Psychotic Experiences and Psychotic Disorders at Age 18 in Relation to Psychotic Experiences at Age 12 in a Longitudinal Population-Based Cohort Study
Abstract
Objective
Method
Results
Conclusions
Method
Sample
Measures
Psychotic experiences at age 18.
Reliability.
Psychotic disorders and at-risk mental states at age 18.
Psychotic experiences at age 12.
Sociodemographic characteristics.
Statistical Analysis
Results
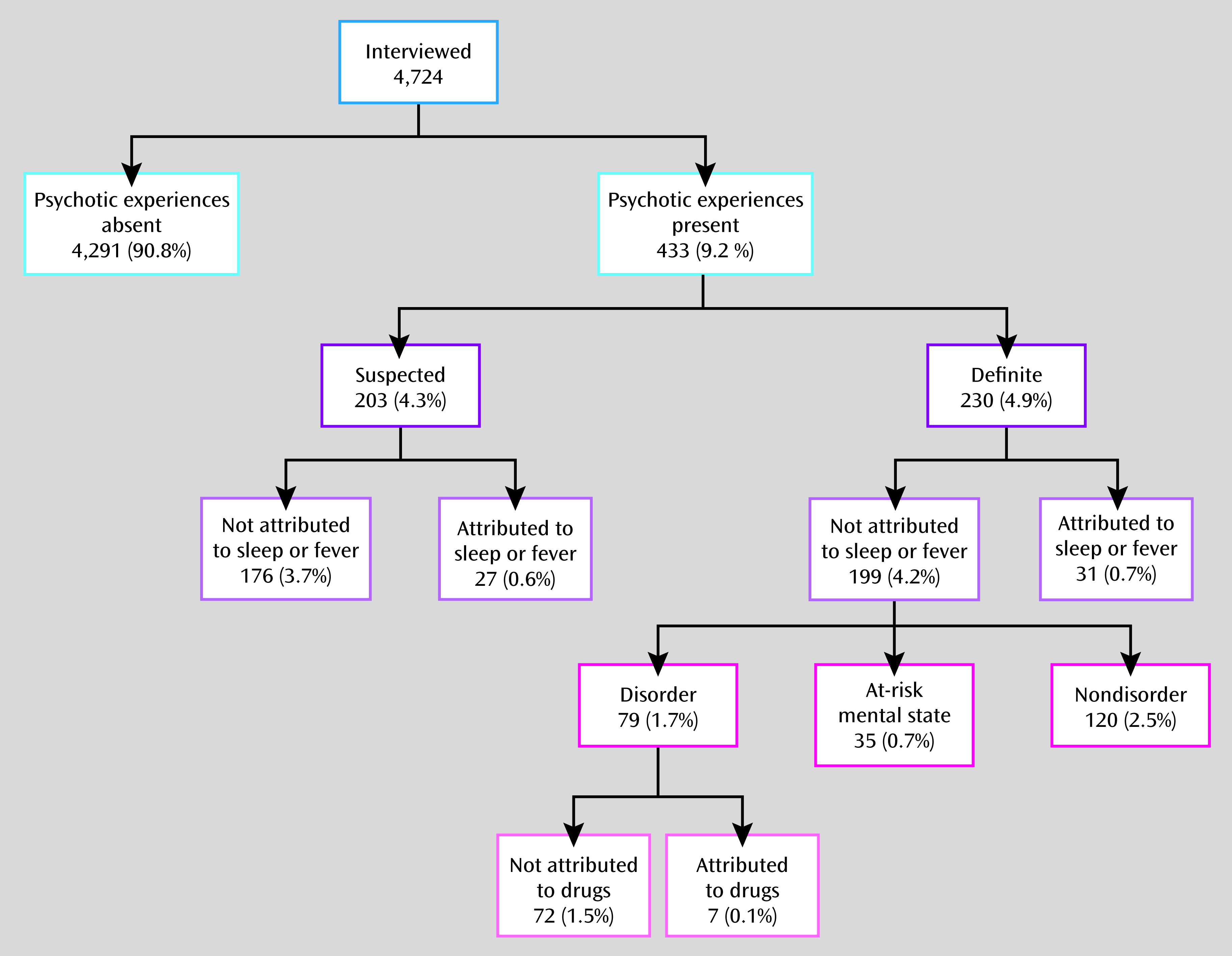
Psychotic Experiences at Age 18
| Psychotic Experiences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None | Suspected | Definite | Anya | Analysis | ||||||
| Characteristic | N | % | N | % | N | % | N | % | Odds Ratio | 95% CI |
| Sex | ||||||||||
| Male | 1,897 | 92.5 | 83 | 4.1 | 71 | 3.5 | 154 | 7.5 | 1.0 | |
| Female | 2,390 | 89.6 | 120 | 4.5 | 159 | 6.0 | 279 | 10.5 | 1.4 | 1.2–1.8 |
| Social classb | ||||||||||
| I | 694 | 92.9 | 27 | 3.6 | 26 | 3.5 | 53 | 7.1 | 0.6 | 0.4–0.9 |
| II | 1,748 | 92.5 | 65 | 3.4 | 76 | 4.0 | 141 | 7.5 | 0.6 | 0.5–0.8 |
| III | 1,175 | 89.0 | 70 | 5.3 | 75 | 5.7 | 145 | 11.0 | 1.0 | |
| IV | 121 | 85.8 | 8 | 5.7 | 12 | 8.5 | 20 | 14.2 | 1.3 | 0.8–2.2 |
| V | 17 | 81.0 | 2 | 9.5 | 2 | 9.5 | 4 | 19.1 | 1.9 | 0.6–5.7 |
| Housing | ||||||||||
| Own/mortgaged | 3,355 | 91.9 | 148 | 4.1 | 146 | 4.0 | 294 | 8.1 | 1.0 | |
| Council rent | 287 | 82.5 | 26 | 7.5 | 35 | 10.1 | 61 | 17.5 | 2.4 | 1.8–3.3 |
| Private rent | 164 | 85.4 | 8 | 4.2 | 20 | 10.4 | 28 | 14.6 | 1.9 | 1.3–3.0 |
| Other | 117 | 94.4 | 2 | 1.6 | 5 | 4.0 | 7 | 5.7 | 0.7 | 0.3–1.5 |
| Maternal partner status | ||||||||||
| Husband | 3,309 | 92.2 | 134 | 3.7 | 148 | 4.1 | 282 | 7.9 | 1.0 | |
| Partner | 611 | 85.9 | 43 | 6.1 | 57 | 8.0 | 100 | 14.1 | 1.9 | 1.5–2.5 |
| None | 47 | 78.3 | 8 | 13.3 | 5 | 8.3 | 13 | 21.7 | 3.2 | 1.7–6.1 |
| Income support | ||||||||||
| No | 3,638 | 91.9 | 155 | 3.9 | 168 | 4.2 | 323 | 8.2 | 1.0 | |
| Yes | 197 | 79.8 | 20 | 8.1 | 30 | 12.2 | 50 | 20.2 | 2.9 | 2.1–4.0 |
| Parental educationb | ||||||||||
| Certificate of Secondary Education/vocational | 422 | 85.8 | 32 | 6.5 | 38 | 7.7 | 70 | 14.2 | 2.0 | 1.5–2.8 |
| Ordinary level | 1,019 | 89.6 | 52 | 4.6 | 66 | 5.8 | 118 | 10.4 | 1.4 | 1.1–1.8 |
| Advanced level | 1,349 | 92.4 | 53 | 3.6 | 58 | 4.0 | 111 | 7.6 | 1.0 | |
| Degree | 1,164 | 92.3 | 47 | 3.7 | 50 | 4.0 | 97 | 7.7 | 1.0 | 0.8–1.3 |
Continuity of Psychotic Experiences From Age 12 to Age 18
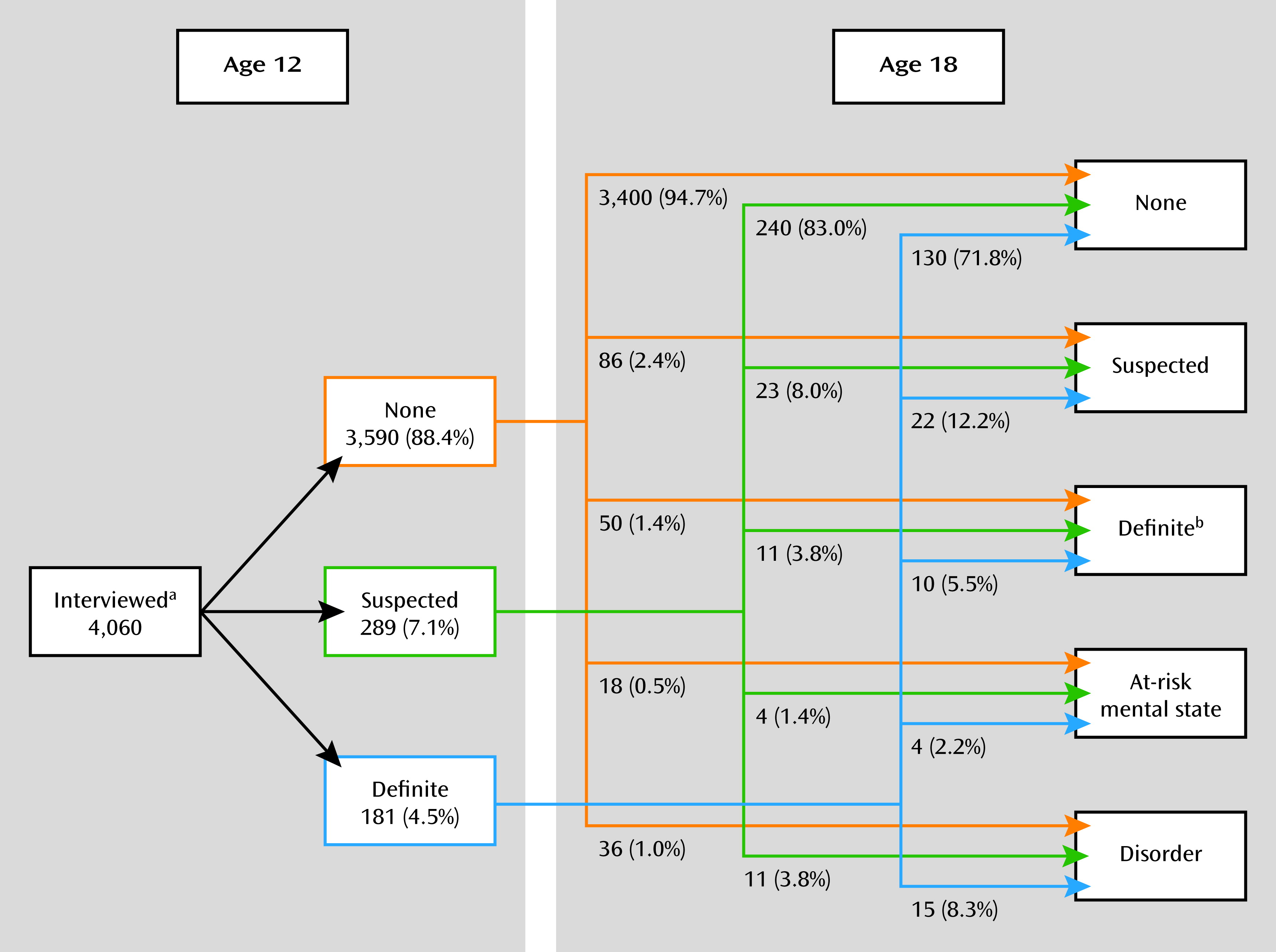
Psychotic Disorders at Age 18
Prediction of Psychotic Disorders at Age 18
| Definite Psychotic Experience at Age 18 | Psychotic Disorders at Age 18 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 12 Experiencesa | Total | N | % | Odds Ratio | 95% CI | p | N | % | Odds Ratio | 95% CI | p |
| None | 2,264 | 38 | 1.7 | 1.0 | 16 | 0.7 | 1.0 | ||||
| Self-reported psychotic-like experience (rated absent by interviewer) | 828 | 33 | 4.0 | 2.4 | 1.5–3.9 | <0.001 | 7 | 0.9 | 1.2 | 0.5–2.9 | 0.691 |
| Interviewer-rated unusual experience | 423 | 21 | 5.0 | 3.1 | 1.8–5.3 | <0.001 | 10 | 2.4 | 3.4 | 1.5–7.5 | 0.003 |
| Interviewer-rated psychotic experiences attributed to sleep/feverb | 75 | 8 | 10.7 | 7.0 | 3.1–15.6 | <0.001 | 3 | 4.0 | 5.9 | 1.7–20.5 | 0.006 |
| Interviewer-rated suspected psychotic experience (not attributed) | 289 | 26 | 9.0 | 5.8 | 3.5–9.7 | <0.001 | 11 | 3.8 | 5.6 | 2.6–12.1 | <0.001 |
| Interviewer-rated definite psychotic experience (not attributed) | 181 | 28 | 15.5 | 10.7 | 6.4–17.9 | <0.001 | 15 | 8.3 | 12.7 | 6.2–26.1 | <0.001 |
| Psychotic Disorders at Age 18 | ||||||
|---|---|---|---|---|---|---|
| Age 12 Psychotic Experiences | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI | Positive Predictive Value | 95% CI |
| Definite (not attributed) | 24.2 | 22.9–25.5 | 95.9 | 95.2–96.4 | 8.3 | 7.4–9.1 |
| Suspected or definite (not attributed) | 41.9 | 40.4–43.5 | 88.9 | 87.9–89.9 | 5.5 | 4.8–6.2 |
| Any suspected or definite | 46.8 | 45.2–48.3 | 87.1 | 86.0–88.1 | 5.3 | 4.6–6.0 |
| Any suspected or definite psychotic or unusual experience | 62.9 | 61.4–64.4 | 76.8 | 75.4–78.1 | 4.0 | 3.4–4.6 |
| Any self-reported experiencesa | 74.2 | 72.9–75.5 | 56.2 | 54.7–57.8 | 2.6 | 2.1–3.1 |
At-Risk Mental States
Multiple Imputation
Discussion
Psychotic Outcomes at Age 18
Clinical Characteristics
Prediction of Psychosis
Implications of Identifying High-Risk Individuals
Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 213.33 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

