Studies have indicated a potential role for a familial factor in the etiology of suicidality
(1–
4). However, psychopathology, arguably the strongest predictor of suicide, also clusters in families, and the nature of the relationship between these two factors remains unclear. Familial aggregation of mental illness and familial aggregation of suicide are not entirely causally related
(5–
9), and family studies in adolescents have shown that even after adjustment for psychopathology, relatives of completers and attempters have higher rates of suicidal behavior than comparison subjects
(10,
11). Further studies have suggested a role for impulsive aggression in families of mood-disordered suicide attempters and nonattempters
(12,
13). However, these results have yet to be confirmed in unselected suicides.
Here we report preliminary results on a family study that confirms the familial transmission of suicidal behavior independently of psychopathology in the first- and second-degree relatives of adult male suicide completers from the general population. Our results also suggest the importance of the severity of suicidal ideation and aggression in the familial transmission of suicidality.
Method
The subjects for this study were 25 male suicide completers who were randomly selected over a 3-year period from the general population of Montreal and 25 age- and gender-matched comparison subjects. The suicide completers were identified through a collaborative agreement with the Quebec Coroner’s Office, and family members appearing at the morgue were invited to participate in the study.
Community comparison subjects were recruited with the best-acquaintance method, whereby comparison subjects were randomly selected from five friends of the deceased. For cases in which no matched friend was available, the recruitment of comparison subjects was done by local advertisement. Comparison subjects were excluded if they had a history of a major axis I disorder. This study was approved by our local institutional review board, and written informed consent was obtained from participating family members after the study had been fully explained.
Consensus psychiatric diagnoses for probands were made by means of the psychological autopsy method with DSM-IV criteria
(14). Structured interviews were carried out by trained clinicians with informants best acquainted with the subject by using modified Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) interviews, including questions from the Interview Schedule for Children to assess personality disorders
(15). To assess how K-SADS interviews would compare to Structured Clinical Interviews for DSM-IV in this adult population, 15 subjects were randomly assessed with both instruments. Agreement for major psychiatric diagnoses was 100%. Procedural details and reasons for using the K-SADS in this particular population are discussed elsewhere
(16,
17). Interrater reliability for diagnoses was estimated in a subgroup of subjects, and kappa coefficients for key psychopathology were above 0.80 (16).
Psychopathology of relatives was assessed through administration of the Family Interview for Genetic Studies
(18). Suicidal behavior and suicidal ideation (the latter was obtained with an adapted version of the Scale of Suicide Ideation
[19] providing a measure of current ideation) were assessed directly with relatives. Relatives were all first- and second-degree relatives of suicide completers and comparison subjects who either were directly assessed for suicidality (suicides, 55.9%; comparison subjects: 53.2%) and/or were described by an informant during the course of the Family Interview for Genetic Studies. Variables were defined according to information obtained through the Family Interview for Genetic Studies and were assessed by the same rater (C.D.K.). “Aggression” was defined as a lifetime history of repeated instances of verbal or physical aggression toward others and was analyzed as a dichotomous variable. “Suicidal behavior” in the analysis included attempts and completions but not ideation.
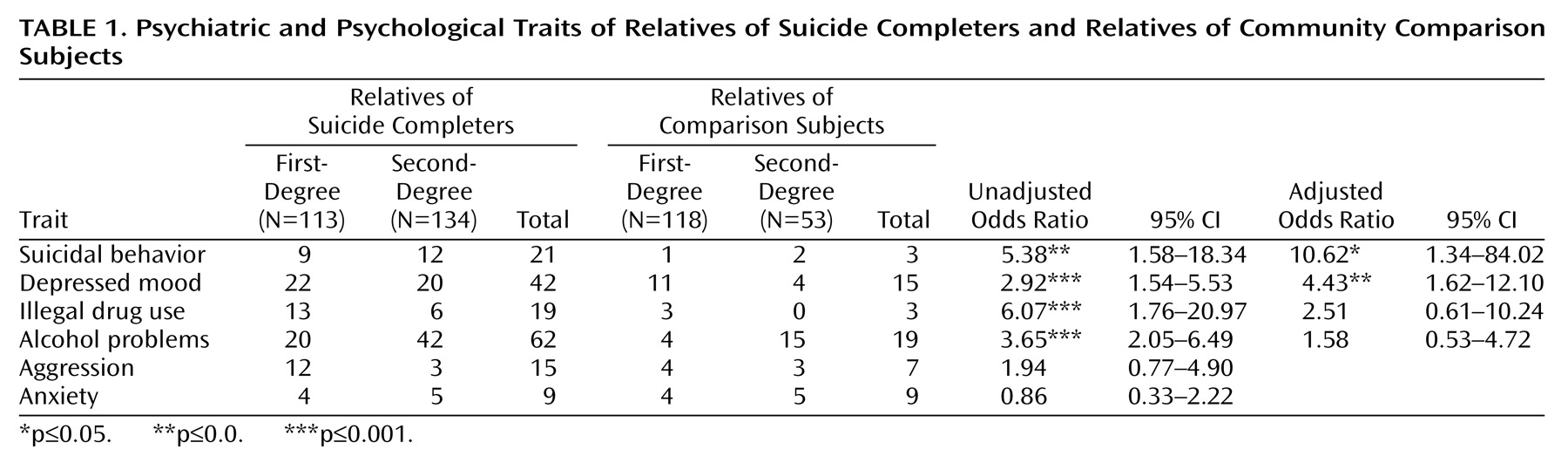
Univariate analyses were carried out using standard tests. Adjusted odds ratios were calculated with logistic regression. Variables included in the regression analysis were depressed mood, alcohol misuse, illegal drug use, and family history of suicidal behavior. Differences between first- and second-degree relatives were controlled for through inclusion of degree of relation in the analysis.
Results
All probands were male. The completers and comparison subjects were not significantly different in age, marital status, or household revenue. More completers were receiving welfare than comparison subjects (20% versus 0%) (p=0.04, Fisher’s exact test), and the completers had lower levels of education than the comparison subjects, with a higher proportion of the comparison subjects (92%) having completed high school in relation to the suicide completers (72%).
Eighty percent of the suicide completers were diagnosed with a major axis I disorder (44% with alcohol abuse or dependence, 40% with depressive disorder, and 24% with drug abuse or dependence); 56% were diagnosed with an axis II personality disorder (4% cluster A, 52% cluster B). Four percent of the comparison probands were diagnosed with an axis II disorder.
The relatives of the suicide completers had a mean age of 46.76 years (SD=16.28) compared with the relatives of the comparison subjects, who had a mean age of 46.48 years (SD=18.29). The relatives of the suicide completers and the relatives of comparison subjects were not significantly different in age. The relatives also were not significantly different in gender or in the prevalence of physical problems/prolonged illness. However, the relatives of the suicide completers were significantly more likely to be deceased than the relatives of the comparison subjects (17.8% versus 9.9%) (χ2=5.1, df=1, p<0.05). The relatives of the suicide completers had a nonsignificantly higher frequency of criminal histories (2.8% versus 1.2%) and sexual abuse (2.0% versus 0%) than the relatives of the comparison subjects.
History of depressed mood, illegal drug use, and alcohol problems were all significantly more likely to occur in the relatives of suicide completers than in the relatives of the comparison subjects. There was a significant difference in the presence of aggressive behavior in the first-degree relatives (odds ratio=3.97, 95% confidence interval [CI]=1.23–12.80; p<0.02). When the first- and second-degree relatives were considered, the effect was less intense, with a nonsignificant tendency for aggressive behavior in the relatives of suicide completers (6.1%) in relation to the comparison subjects (4.1%). Other Family Interview for Genetic Studies personality and psychiatric traits are shown in
Table 1.
A total of 227 relatives were directly assessed for suicidal behavior and ideation (relatives of the suicide completers=132, relatives of the comparison subjects=95). The relatives of the suicide completers and the relatives of the comparison subjects were not significantly different for past or present suicidal ideation (odds ratio=2.08, 95% CI=0.98–4.42). However, the relatives of the suicide completers had significantly higher suicidal ideation scores than the relatives of the comparison subjects (t=–2.69, df=225, p=0.008).
Previous work in our group has suggested that suicide completers can be divided into subgroups according to psychopathology, most notably by the conditions characterized by impulsive and aggressive traits
(17). Thus, a subgroup of suicide completers with cluster B disorders was compared to the comparison group. Thirteen suicide completers were diagnosed with cluster B personality disorders.
Aggression in the first-degree relatives of cluster B completers was significantly higher in relation to the relatives of comparison subjects (odds ratio=5.43, 95% CI=1.62–18.19; p<0.006). When all relatives were considered, the tendency remained, although it became nonsignificant (7.6% of the relatives of cluster B completers versus 4.1% of the relatives of the comparison subjects). The adjusted odds ratio for the effect of family history on suicidal behavior was 14.84 (95% CI=1.82–120.81; p<0.05). Depressed mood had an adjusted odds ratio of 4.90 (95% CI=1.55–15.46; p≤0.01). Neither alcohol problems (odds ratio=1.15, 95% CI=0.32–4.10) nor illegal drug use (odds ratio=4.01, 95% CI=0.85–18.88) remained significant in the logistic regression model.
Discussion
We found that a family history of suicide remains a significant predictor of suicidal behavior even when psychopathology is taken into account and that aggression is significantly higher among the first-degree relatives of suicide completers than among the relatives of comparison subjects. When we looked at a subgroup of suicide completers with cluster B personality disorders, we found that the effect of family history in predicting suicidal behavior was strengthened both in intensity and in significance, as was aggression in first-degree relatives. The latter finding is interesting, as previous studies have found that higher
proband aggression is associated with higher familial suicidal behavior in adolescent completers
(10).
We also found that the occurrence of suicidal ideation is not significantly different between the relatives of completers versus the relatives of comparison subjects. However, we found that the relatives of completers have higher
levels of ideation than do the relatives of comparison subjects, suggesting that it is the severity rather than the presence of suicidal ideation that may be part of the liability toward suicide transmitted in families. This is consistent with models proposed to understand the predisposition to suicide
(20).
Of interest, the relatives of suicide completers—in both the large group and the subgroup—were more likely to be deceased than the relatives of comparison subjects, even though the relatives were not different in age, gender, or the presence of physical or prolonged illness. It is possible that the relatives of suicide completers are engaged in activities or behaviors that put them at a higher risk for death. However, this should be confirmed and further investigated.
Nonsignificantly higher rates of criminal behavior and sexual abuse were found in relatives of both groups of suicide completers. This is consistent with previous studies linking suicidality with criminal behavior
(21) or a history of childhood sexual abuse
(12). The lack of significance of these tendencies may be due to the power limitations of our study. Further work would benefit from more thorough assessment of cluster B personality disorders and aggressive traits.
In conclusion, we have confirmed that suicidal behavior has a strong familial component and that this family effect is particularly high in the relatives of suicide completers with cluster B personality disorders. Our results further suggest the possibility that aggressive behavior together with severe suicidal ideation may be factors in the familial transmission of suicidal behavior.