Psychological Interventions for Psychosis: A Meta-Analysis of Comparative Outcome Studies
Abstract
Objective
Method
Results
Conclusions
Method
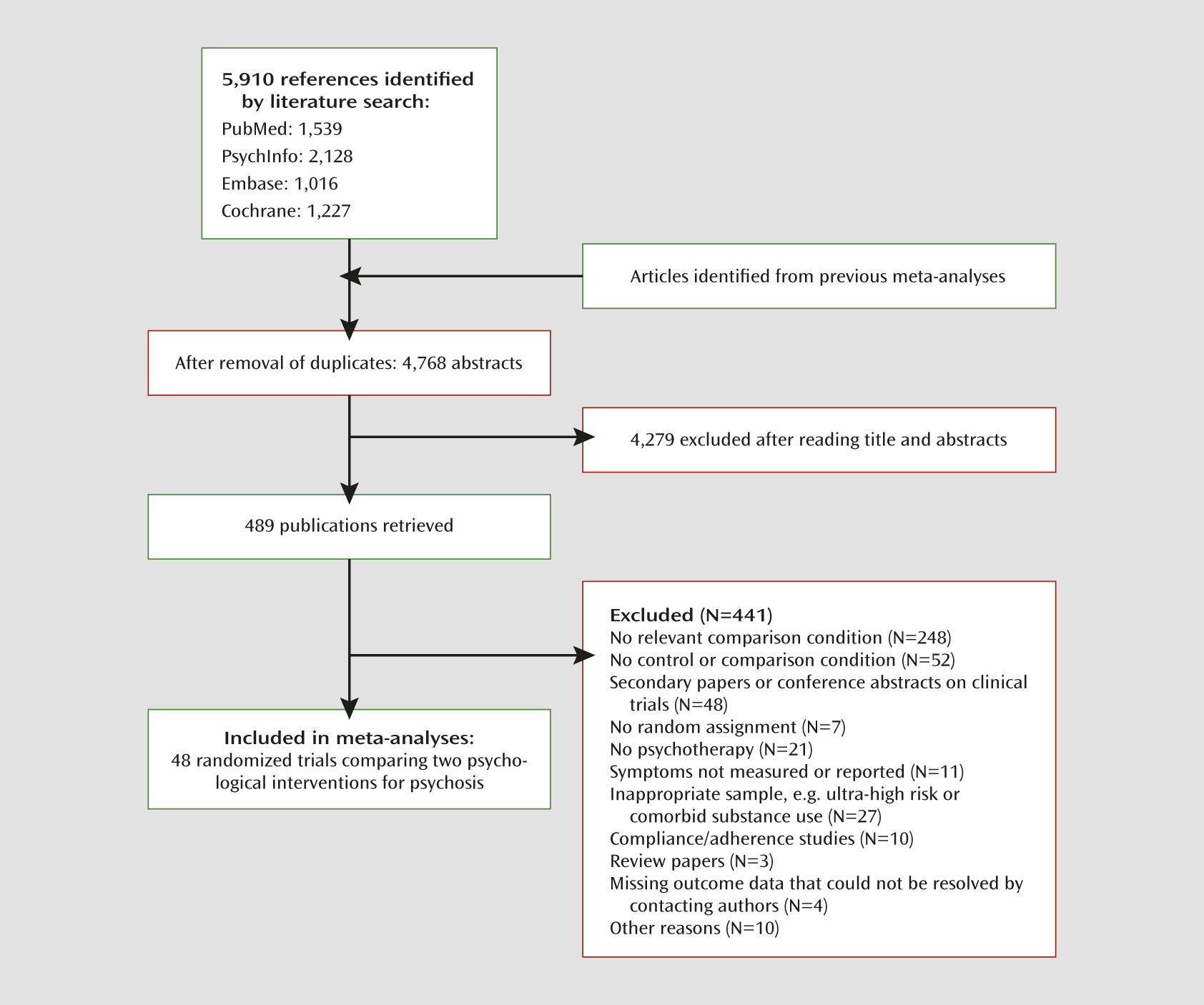
Search Strategy
Study Selection
| Treatment | Definition | Nst | Np |
|---|---|---|---|
| Befriending | Participants are assigned social support to match therapy hours provided in other conditions. Typically this consists of friendly discussion or social activities, not directly related to symptoms, with a supportive and empathic individual. Discussion instead focuses primarily on neutral topics, such as current affairs or hobbies, and structured group activities may also be provided. Befriending has been suggested as an efficacious intervention in reducing symptoms of psychosis (26, 27). | 11 | 400 |
| Cognitive-behavioral therapy (CBT) | CBT aims to promote awareness of the links between thoughts, behaviors, and feelings to help implement changes in symptoms and functioning. Therapists focus on the modification of dysfunctional thoughts and self-defeating behaviors that perpetuate symptoms or suffering. CBT specifically targeting psychosis has been developed primarily since the 1990s and was originally focused on coping with symptoms (28, 29), whereas more recent approaches have focused on challenging maladaptive cognitions through cognitive restructuring and a formulation-based approach (30–32). We identified these as two main subtypes of CBT for the purposes of this meta-analysis, referring to them as “coping enhancement” and “generic CBT.” | 22 | 706 |
| Cognitive remediation | Cognitive deficits have been widely implicated as influential in the development and course of psychosis and have therefore been suggested as worthy treatment targets (33). Cognitive remediation refers to those interventions that target basic cognitive processes, such as working memory, attention, and executive function. This intervention is intended to improve these basic cognitive functions and may also be intended to improve various other aspects of functioning. Computer-based tasks are often the chosen method of implementing cognitive remediation. | 11 | 475 |
| Psychoeducation | Provision of relevant information to participants about their diagnosis with the aim of improving their understanding of and coping with their diagnosis. Various psychoeducation methods have been developed for psychosis that go further than provision of basic information and therefore may involve development of coping strategies and role playing. A group format is often utilized, and there is often considerable diversity in what may be labeled “psychoeducation.” This modality is often used as a comparator intervention for more standardized forms of intervention. | 8 | 249 |
| Social skills training | Behavioral intervention based on behavioral and social learning traditions in which participants’ social functioning is targeted in order to improve their ability to perform in social situations, manage daily life tasks, and reduce social distress. Importance is typically placed on verbal and nonverbal communication alongside learning appropriate perception and responses to social cues. The intervention may also include training in independent living skills. | 16 | 541 |
| Supportive counseling | Nondirective talking therapy that may be based on the work of Carl Rogers (34) or may simply be described in studies as a nondirective intervention in which participants have an open forum to discuss their difficulties, without being actively led or challenged by the therapist. Supportive counseling was therefore defined as an intervention in which the common factors of psychotherapy were present without the specific techniques applied in other, more directive therapies, such as CBT. The opportunity to discuss problems with an empathic therapist in a healing setting may provide relief for the participant without any focus on acquiring new skills or challenging cognitive distortions. Supportive counseling is often used as a means of comparing other interventions against only the common factors of psychological interventions (1). | 17 | 529 |
Quality Assessment
Data Extraction and Selection of Outcome Measures
| Study Authors (Reference Number) | Sample Characteristics | Relevant Comparisons | Symptom Outcome Measures | Format | Bias Risk (0–4) | Duration (weeks) | Follow-Up | Allegiance |
|---|---|---|---|---|---|---|---|---|
| Barretto et al. (36) | DSM-IV schizophrenia; 6 months clozapine treatment-resistant; outpatients | CBT (N=12) vs. BF (N=10) | CGI, BPRS, PANSS | Individual | 2 | 21 | 6 months | CBT |
| Bechdolf et al. (37, 38) | ICD-10 schizophrenia or related disorder; inpatients | CBT (N=40) vs. PE (N=48) | PANSS | Group | 0 | 8 | 6 and 24 months | None |
| Bowie et al. (39) | Schizophrenia or schizoaffective disorder; outpatients | SST (N=38) vs. CR (N=38) | PANSS | Group | 1 | 12 | 24 weeks | None |
| Cather et al. (40) | Schizophrenia or schizoaffective disorder; outpatients | CBT (N=15) vs. PE (N=13) | PANSS, PSYRATS | Individual | 1 | 16 | N/A | CBT |
| Crawford et al. (41) | Schizophrenia; outpatients | BF (N=140) vs. AT (N=140) | PANSS | Group | 0 | 12 | 24 months | AT |
| Dobson et al. (42) | DSM-III schizophrenia; outpatients (severe patients excluded) | SST (N=15) vs. BF (N=13) | PANSS | Group | 3 | 11 | 3 months | None |
| Drury et al. (43, 44) | Current functional psychosis, excluding bipolar, hypomania, organic syndrome, confusional states, and drug or alcohol disorders | CBT (N=20) vs. BF (N=20) | PAS | Both | 3 | 12 | 5 years | CBT |
| Durham et al. (45) | Schizophrenia, schizoaffective disorder, or delusional disorder with positive symptoms; outpatient and inpatient | CBT (N=22) vs. SC (N=23) | PANSS, PSYRATS, GAS | Individual | 0 | 39 | 3 months | CBT |
| Eack et al. (46) | DSM-IV schizophrenia or schizoaffective disorder, in early stages of illness; outpatients | CR (N=31) vs. PE (N=27) | Composite symptoms | Group | 2 | 104 | 12 months | CR |
| Falloon et al. (47, 48) | DSM-III schizophrenia from families high in expressed emotion; inpatients | SC (N=18) vs. FI (N=18) | Clinical exacerbation; remission; target symptom ratings | Individual | 3 | 39 | 24 months | FI |
| Farreny et al. (49) | DSM-IV-TR schizophrenia or schizoaffective disorder; illness duration >2 years; outpatients | CR (N=34) vs. BF (N=28) | PANSS | Group | 2 | 16 | 40 weeks | CR |
| Fries et al. (50) | ICD-10 schizophrenia and schizoaffective disorder; at least two hospitalizations; in at least partial remission at baseline | PE (N=23) vs. SC (N=17) | BPRS, SANS | Group | 4 | 25 | 12 months | None |
| Garety et al. (51) | Recently relapsed nonaffective psychosis (ICD-10 F2 or DSM-IV), with positive symptoms; carers included in study | CBT (N=27) vs. FI (N=28) | PANSS, PSYRATS, BDI, BAI | Individual | 0 | 52 | 24 months | None |
| Haddock et al. (52) | DSM-IV schizophrenia or schizoaffective disorder (< 5 years); current acute ward admission for positive symptoms | CBT (N=9) vs. SC (N=10) | BPRS | Individual | 1 | 5 | N/A | CBT |
| Haddock et al. (53) | DSM-IV schizophrenia or schizoaffective disorder; with history of violence; current antipsychotic medication and positive symptoms | CBT (N=38) vs. BF (N=39) | PANSS, PSYRATS | Individual | 0 | 26 | 12 months | CBT |
| Hayes et al. (54) | DSM-III-R schizophrenia; noncurrent positive symptoms; from a range of services | SST (N=23) vs. SC (N=22) | BPRS, SANS | Group | 4 | 18 | 6 months | SST |
| Hogarty et al. (55, 56) | RDC schizophrenia or schizoaffective disorder from families high in expressed emotion; inpatients | SST (N=23) vs. FI (N=23) | Symptom relapse | Individual | 4 | 104 | N/A | None |
| Hogarty et al. (57, 58) | DSM-III-R or DSM-IV schizophrenia or schizoaffective disorder; outpatients | CR (N=67) vs. PE (N=54) | Composite symptoms | Group | 3 | 52 | 24 months | CR |
| Horan et al. (59) | DSM-IV schizophrenia or schizoaffective disorder; clinically stable outpatients | SST (N=17) vs. PE (N=17) | BPRS | Group | 2 | 6 | N/A | SST |
| Horan et al. (60) | DSM-IV schizophrenia, schizoaffective disorder, delusional disorder, or psychosis not otherwise specified (not secondary to substance disorder); clinically stable outpatients | SST (N=19) vs. CR (N=24) | BPRS | Group | 2 | 12 | N/A | SST |
| Jackson et al. (61) | First-episode psychosis, including schizophrenia, schizophreniform, schizoaffective, bipolar, delusional disorder, and psychosis not otherwise specified; inpatient and outpatient | CBT (N=31) vs. BF (N=31) | BPRS, SANS | Individual | 2 | 12 | 12 months | CBT |
| Keefe et al. (62) | Chronic DSM-IV schizophrenia, moderate severity | CR (N=27) vs. BF (N=26) | PANSS | Group | 1 | 12 | N/A | CR |
| Klingberg et al. (63, 64) | DSM-IV schizophrenia, with at least one negative symptom; positive symptoms excluded; outpatients | CBT (N=99) vs. CR (N=99) | PANSS, SANS, CDSS, CGI, SCL-90 | Individual | 0 | 52 | N/A | CBT |
| Lecomte et al. (65, 66) | Early psychosis (< 2 years), with current psychotic symptoms; stabilized outpatients | CBT (N=48) vs. SST (N=54) | BPRS | Group | 0 | 13 | 6 and 12 months | None |
| Lewis et al. (30) | DSM-IV schizophrenia, schizophreniform, schizoaffective, or delusional disorder; first or second admission; inpatients and outpatients | CBT (N=101) vs. SC (N=106) | PANSS, PSYRATS | Individual | 0 | 5 | 18 months | CBT |
| Liberman et al. (67) | Persistent and unremitting schizophrenia; outpatients | SST (N=42) vs. OT (N=42) | BSI, GAS, BPRS | Both | 3 | 26 | 24 months | None |
| Lukoff et al. (68) | DSM-III schizophrenia; inpatients | SST (N=14) vs. PE (N=14) | PAS | Group | 2 | 10 | N/A | None |
| Marder et al. (69) | DSM-III schizophrenia; at least two acute episodes or 2 years of psychotic symptoms; male outpatients | SST (N=13) vs. SC (N=14) | BPRS exacerbations | Group | 3 | 104 | N/A | None |
| Moritz et al. (70) | Broad psychotic inpatients who met criteria for schizophreniform disorder | CBT (N=24) vs. CR (N=24) | PANSS, PSYRATS | Both | 0 | 4 | N/A | CBT |
| Ng and Cheung (71) | DSM-IV schizophrenia; inpatients | SST (N=18) vs. SC (N=18) | BPRS, SANS | Group | 0 | 8 | 6 months | SST |
| O’Connor et al. (72) | DSM-IV delusional disorder; stabilized on medication | CBT (N=12) vs. SC (N=12) | MADS, BAI, BDI | Individual | 3 | 24 | N/A | CBT |
| Ojeda et al. (73) | DSM-IV schizophrenia; treatment-resistant; inpatients | CR (N=47) vs. OT (N=46) | PANSS | Individual | 2 | 13 | N/A | CR |
| Patterson et al. (74) | DSM-IV schizophrenia or schizophreniform disorder; older chronic Latino inpatients | SST (N=21) vs. SC (N=8) | PANSS | Group | 3 | 26 | 12 months | SST |
| Patterson et al. (75) | DSM-IV schizophrenia or schizophreniform disorder; older chronic inpatients | SST (N=124) vs. SC (N=116) | PANSS, HAM-D | Group | 2 | 26 | N/A | SST |
| Penadés et al. (76, 77) | DSM-IV schizophrenia, chronic, with a prevalence of negative symptoms and cognitive impairment | CBT (N=20) vs. CR (N=20) | PANSS | Individual | 0 | 17 | 6 months | CR |
| Penn et al. (78) | Schizophrenia or schizoaffective disorder and current auditory hallucinations; outpatients | CBT (N=32) vs. SC (N=33) | PANSS, BAVQ, PSYRATS | Group | 0 | 12 | 3 and 12 months | CBT |
| Pinto et al. (79) | DSM-IV schizophrenia; treatment-refractory; outpatients | CBT (N=19) vs. SC (N=18) | BPRS, SAPS, SANS | Individual | 3 | 26 | N/A | CBT |
| Rodewald et al. (80) | DSM schizophrenia or schizoaffective disorder; inpatients | CR (N=44) vs. PST (N=45) | PANSS | Group | 3 | 3 | N/A | PST |
| Röhricht and Priebe (81) | DSM-IV schizophrenia; at least two episodes; outpatients | SC (N=21) vs. BP (N=24) | PANSS | Group | 0 | 10 | 4 months | BP |
| Sensky et al. (26) and Turkington et al. (82) | DSM-IV or ICD-10 schizophrenia; treatment-resistant; outpatients | CBT (N=46) vs. BF (N=44) | CPRS, SANS, MADRS | Individual | 0 | 39 | 9 months, 5 years | CBT |
| Shawyer et al. (83) | DSM-IV schizophrenia or related condition; with command hallucinations in previous 6 months; outpatients | CBT (N=21) vs. BF (N=22) | PANSS, PSYRATS, CH | Individual | 0 | 15 | 6 months | CBT |
| Tarrier et al. (28) | DSM-III-R schizophrenia; treatment resistant | CBT (N=15) vs. PST (N=12) | BPRS, PSE | Individual | 3 | 6 | 6 months | CBT |
| Tarrier et al. (29, 84, 85, 86) | Schizophrenia according to PSE; acute-ward inpatients | CBT (N=19) vs. SC (N=19) | BPRS, SANS | Individual | 0 | 13 | 12 months | CBT |
| Tas et al. (87) | DSM-IV schizophrenia; clinically stable outpatients | SST (N=22) vs. BF (N=27) | PANSS | Group | 0 | 16 | N/A | SST |
| Valmaggia et al. (31) | DSM-IV schizophrenia; with residual delusions or auditory hallucinations; medication resistant | CBT (N=36) vs. SC (N=26) | PANSS, PSYRATS | Individual | 0 | 22 | 6 months | CBT |
| Wykes et al. (88, 89) | DSM-IV schizophrenia; with >2 years contact with services; outpatients and inpatients | CR (N=20) vs. OT (N=16) | BPRS | Individual | 0 | 13 | 6 months | CR |
| Xiang et al. (90) | DSM-IV schizophrenia; clinically stable outpatients | SST (N=48) vs. SC (N=48) | PANSS | Group | 1 | 9 | 6 months | SST |
| Xiang et al. (91) | DSM-IV schizophrenia; clinically stable inpatients and outpatients | SST (N=50) vs. PE (N=53) | PANSS | Group | 2 | 4 | 6 and 12 months | SST |
Meta-Analyses
Heterogeneity
Additional Analyses
Power Calculation
Results
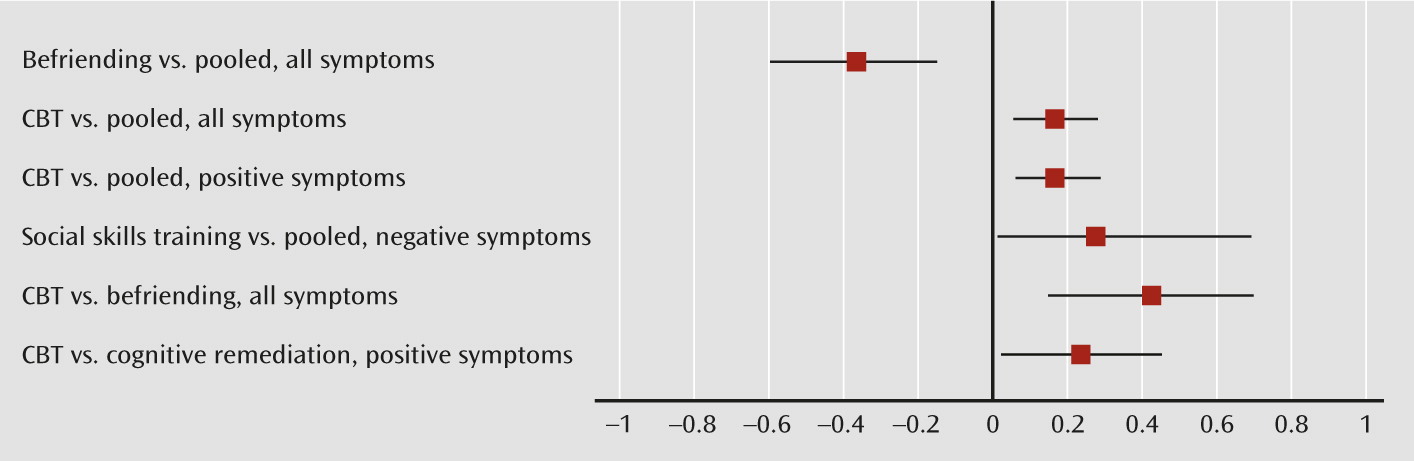
Differences Between Psychological Interventions and Other Interventions Pooled
| Comparison | N | Hedges’ g | 95% CI | Z-Score | Q | I2 (%) |
|---|---|---|---|---|---|---|
| Befriending vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 11 | –0.37* | –0.60, –0.13 | –3.08 | 21.24* | 52.93 |
| Excluding high risk of bias (≥3) | 9 | –0.28* | –0.51, –0.05 | –2.39 | 14.84 | 46.08 |
| Excluding low risk of bias (≥2) | 6 | –0.22 | –0.50, 0.06 | –1.56 | 10.78 | 53.61 |
| Excluding any risk of bias (≥1) | 5 | –0.20 | –0.52, 0.11 | –1.27 | 10.04* | 60.17 |
| Positive symptoms | ||||||
| All eligible studies/excluding high risk (≥3) | 6 | –0.14 | –0.41, 0.13 | –0.10 | 8.81 | 43.23 |
| Excluding any risk of bias (≥1) | 4 | –0.17 | –0.56, 0.22 | –0.86 | 8.50* | 64.72 |
| Negative symptoms | ||||||
| All eligible studies | 9 | –0.22 | –0.41, 0.04 | –1.69 | 18.12* | 55.85 |
| Excluding high risk of bias (≥3) | 8 | –0.18 | –0.45, 0.80 | –1.37 | 15.93* | 56.67 |
| Excluding low (≥2) and any risk of bias (≥1) | 5 | –0.10 | –0.44, 0.24 | –0.56 | 11.94* | 66.49 |
| General symptoms (PANSS) | 5 | –0.24 | –0.61, 0.13 | –1.26 | 10.42* | 61.61 |
| Cognitive behavioral therapy vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 22 | 0.16* | 0.04, 0.28 | 2.64 | 23.91 | 12.18 |
| Excluding high risk of bias (≥3) | 18 | 0.12* | 0.00, 0.23 | 2.01 | 14.98 | 0.00 |
| Excluding low risk of bias (≥2) | 15 | 0.10 | –0.03, 0.22 | 1.53 | 11.30 | 0.00 |
| Excluding any risk of bias (≥1) | 13 | 0.11 | –0.02, 0.24 | 1.72 | 9.16 | 0.00 |
| Positive symptoms | ||||||
| All eligible studies | 17 | 0.16* | 0.04, 0.28 | 2.67 | 11.17 | 0.00 |
| Excluding high risk of bias (≥3) | 15 | 0.14* | 0.02, 0.27 | 2.32 | 9.42 | 0.00 |
| Excluding low risk of bias (≥2) | 12 | 0.15* | 0.02, 0.28 | 2.18 | 9.19 | 0.00 |
| Excluding any risk of bias (≥1) | 11 | 0.14* | 0.00, 0.27 | 1.97 | 7.44 | 0.00 |
| Negative symptoms | ||||||
| All eligible studies | 15 | 0.04 | –0.09, 0.16 | 0.55 | 13.94 | 0.00 |
| Excluding high risk of bias (≥3) | 14 | 0.02 | –0.10, 0.15 | 0.36 | 13.04 | 0.34 |
| Excluding low risk of bias (≥2) | 11 | –0.00 | –0.15, 0.14 | –0.06 | 8.13 | 0.00 |
| Excluding any risk of bias (≥1) | 10 | –0.01 | –0.15, 0.14 | –0.06 | 8.14 | 0.00 |
| General symptoms (PANSS) | ||||||
| All eligible studies/low risk of bias (≥2) | 8 | 0.10 | –0.13, 0.32 | 0.86 | 12.10 | 42.16 |
| Excluding any risk of bias (≥1) | 7 | 0.05 | –0.14, 0.24 | 0.54 | 7.60 | 21.06 |
| Cognitive remediation vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 11 | 0.13 | –0.05, 0.31 | 1.46 | 14.63 | 31.69 |
| Excluding high risk of bias (≥3) | 10 | 0.20* | 0.01, 0.39 | 2.06 | 11.34 | 20.65 |
| Excluding low risk of bias (≥2) | 6 | 0.14 | –0.05, 0.33 | 1.41 | 3.21 | 0.00 |
| Excluding any risk of bias (≥1) | 4 | 0.12 | –0.11, 0.34 | 1.02 | 2.49 | 0.00 |
| Positive symptoms | ||||||
| All eligible studies | 6 | 0.16 | –0.17, 0.49 | 0.97 | 14.11* | 64.56 |
| Excluding low risk of bias (≥2) | 4 | 0.29 | –0.06, 0.64 | 1.63 | 6.61 | 54.59 |
| Negative symptoms | ||||||
| All eligible studies | 6 | –0.14 | –0.39, 0.06 | –1.12 | 8.47 | 40.99 |
| Excluding high (≥3) and low (≥2) risk of bias | 4 | –0.08 | –0.38, 0.22 | –0.50 | 5.23 | 42.59 |
| Psychoeducation vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 8 | 0.10 | –0.27, 0.11 | –0.80 | 8.02 | 12.66 |
| Excluding high risk of bias (≥3) | 6 | –0.13 | –0.41, 0.14 | 0.94 | 7.43 | 32.67 |
| Positive symptoms | ||||||
| All eligible studies/excluding high risk (≥3) | 4 | 0.19 | –0.06, 0.44 | 1.50 | 1.70 | 0.00 |
| Negative symptoms | ||||||
| All eligible studies | 5 | 0.02 | –0.22, 0.25 | 0.13 | 3.06 | 0.00 |
| Excluding high risk of bias (≥3) | 4 | 0.03 | –0.22, 0.28 | 0.23 | 2.97 | 0.00 |
| Social skills training vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 16 | 0.06 | –0.17, 0.28 | 0.49 | 45.33* | 66.91 |
| Excluding high risk of bias (≥3) | 10 | 0.19* | 0.02, 0.36 | 2.15 | 8.72 | 0.00 |
| Excluding low risk of bias (≥2) | 4 | 0.34 | –0.02, 0.70 | 1.87 | 5.47 | 45.13 |
| Positive symptoms | ||||||
| All eligible studies | 7 | 0.09 | –0.23, 0.41 | 0.56 | 16.44* | 63.51 |
| Excluding high risk of bias (≥3) | 6 | 0.09 | –0.26, 0.45 | 0.50 | 16.41* | 69.53 |
| Negative symptoms | ||||||
| All eligible studies | 9 | 0.27* | 0.01, 0.53 | 2.01 | 17.33* | 53.83 |
| Excluding high risk of bias (≥3) | 7 | 0.32* | 0.07, 0.56 | 2.55 | 10.25 | 41.47 |
| Excluding low risk of bias (≥2) | 4 | 0.56* | 0.31, 0.82 | 4.29 | 1.99 | 0.00 |
| Supportive counseling vs. all other therapies | ||||||
| All symptoms | ||||||
| All eligible studies | 17 | 0.00 | –0.21, 0.22 | 0.04 | 40.31* | 60.31 |
| Excluding high risk of bias (≥3) | 10 | 0.01 | –0.30, 0.32 | 0.06 | 32.97 | 72.70 |
| Excluding low risk of bias (≥2) | 9 | –0.12 | –0.30, 0.05 | –1.37 | 6.18 | 0.00 |
| Excluding any risk of bias (≥1) | 7 | –0.08 | –0.28, 0.11 | –0.83 | 1.74 | 0.00 |
| Positive symptoms | ||||||
| All eligible studies | 8 | –0.14 | –0.36, 0.09 | –1.12 | 10.28 | 31.90 |
| Excluding high (≥3) and low (≥2) risk of bias | 6 | –0.05 | –0.25, 0.15 | –0.51 | 5.33 | 6.27 |
| Excluding any risk of bias (≥1) | 5 | –0.02 | –0.27, 0.23 | –0.17 | 5.00 | 19.98 |
| Negative symptoms | ||||||
| All eligible studies | 9 | –0.12 | –0.41, 0.17 | –0.83 | 18.55* | 56.87 |
| Excluding high (≥3) and low (≥2) risk of bias | 6 | –0.21 | –0.57, 0.15 | –1.13 | 13.34* | 62.52 |
| Excluding any risk of bias (≥1) | 5 | –0.09 | –0.45, 0.27 | –0.50 | 7.74 | 48.30 |
Direct Comparisons of Psychological Interventions
| Comparison | N | Hedges’ g | 95% CI | Z-Score | Q | I2 (%) | p |
|---|---|---|---|---|---|---|---|
| Direct comparisons of two interventions | |||||||
| CBT vs. befriending | |||||||
| All symptoms (R) | 6 | 0.42* | 0.15, 0.69 | 3.02 | 7.00 | 28.61 | |
| CBT vs. supportive counseling | |||||||
| All symptoms (F/R) | 8 | 0.10 | –0.10, 0.30 | 0.99 | 6.09 | 0.00 | |
| Positive symptoms (F/R) | 6 | 0.23* | 0.01, 0.44 | 2.07 | 5.00 | 0.04 | |
| Social skills training vs. supportive counseling | |||||||
| All symptoms (R) | 6 | –0.07 | –0.54, 0.40 | –0.29 | 26.27 | 80.96 | |
| CBT subtypes vs. other interventions pooled | |||||||
| Coping enhancement subtype | |||||||
| All symptoms (F/R) | 6 | –0.01 | –0.19, 0.18 | –0.08 | 1.83 | 0.00 | |
| Negative symptoms (F/R) | 5 | –0.04 | –0.23, 0.15 | –0.41 | 2.45 | 0.00 | |
| Generic subtype | |||||||
| All symptoms (R) | 16 | 0.22* | 0.08, 0.37 | 2.97 | 16.96 | 11.58 | |
| Positive symptoms (F/R) | 13 | 0.17* | 0.03, 0.32 | 2.28 | 10.66 | 0.00 | |
| Negative symptoms (R) | 10 | 0.01 | –0.08, 0.28 | 1.07 | 10.44 | 13.76 | |
| Subgroup analyses of CBT: group vs. individual formatb | |||||||
| All symptoms | |||||||
| Individual (R) | 18 | 0.18* | 0.05, 0.32 | 2.66 | 19.93 | 14.9 | |
| Group (R) | 3 | 0.00 | –0.26, 0.27 | 0.03 | 1.08 | 0.00 | |
| Overall (R) | 21 | 0.13 | –0.02, 0.29 | 1.64 | 22.45 | 10.93 | 0.24 |
| Positive symptoms | |||||||
| Individual (F/R) | 13 | 0.16* | 0.02, 0.30 | 2.17 | 9.04 | 0.00 | |
| Group (F/R) | 3 | 0.12 | –0.13, 0.36 | 0.93 | 0.39 | 0.00 | |
| Overall (F/R) | 16 | 0.15* | 0.01, 0.34 | 2.04 | 9.50 | 0.00 | 0.80 |
| Negative symptoms | |||||||
| Individual (F/R) | 12 | 0.09 | –0.06, 0.23 | 1.15 | 12.05 | 8.68 | |
| Group (F/R) | 3 | –0.11 | –0.35, 0.14 | –0.85 | 0.16 | 0.00 | |
| Overall (F/R) | 15 | 0.02 | –0.17, 0.20 | 0.17 | 13.94 | 0.00 | 0.19 |
| Subgroup analyses of researcher allegiance for comparisons with robust significant effects | |||||||
| CBT vs. all other therapiesc | |||||||
| Positive symptoms (F/M) | |||||||
| Excluding high risk of bias (≥3) | |||||||
| No allegiance | 3 | 0.10 | –0.15, 0.35 | 0.80 | 0.24 | 0.00 | 0.42 |
| Allegiance for CBT | 11 | 0.17 | 0.01, 0.32 | 2.40 | 5.35 | 0.00 | |
| Excluding low risk of bias (≥2) | |||||||
| No allegiance | 2 | 0.08 | –0.25, 0.40 | 0.50 | 0.21 | 0.00 | 0.60 |
| Allegiance for CBT | 9 | 0.18 | 0.03, 0.33 | 2.33 | 5.07 | 0.00 | |
| Excluding any risk of bias (≥1) | |||||||
| No allegiance | 2 | 0.08 | –0.25, 0.40 | 0.50 | 0.21 | 0.00 | 0.58 |
| Allegiance for CBT | 8 | 0.19 | 0.03, 0.34 | 2.36 | 4.96 | 0.00 | |
| Social skills training vs. all other therapies | |||||||
| Negative symptoms (M) | |||||||
| All eligible studies | |||||||
| No allegiance | 3 | 0.37 | 0.04, 0.7 | 2.20 | 2.30 | 13.27 | 0.55 |
| Allegiance for social skills training | 6 | 0.21 | –0.21, 0.62 | 0.98 | 15.50 | 67.7 | |
| Excluding high risk of bias (≥3) | |||||||
| No allegiance | 2 | 0.30 | –0.10, 0.71 | 1.48 | 1.51 | 33.82 | 0.83 |
| Allegiance for social skills training | 6 | 0.36 | 0.04, 0.69 | 2.19 | 8.97 | 44.25 | |
Meta-Analyses for CBT Subtypes
Researcher allegiance.
Publication bias.
Discussion
Acknowledgments
Supplementary Material
- View/Download
- 32.12 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

