
Consistent with the lack of difference in suicidal ideation in the two groups, there were no significant differences between lifetime PTSD subjects and subjects with no PTSD in levels of subjective depression or hopelessness. Both groups had a similar proportion of subjects with a current depressive episode; however, PTSD subjects showed significantly higher objective depression ratings, compared to subjects with no history of PTSD. Although Golier et al.
(39) suggested that comorbidity with PTSD does not result in increased severity of depressive episode, but instead is associated with more pronounced variability in mood, Shalev et al.
(19) noted about twice the severity of depressive symptoms in subjects with PTSD and major depressive episode, compared to those with major depressive episode alone. Moreover, Freeman et al.
(16) reported more depressive symptoms in those with PTSD and suicidal behavior, although comorbidity with depression was not established in that study. PTSD and major depressive episode share a number of symptoms, including sleep disturbance, poor concentration, guilt, restricted affect, and suicidal ideation, all of which, with the exception of restricted affect, are measured by the Hamilton depression scale. We did not measure severity of PTSD symptoms and thus cannot assess the relationship between severity of PTSD and objective severity of depression. However, given that some subjects with a lifetime history of PTSD (N=59) still had ongoing symptoms of PTSD (N=37 [62%]), it is not surprising that a history of these two disorders leads to higher ratings of depression on the Hamilton depression scale.
PTSD, Aggression, Hostility, and Impulsivity
Aggression, hostility, and impulsivity have been associated with elevated risk for suicidal behavior in borderline personality disorder
(40), major depression
(41), and PTSD
(16,
42–44). In the current study group, measures of lifetime aggression were not higher in lifetime PTSD subjects, suggesting that major depressive episode and PTSD do not have an additive effect on aggression. It is noteworthy that the levels of impulsivity and hostility were higher in the group with lifetime PTSD, while the level of aggression was not. We
(17) and others
(7) have suggested that females may be more vulnerable to PTSD than males. Most studies of the relationship between PTSD and aggression have been conducted in predominantly male cohorts of veterans
(16,
43,
44). Perhaps in this mostly female group of depressed subjects with lifetime PTSD, the presence of higher levels of impulsivity and hostility is related to the high co-occurrence of cluster B personality disorder and a childhood history of abuse. The absence of an effect on aggression may be related to the low numbers of male subjects in the study group, as only three of the 59 subjects with lifetime PTSD and major depression were male.
Trauma History, PTSD, and Cluster B Personality Disorders
A history of childhood sexual or physical abuse is associated with suicidal behavior in borderline personality disorder patients
(45) and in the offspring of depressed parents
(46) and with high rates of self-destructive behaviors in adults with a history of sexual abuse
(47). Thus, abuse during childhood may create a later predisposition to self-mutilation and suicidal behavior
(45,
47). Childhood sexual and/or physical abuse has also been thought to have long-term sequelae in terms of other psychological as well as biological effects (see reference
48 for a review). For example, some
(49) have characterized borderline personality disorder as a chronic form of PTSD stemming from early childhood abuse. Others suggest significant, but not complete, overlap of these two disorders and report that more than one-half (55%) of borderline personality disorder patients carry a diagnosis of PTSD
(50). In the current group of patients with a lifetime history of major depressive episode, 35% of the patients with lifetime PTSD had comorbid cluster B personality disorder, compared to 20% of the patients with no PTSD. The contribution of childhood trauma to the development of PTSD and cluster B personality disorder and to their frequent co-occurrence is as yet unclear. Zlotnick et al.
(51) found that women with PTSD, both with and without comorbid borderline personality disorder, had higher levels of childhood trauma than women with borderline personality disorder only, suggesting that childhood trauma is more closely associated with the development of PTSD than with the development of borderline personality disorder. This interpretation is supported by another report in which childhood trauma emerged as a risk factor for PTSD, independent of the type of comorbid personality disorder
(39). In this cohort, we found that in addition to having greater comorbidity with cluster B personality disorder, patients with comorbid PTSD were also significantly more likely to report a history of childhood physical or sexual abuse.
Cluster B personality disorders, particularly borderline personality disorder, are a risk factor for suicidal behavior in depressed patients
(45,
52,
53), even when the patients do not meet the full criteria for a cluster B personality disorder
(54). Moreover, borderline personality disorder has been reported to have an additive effect with respect to suicidal behavior when it is comorbid with PTSD. In a nondepressed group of subjects, Zlotnick et al.
(51) found that patients with borderline personality disorder or with comorbid borderline personality disorder and PTSD scored higher on measures of suicide proneness than those with PTSD only. Perhaps childhood abuse increases the liability for PTSD in the face of later traumatic events, but it is comorbidity with borderline personality disorder that elevates the risk for suicidal behavior in those with PTSD.
In contrast with our previous report, the results of the current multivariate analysis, in which cluster B personality disorder is a significant contributor to suicide attempt status, support a role for cluster B personality disorder, but not PTSD directly, in higher risk for suicidal behavior. The findings from this study suggest that the increased liability for suicidal behavior that comorbid PTSD confers is mediated by the frequency of cluster B personality disorder comorbidity. In support of this notion, Heffernan and Cloitre
(55) found that women with a history of childhood abuse who had both PTSD and borderline personality disorder were more likely to engage in suicidal behavior than those with PTSD alone. Our study design did not permit tracking of the patterns and timing of onset of comorbid disorders and major depressive episode; however, it did show that, generally, the onset of PTSD antedated the first suicide attempt and that both occurred later than the reported childhood abuse. One possible explanation for our findings is that although trauma in childhood increases vulnerability to both PTSD and cluster B personality disorder, it is this latter condition that elevates the risk for suicidal behavior, possibly mediated through other associated disturbances in cluster B personality disorder that are not directly linked to childhood trauma. To dissect this relationship, prospective studies that attend to the sequence of onset of the disorders are required.
Conclusions
PTSD is frequently comorbid with major depressive disorder, and when the two disorders co-occur, the risk for suicidal behavior is enhanced. The relationship between PTSD and suicidal behavior appears to be mediated by the presence of cluster B personality disorder, with both PTSD and cluster B personality disorder arising as a result of earlier traumatic experiences. The assessment and treatment of comorbid conditions such as PTSD and cluster B personality disorder in the context of major depressive disorder are likely to contribute to the reduction of suicide risk in this vulnerable population.