Suicide and suicide attempts are risks of the major psychiatric illnesses, with mortality rates markedly higher than for the general population
(1). A lifetime risk of 15% for suicide was the conclusion of a meta-analysis of hospitalized patients by Guze and Robins
(2). A reanalysis of studies of suicide in affective illness in three groups of patients—outpatients, inpatients, and suicidal patients—found a risk of those ever hospitalized of 8.6%
(3). Other studies confirmed the risk of suicide to be particularly high in hospitalized depressed patients
(4–
6). Profound hopelessness, hypochondriacal ruminations or delusions, and thoughts of suicide or self-harm during depression predict future suicide
(7).
Antidepressant medications are the principal agents used to treat affective disorders today. Their impact on suicide risk is not well defined, however, and they are generally viewed as less effective than ECT in relieving depression and suicidal thoughts. Hordern et al.
(8) reported no suicides at the 6-month follow-up in 34 women treated with ECT but found two in the 84 patients treated with antidepressants (2.4%). Avery and Winokur
(9) assessed suicidal behavior in the 6 months following the treatment of depression in 519 patients. Suicide attempts were recorded in 0.8% of the ECT patients compared to 4.2% of those who had received “adequate” and 7% “inadequate” antidepressant medication treatment. Khan et al.
(10) found antidepressant drugs to be no more effective than placebo in reducing suicide rates in seriously ill depressed patients.
The experience with ECT is also unclear. A comparison of the frequency of suicides in different decades found decreased rates when ECT was the dominant treatment for mental illness
(11). An examination of the records of 1,397 completed suicides in Finland within a 12-month period showed only two patients having received ECT
(12). In another report, Sharma
(13) identified 45 psychiatric inpatients in a Canadian provincial hospital who committed suicide and compared their records with an equal number of patients matched for gender, age, and admission diagnosis
(13). He reported no difference in ECT use in the two samples, finding no particular benefit for ECT.
Prudic and Sackeim
(14) examined the changes in item 3 (expressed suicidal intent) of the Hamilton Depression Rating Scale in 148 patients referred for ECT. Both suicide and mortality rates were reduced with treatment. The overall average score on item 3 was 1.8 at baseline and was reduced to 0.1 in 72 responders and to 0.9 in 76 nonresponders. For the total sample, there was a greater decrease in the suicide item scores than the overall Hamilton depression scale scores.
National psychiatric associations in Great Britain and the United States
(15,
16) and recent assessments by the Canadian Agence d’Évaluation des Technologies et des Modes d’Intervention en Santé
(17) and the U.K. National Institute for Clinical Excellence
(18) cited the reduction of suicide risk as a justification for the use of ECT.
We assessed suicide risk in an ongoing collaborative multicenter study comparing the efficacy of continuation ECT with continuation pharmacotherapy in unipolar depressed patients after response to a course of ECT.
Method
Study Design
The Consortium for Research in ECT Continuation ECT Study is a multisite, collaborative study funded by the National Institute of Mental Health to compare the efficacy of continuation ECT and continuation pharmacotherapy (lithium plus nortriptyline). Patients with unipolar major depression were referred for ECT at four institutions to receive an acute course of thrice-weekly bilateral ECT sessions (acute phase)
(19). ECT is given with a standardized protocol with a Thymatron DGx device (Somatics, Inc., Lake Bluff, Ill.). The patients whose condition remits and remains remitted for 1 week without treatment are randomly assigned to receive either continuation ECT or continuation pharmacotherapy (nortriptyline plus lithium) (continuation phase). In the 6-month continuation phase, the patients receive bilateral ECT weekly for 4 weeks, biweekly for 8 weeks, and monthly for 2 months.
Depressive symptoms are assessed at baseline and three times weekly during the course of treatment (24–36 hours after each ECT session) with the 24-item Hamilton depression scale
(20). Remission in the acute phase is defined by two consecutive Hamilton depression scale ratings ≤10 and a ≥60% reduction in Hamilton depression scale total score. The reliability of these ratings was checked by a quality assurance program in which a doctoral-level psychologist reviewed and co-rated videotapes of interviews from each site. All raters participated in a co-rating of interviews at least three times a year. When ratings were not within the acceptable range, the rater participated in customized remediation sessions.
There is no prescribed minimum or maximum number of ECT sessions; however, to be declared a nonremitter, a patient must have received at least 10 ECT treatments and reached a plateau relative to the decline of Hamilton depression scale total scores, indicating no further clinical improvement. Patients who withdraw consent or for whom ECT is discontinued for clinical or other reasons before receiving 10 ECT sessions are considered dropouts.
Study Group
Patients with DSM-IV-defined major depressive disorder (major depressive disorder as assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders criteria
[21]), with age ranges of 18–85 years, who were referred for ECT and who had a minimum baseline Hamilton depression scale total scores of 21 were eligible for study inclusion. Exclusion criteria included schizophrenia, bipolar disorder, neurological illness, or illicit substance dependence within 1 year and ECT within 3 months. To date, 444 patients with unipolar major depression have entered the study, with 355 (80%) completing the acute course of ECT and 89 dropping out (20%). Reasons for dropping out during the acute phase included patient withdrawal of consent (N=37), adverse events (N=33), and protocol violations (N=19). Reasons for patient-initiated withdrawal (N=37) included concerns about cognitive effects (N=5), no perceived treatment effects (N=1), the patient perceiving that no further treatments were needed (N=5), preferred medications (N=6), wanting to go home (N=2), and no reason given
(18). Adverse events were confusion or memory problems (N=20), intercurrent medical condition (N=9), and other psychiatric illnesses (N=4). The study group was 31.8% male, 91.7% Caucasian, 29.7% with psychotic depression. The mean Hamilton depression scale score at baseline was 35.1 (SD=7.2). Demographic characteristics of the study group are representative of patients typically referred for ECT.
Acute-Phase ECT
A stimulus dose titration procedure was performed at the first treatment to determine seizure threshold, and subsequent stimulus dosing was at 1.5 times the seizure threshold. The patients were treated with a standard brief-pulse ECT device with bitemporal electrode placement.
Outcome
This report considers the change in expressed suicidal intent, as recorded in item 3 of the Hamilton depression scale. This item was scored 0=absent; 1=feels life is empty or is not worth living; 2=recurrent thoughts or wishes of death of self; 3=active suicidal thoughts, threats, gestures; and 4=serious suicide attempt. Scores of 3 and 4 were evidence of expressed suicide intent (0–2 [low suicide rating group] and 3–4 [high suicide rating group]). The primary outcome was resolution of the suicide score to 0 (score resolved to 0/did not resolve to 0). For primary analyses, those in the high suicide rating group were followed for occurrence of the primary outcome (item 3 score resolved to 0).
Statistical Analysis
Standard descriptive measures (means and standard deviations for continuous variables, proportions for categorical variables) were used to describe baseline demographic and clinical characteristics of the total study group and the high versus low suicide rating groups. Baseline characteristics were compared across the low/high suicide rating groups with either a two-sample t test (continuous variables) or a chi-square test (categorical variables). For the primary analysis, a frequency distribution describing proportion of patients in the high rating group whose suicidality scores resolved (became 0) after successive ECT treatments was determined. In additional secondary analyses, percent change in item 3 means and corresponding Hamilton depression scale total score means for the total study group after 1 week (three ECT sessions) and 2 weeks (six ECT sessions) of treatment were also determined. The statistical significance of the decline in item 3 values over the course of the first three ECT sessions (1 week of treatment) and over the course of the first six ECT sessions (within 2 weeks of treatment) was assessed with mixed-models analysis (SAS Proc Mixed with unstructured covariance [SAS Institute, Cary, N.C.]), which evaluates the longitudinal profile (e.g., slope) in repeated correlated measures over time. Characteristics of the groups whose expressed suicidal intent scores resolved (became 0) and whose scores did not resolve were described with standard descriptive methods and were compared with either a two-sample t test (continuous variables) or a chi-square test (categorical variables). In exploratory analyses, we investigated the relationship of psychosis status and age to resolution of expressed suicidal intent with logistic regression with expressed intent resolved or not resolved as the dependent variable. Psychosis status and age were considered both separately (univariate analyses) and together (multivariate analyses). Odds ratios and corresponding 95% confidence intervals (CIs) are reported from these analyses. No correction for multiple analyses was used; therefore, secondary and exploratory results must be evaluated cautiously in terms of type I error rate.
Results
The remission rate for depression in the 355 patients who completed the course of treatment was 85.6% (N=304). For the total study group (N=444) (treating dropouts as nonremitters), the remission rate was 68.5% (N=304). The average Hamilton depression scale score at baseline was 35.1 (SD=7.2) for the full group, with an average change from baseline of 24.8 (SD=10.2) for the full group and 26.9 (SD=9.1) for those who completed the acute course of ECT.
On item 3 of the Hamilton depression scale for the 444 patients referred for ECT, 118 (26.6%) received a score of 3 for having active suicidal thoughts, actions, or gestures, and 13 (2.9%) received a score of 4 for reporting a suicidal event during the current episode. The baseline means for the item 3 ratings were 1.70 (SD=1.16) for the full group, 1.64 (SD=1.18) for the 355 patients who completed the full treatment course, and 1.92 (SD=1.00) for the 89 dropouts.
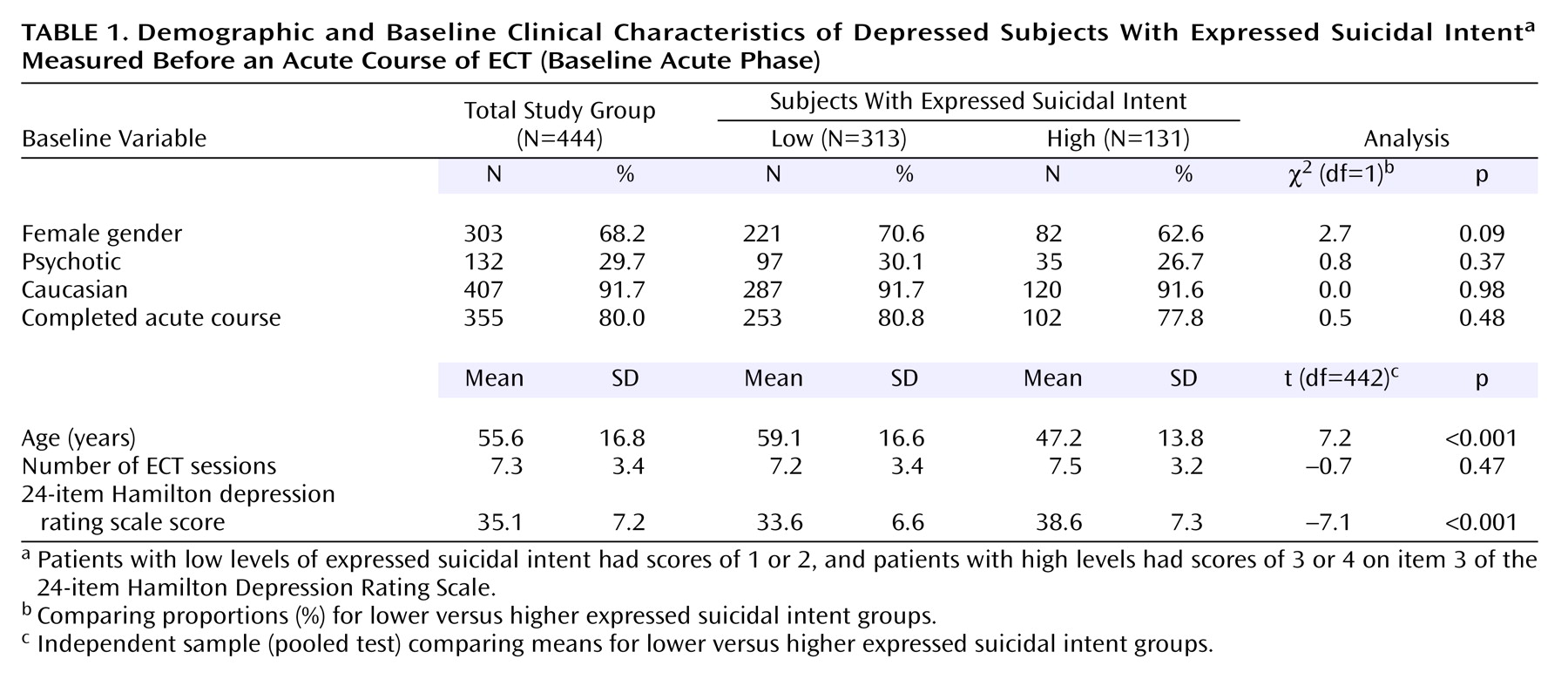
Patients in the high expressed suicidal intent group were younger, on average, than those in the low group (mean=47.2, SD=13.8, versus mean=59.1, SD=16.6) (p<0.001) (
Table 1). Although there were fewer psychotic patients and women in the high expressed suicidal intent group, the differences were not significant (p=0.37 and p=0.09, respectively) (
Table 1). There were no differences in the dropout rates for those in the high compared to the low expressed suicidal intent groups (22% versus 19%) (χ
2=0.51, df=1, p=0.48).
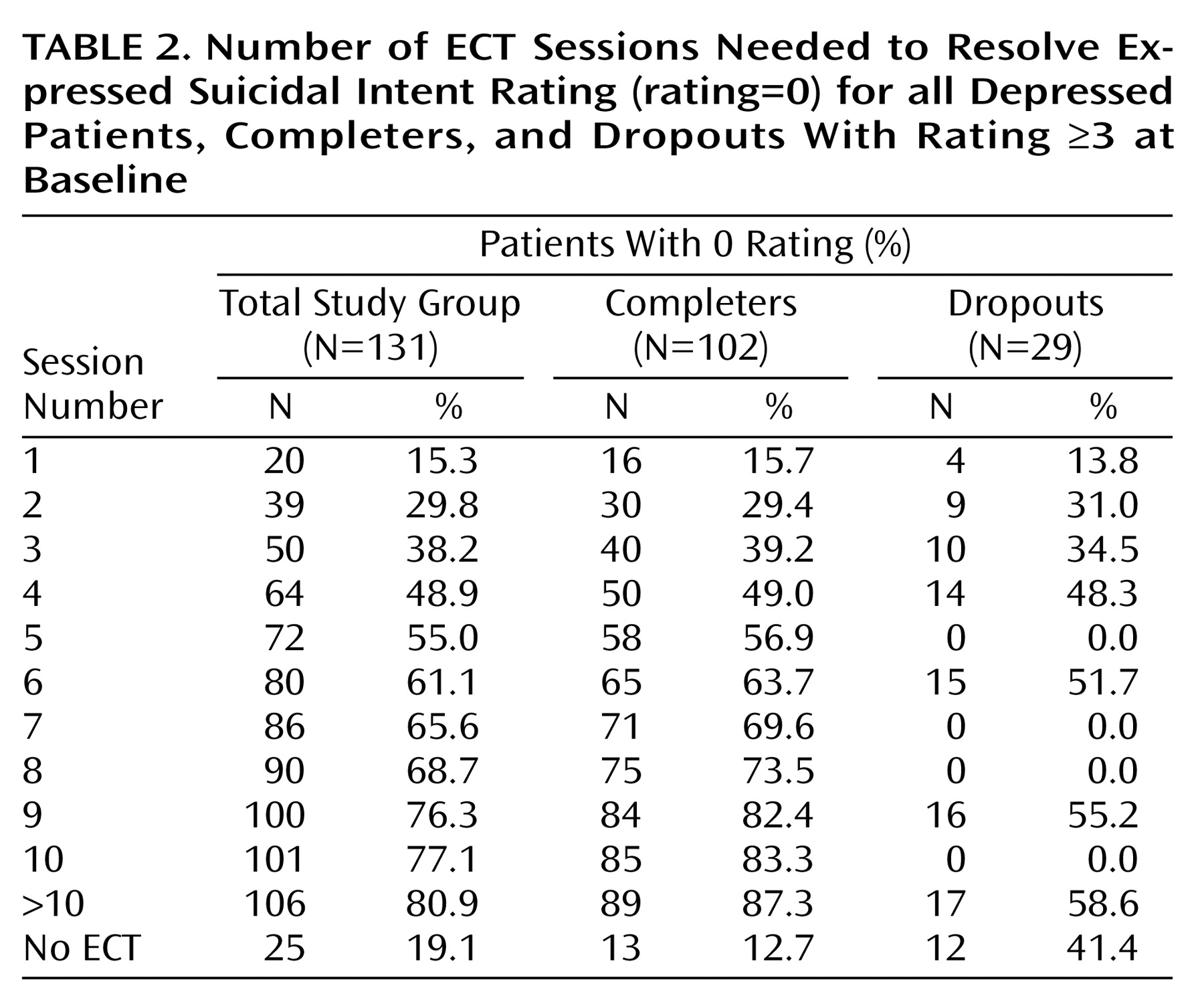
Of the 131 patients in the high expressed suicidal intent group, the rating of 106 patients (80.9%) ultimately dropped to 0. This occurred in 15.3% (N=20) after one ECT session; in 38.2% (N=50) after three ECT sessions (1 week); in 61.1% (N=80) after six ECT sessions (2 weeks); and in 76.3% (N=100) after nine ECT sessions (3 weeks) (
Table 2). Among 102 patients in the high expressed suicidal intent group who completed the acute course of ECT, 87.3% (N=89) had their scores drop to 0 by the end of the treatment course, with approximately 63.7% reaching resolution after six ECT sessions (within 2 weeks). For the 13 patients with a rating of 4 (suicide attempt) at baseline, all saw their ratings drop to 0 by the end of their treatment.
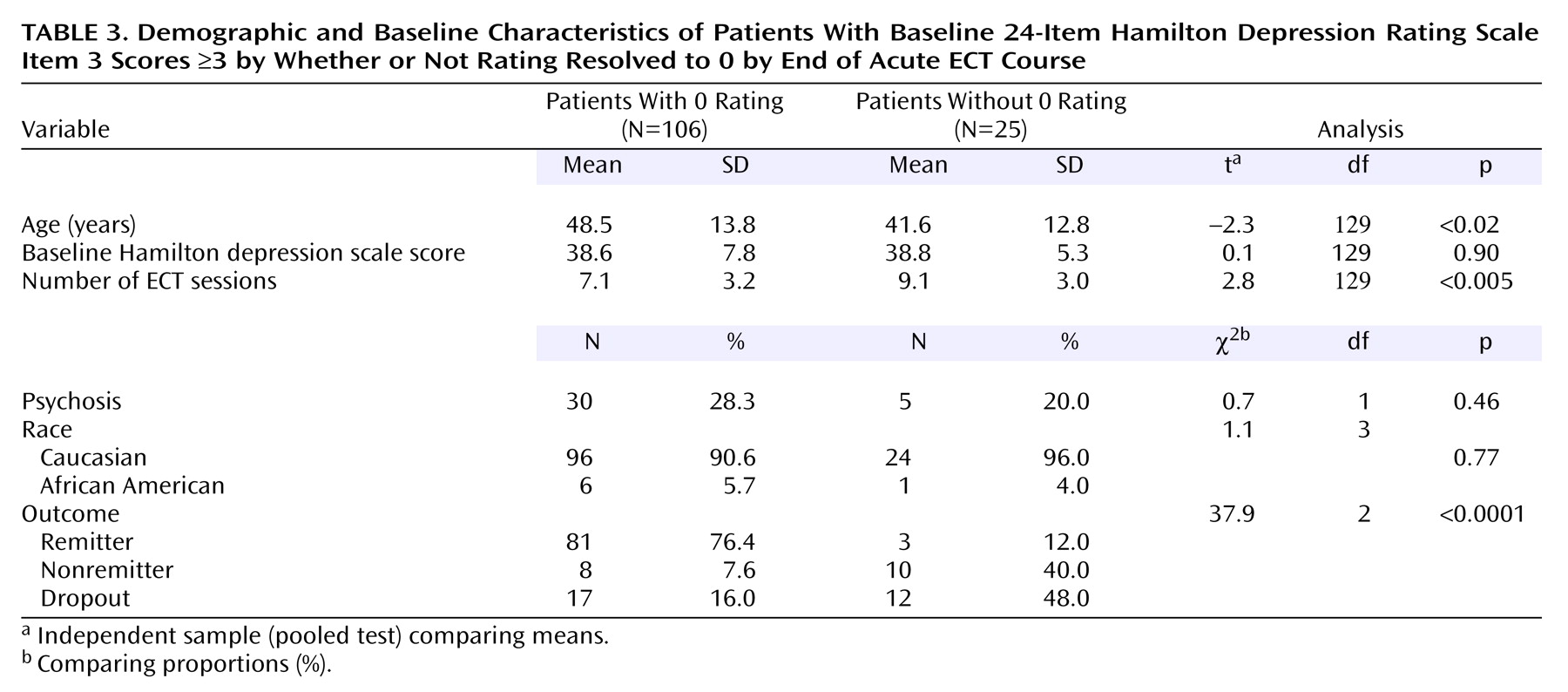
Among the 25 patients in the high expressed suicidal intent group whose ratings did not resolve to 0, 48% (N=12) dropped out before receiving an adequate course of treatment and, of the remaining 13 patients, 46% (N=6) had a rating of 1 at the end of the acute course. Over half (N=7) of the 13 patients rated 0 during the treatment course but did not retain it at the final rating. The patients whose expressed suicide intent ratings did not resolve were younger than those whose ratings resolved (t=–2.3, df=129, p<0.02) but were not different with respect to percent with psychosis or baseline severity of illness (
Table 3).
After six ECT sessions (2 weeks), 66% (N=35) of 53 older patients (≥50 years) had expressed suicidal intent scores of 0 compared to 58% (N=45) of 78 younger (<50 years) patients; 89% (N=47) of the older group eventually reached ratings of 0 compared to 76% (N=59) of the younger group. The odds of having the expressed suicide intent rating resolve to 0 was 2.5 times higher for the older compared to the younger group (odds ratio=2.5, 95% confidence interval=0.9–6.8). When we treated age as a continuous variable in the logistic regression model, there was a significant relationship between the outcome (expressed suicidal intent rating resolved or did not resolve) and age (p<0.03).
At baseline, the correlation between item 3 ratings and Hamilton depression scale total score was –0.01 (Pearson correlation, p=0.87) among the group in the high rating category. The correlation between change from baseline for the item 3 rating and Hamilton depression scale total score was 0.45 (Pearson correlation, p<0.001) for this group. Within the first week of treatment (three ECT sessions), the average percent reduction from baseline in item 3 scores for the total study group was 56% compared to a relative change of 52% for the Hamilton depression scale total score. After 2 weeks of treatment (six ECT sessions), the expressed suicide intent rating item had a relative reduction from baseline of 78% (75% for Hamilton depression scale total score).
Two patients died by suicide in the course of the study, one each at different sites. Both were white men, 76 and 80 years of age, and were diagnosed with a major depressive disorder without psychosis. At the outset, one patient had a Hamilton depression scale of 29 with an expressed intent that was scored 1 on item 3. He received seven ECT sessions and ended the course with a Hamilton depression scale score of 8 and a score of 0 on item 3. He was in the 1-week interim phase awaiting random assignment, and on day 6 after the last ECT session, he died by gunshot wound. The second patient had a baseline Hamilton depression scale score of 22 and expressed no suicidal intent, scoring 0 on item 3. After 10 ECT sessions, his Hamilton depression scale score was 8, and 1 week later, he was randomly assigned to receive continuation ECT. Two weeks later, after the second continuation ECT session (Hamilton depression scale score of 16 and item 3 score of 2), he successfully overdosed with medications.
Discussion
These data, from a large group of severely depressed patients, most of whom were hospitalized, document a rapid reduction in expressed suicidal intent in patients treated with ECT. The patients were referred at four geographically dispersed academic medical centers and are typical of depressed patients who receive ECT after extensive medication and psychotherapy trials. Expressed suicidal intent, as reflected in scores of 3 and 4 on item 3 of the Hamilton depression rating scale, was present in 29.5% of the treatment group of 444. This incidence of expressed suicidal intent is considerably larger than in the usual populations treated with medications
(22).
Two of 444 patients died by suicide, both in the follow-up period after the index ECT course and both on outpatient status. We find the benefits of ECT to be immediate, but they may not persist unless treatment is sustained, a conclusion also reached by others
(11,
14). More intensive and extensive treatment is needed to consolidate the benefits of antidepressant treatment.
Suicide risk is high after discharge from hospital care for depression. In a study of depressed patients at 3 months, 1 year, and 2 years after admission, Oquendo et al.
(23) reported that the persistence of major depression in the follow-up period increased the risk of a suicide attempt sevenfold. Antidepressant treatment in the follow-up period was largely inadequate, and patients with a prior suicide attempt did not receive more vigorous care than nonattempters. For each suicide attempt in the subject’s history, the risk for an attempt in the follow-up period increased by 30%.
Two cohort studies also reported higher suicide rates in depressed patients immediately after hospital discharge
(24,
25). A third study did not find an association
(26). The author noted “that no specific diagnosis seems to stand out suggest[ing] that an improvement in the quality of care for all discharged patients is necessary to reduce suicide rates.” We would add that effective remission of mood disorder and psychosis should reduce the incidence of suicide after hospital discharge.
These observations are relevant to the development of treatment algorithms for major depressive illness. Our present treatment algorithms do not reflect the efficacy of ECT
(27). They offer treatments of lesser, and even some unproven, efficacy before recommending ECT, which is usually cited as the “last resort.” Such approaches are justified by the controversial nature of ECT, the reluctance of patients to accept it without having tried all other treatment courses, and the unavailability of ECT at major treatment centers. Indeed, in some states, notably California and Texas, the last resort option is codified into law
(28,
29). Whatever the objections to the use of ECT may be, the present data on the rapid resolution of expressed suicidal intent warrant greater attention in evidence-based treatment algorithms.
Just as it has been advantageous to dichotomize depressive patients as to the presence of psychosis, offering different treatment options for the two groups, it may be advantageous to dichotomize patients at risk of suicide. For those at high suicide risk or with recent suicide attempts, especially those who appear so suicidal as to require continuing observation, ECT should be considered early in the algorithm.
The presence of psychosis in depression is an additional risk factor for suicide. Roose et al.
(4) retrospectively studied 22 suicides in patients with major affective disorders. Their 14 patients with delusional unipolar depression were 5.3 times as likely to complete suicide as their unipolar depressed patients without delusions. Patients with psychotic depression respond better and more rapidly to real rather than sham ECT
(30,
31). They also respond more rapidly and better than nonpsychotic depressed patients to ECT
(19,
32).
A limitation of the current study was the use of a single item to assess a behavior as complex as expressed suicidal intent. And, in the absence of a concurrent comparison group, we depend on historical comparisons with antidepressant medications.
Advantages of the current study include the large group, multiple sites, standardized single treatment, well-trained raters, rigorous nature of the assessments, and the limitations in variability of additional medications and rescue treatments, thereby defining a rigorous study group with homogeneous treatment characteristics. The use of bilateral electrode placement, the monitoring of the EEG of each treatment to ensure adequate treatments, and the use of standardized dosing schedules helped to improve treatment outcome.
More and more emphasis is being placed on outcomes in psychiatric practice. The most recent large-scale meta-analysis of the efficacy and safety of ECT in depressive disorders reports real ECT to be more effective than simulated ECT and more effective than pharmacotherapy
(33). The authors conclude, “There is a reasonable evidence base for the use of ECT; it does not rest simply on anecdote, habit, and tradition.…ECT remains an important treatment option for the management of severe depression.” Indeed, a recent report on the quality of health care delivered to adults in the United States
(34) finds a disturbing failure of patients to get the recommended medical treatment for their illness almost half the time. The efficacy of ECT in treating depression is largely ignored in treatment algorithms, limiting the chance that severely ill, depressed patients will get an available effective treatment.
The profession often cites suicide risk as a justification for ECT
(15,
17). The present study encourages earlier consideration of ECT in the course of the treatment of severely depressed patients than is presently offered in the professional literature.
Conclusions
Considering the risk of suicide and the delayed efficacy of medications in severely depressed patients, the present practice of recommending ECT as a last resort in expert treatment algorithms unnecessarily puts suicidal psychiatrically ill patients at substantial risk
(23,
35). The common recommendation that medication be offered patients with severe depression, regardless of the symptom of expressed suicidal intent, is not justified. It is prudent to consider differentiating treatment options on a measure of expressed suicide intent.