Posttraumatic stress disorder (PTSD) is a widespread (
1) and debilitating (
2) disorder. Its annual prevalence of 3.5% (
1), lifetime prevalence of 6.8% (
3), and suicidal risk (
4) constitute a public health problem. Cognitive-behavioral therapies dominate the moderately effective available treatments (
5,
6). The central technique of most empirically validated psychotherapies for PTSD involves exposing patients to objectively safe reminders of their trauma, including reviewing traumatic memories, with the aim of habituating and extinguishing learned fear responses (
7). Validated cognitive-behavioral therapies—prolonged exposure, cognitive processing therapy, eye movement desensitization and reprocessing—rely largely on exposure modalities (
8–
10), although cognitive processing therapy has demonstrated efficacy without its exposure component (
11). Expert consensus and treatment guidelines emphasize that “the shared element of controlled exposure may be the critical intervention” (
8). The Institute of Medicine in 2008 endorsed exposure therapy as the sole adequately empirically supported trauma treatment, finding too little evidence to support other psychosocial techniques and psychopharmacology (
9). The mechanism of exposure-based treatment meshes with animal models of fear activation (
12); imaging studies link it to prefrontal cortical suppression of amygdalar fear responses to trauma reminders (
13).
Like most psychiatric interventions, exposure-based treatments also have known limits. Not all patients respond; most do not remit (
14,
15). Exposure-based treatments can feel grueling for patients and therapists (
16). Moreover, PTSD’s complex picture contains a powerful interpersonal theme. Interpersonal traumas more often trigger PTSD (
10,
17), causing more severe distress than events without human agency such as natural disasters. Many PTSD symptoms reflect interpersonal difficulties (
17), such as emotional withdrawal from relationships. Mistrusting their interpersonal environments, traumatized individuals develop “interpersonal hypervigilance” (
18). Social support protects against developing PTSD and fosters recovery (
10,
18).
We therefore adapted interpersonal psychotherapy (IPT) (
19), a time-limited, diagnosis-targeted psychotherapy efficacious for mood (
20) and eating disorders (
19), as a non-exposure-based, non-cognitive-behavioral PTSD treatment. Patients focus on current interpersonal encounters rather than past trauma (
10,
18). IPT therapists, monitored by adherence raters checking session tapes, may neither evoke nor encourage exposure to trauma reminders.
Based on promising pilot data suggesting that IPT might benefit PTSD symptoms (
18,
22,
23), including our own small open trial (N=14; 69% response rate [
18]), we conducted a 14-week randomized trial comparing IPT, prolonged exposure (
24) (as a standard, reference treatment), and relaxation therapy (
25) (an active control condition) in unmedicated patients with chronic (>3 months) DSM-IV PTSD. Previous research has shown prolonged exposure to be superior to relaxation therapy (
26,
27). We hypothesized that IPT would demonstrate no more than minimal inferiority to prolonged exposure and that prolonged exposure and IPT would both be superior to relaxation therapy. We secondarily hypothesized that prolonged exposure and IPT would have comparable response and remission rates, exceeding those of relaxation therapy, and that improvements in social functioning and quality of life would echo this pattern. Because IPT has had low attrition (
18,
22) and takes a more supportive, less confrontational stance, we anticipated lower attrition than for prolonged exposure, which has historical dropout rates >20% (
28). We further investigated the effect of comorbid depression on PTSD outcome.
Method
The study protocol was approved by the Institutional Review Board of the New York State Psychiatric Institute. Potential study subjects responding to advertisements on the Internet, in print media, and on hospital bulletin board flyers telephoned research assistants for brief, semistructured screening interviews (
29). Those who were screen eligible were invited to attend clinical interviews with research psychiatrists. After providing written informed consent for intake, individuals were interviewed to assess DSM-IV-defined trauma, PTSD as primary diagnosis, and exclusion criteria. They received physical examinations and appropriate laboratory studies. Independent evaluators (doctoral-level psychologists) interviewed subjects using the Clinician-Administered PTSD Scale (CAPS) (
30), the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID) (
31), and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (
32) to establish current and lifetime diagnoses.
Eligible individuals who provided written informed consent for the treatment study were randomly assigned to receive prolonged exposure, IPT, or relaxation therapy, in a 4:4:3 ratio. Randomization followed a computer-generated program designed by the study’s statistician, who had no patient contact. Randomization was stratified by presence of major depressive disorder (diagnosed according to the SCID, along with a score ≥20 on the 24-item Hamilton Depression Rating Scale [HAM-D] [
33]) and implemented in blocks of random sizes (11 or 22).
Participants
Participants were 18–65 years old and had a primary DSM-IV diagnosis of chronic PTSD and a CAPS score >50 (indicating at least moderate PTSD severity). Exclusion criteria included psychotic disorders, bipolar disorder, an unstable medical condition, substance dependence, or active suicidal ideation; antisocial, schizotypal, or schizoid personality disorder; prior nonresponse to >8 weeks of a study therapy; and ongoing psychiatric treatment including pharmacotherapy.
Treatments
The three manualized psychotherapies differ markedly. In prolonged exposure, patients narrate an increasingly detailed trauma narrative (imaginal exposure) and confront trauma reminders (in vivo exposure) to extinguish fear responses. Relaxation therapy, which is highly scripted, induces progressive muscle and mental relaxation. These treatments require listening to session or relaxation tapes as homework. IPT addressed not trauma but its interpersonal aftermath, and no homework was assigned. The first half of IPT emphasized affective attunement, recognizing, naming, and expressing one’s feelings in non-trauma-related interpersonal situations; the remainder addressed typical IPT problem areas (e.g., role disputes, role transitions) (
19).
We previously tested IPT as 14 weekly 50-minute sessions (700 minutes) (
18). Other researchers designed prolonged exposure to have 10 weekly 90-minute sessions (900 minutes), and relaxation therapy to have nine weekly 90-minute sessions and a final 30-minute session (840 minutes). National Institute of Mental Health (NIMH) reviewers recommended stretching the latter therapies across 14 weeks to equalize treatment duration. Prolonged exposure and relaxation therapy expert supervisors were comfortable scheduling seven consecutive weekly sessions and dispersing the remaining three sessions over 7 weeks.
Therapists
The study therapists were psychologists or psychiatrists. Each therapist treated a minimum of two pilot cases to ensure expertise. Therapists were audiotaped, monitored for adherence, and supervised by experts to ensure adherence and competence. The study included two prolonged exposure therapists who had experience from previous PTSD research (
15) and were supervised by E.H.; four IPT therapists who were trained and supervised by J.C.M.; and four relaxation therapy therapists who were trained and supervised by K.L. Therapists reported primary allegiance to their study therapy (
34). Therapy teams did not differ significantly in mean age (47.5 years [SD=10.6] for prolonged exposure, 41.0 years [SD=9.1] for IPT, and 34.8 years [SD=5.1] for relaxation therapy) or in years of modality-specific psychotherapy experience (7.5 years [SD=0.7] for prolonged exposure, 9.0 years [SD=8.4] for IPT, and 3.8 years [SD=4.4] for relaxation therapy). Patients could choose male or female therapists.
Assessments
Experienced independent evaluators were blind to treatment condition, and patients were reminded not to identify their therapy or therapist during evaluations. Major evaluations occurred at baseline, at week 7, and at week 14.
The trial employed established instruments. The widely used 30-item CAPS was used to assess PTSD symptoms on frequency and intensity scales. Subscales describe intrusion, avoidance, and hyperarousal symptom clusters and associated affective features. Interrater reliability for frequency and severity is excellent for the intrusion, hyperarousal, and avoidance subscales (r values, >0.92). Each subscale has good internal consistency (Cronbach’s alpha=0.87) (
30,
35). A CAPS score >50 indicates at least moderate PTSD; 60, severe PTSD; and 80, extreme PTSD; scores <20 in patients with PTSD indicate remission (
36). The independent evaluators achieved excellent interrater reliability on the CAPS (primary outcome measure; Shrout-Fleiss interclass reliability coefficient=0.93), the HAM-D (0.89), and other instruments, and they met regularly to compare taped interview ratings.
A modified version of the Posttraumatic Stress Scale–Self Report version (
37) was used to evaluate subjective PTSD symptoms. Other instruments were used to measure social adjustment and functioning (the Social Adjustment Scale–Self-Report [
38]), quality of life (the Quality of Life Enjoyment and Satisfaction Questionnaire [
39]), and interpersonal functioning (the Inventory of Interpersonal Problems [
40]). Lacking an instrument to measure self-exposure, we developed a novel scale (the Self-Initiated In Vivo Exposure Scale), based on Foa and colleagues’ Subjective Units of Distress (
24) scale, to assess patients’ self-exposure to trauma reminders. We used this scale to develop a hierarchy of patients’ fear intensity in response to trauma reminders and to assess how often patients were avoiding these feared reminders (“frequency of avoidance”).
All treatment sessions were audiotaped, encrypted, and transmitted to supervisors. Adherence raters (master’s-level psychologists) randomly sampled one early and one late therapy audiotape and rated them with Hollon’s Collaborative Study Psychotherapy Rating Scale (
41) and a briefer quality-of-therapy measure to ensure therapist fidelity. Twenty sessions rated by multiple raters showed perfect agreement on the latter form. Raters found the three disparate therapies easily distinguishable and the therapists adherent, correctly identifying rated sessions (N=92), although they did not succeed in rating two tapes for every treatment dyad.
Statistical Analysis
Analyses followed the intention-to-treat principle. Some participants who discontinued treatment were subsequently assessed at the specified assessment times, whereas some participants who completed treatment missed the midtreatment assessment. We compared participants with missing postrandomization data to those without missing data with respect to baseline characteristics. No comparisons between subjects with and without postrandomization assessment overall, or within treatment groups, were significantly different, and no differences approached clinically meaningful magnitude. Efficacy of the three treatments with respect to symptom severity was estimated based on longitudinal mixed-effects models (
42) using multiple imputation for the missing values (
43). For each variable (score on the CAPS, the Posttraumatic Stress Scale–Self Report, the HAM-D, the Social Adjustment Scale–Self-Report, the quality of life measure, and the Inventory of Interpersonal Problems), we used the Markov chain Monte Carlo technique to obtain a monotone missing data pattern. We then applied a predictive mean-matching regression method separately for the three treatment groups (
44); to increase the likelihood that the missing-at-random assumption is valid, in addition to the previous values of the variable being imputed, we used all other symptom variables and baseline major depression status as predictors in predictive mean-matching regression. Fifty imputed data sets were generated.
We modeled the postrandomization values as functions of treatment, time, and their interaction, controlling for baseline values of the outcome and major depression status. If the time-by-treatment interaction was statistically significant, differences between treatments were estimated separately at midtreatment (week 7) and at end of treatment (week 14); otherwise, the model was refitted with only main effects for treatment and time, and the differences were assessed from a model postulating similar relationships between the treatments at all times.
Response and remission rates were estimated based on the observed data using prespecified criteria: response was defined as a decrease >30% from baseline CAPS score, and remission was defined as a CAPS score <20 (
30,
35,
36); participants for whom these data were missing were categorized as nonresponders and nonremitters. Statistical significance was assessed throughout at an alpha of 0.05 (two-sided). We report p values without adjustment for multiple testing, as the reported results pertain to prespecified hypotheses and tests. All analyses used SAS/STAT, version 9.2 (SAS Institute, Cary, N.C.).
A projected enrollment of 165 participants (60 each for the IPT and prolonged exposure groups and 45 for the relaxation therapy group) allowed at least 80% power of two-sided tests based on longitudinal mixed-effects models with a significance threshold of 0.05 to establish 1) the superiority of both IPT and prolonged exposure compared with relaxation therapy (i.e., to reject the null hypothesis of comparability against the alternative that a difference of ≥15 CAPS points favors IPT or prolonged exposure over relaxation therapy) and 2) that IPT would be no more than minimally inferior compared with prolonged exposure (i.e., to reject the null hypothesis that the difference is ≥12.5 CAPS points in favor of prolonged exposure against the alternative that the difference is zero). The planned sample size provided sufficient power (≥80%) to detect a ≥20% difference between prolonged exposure or IPT compared with relaxation therapy with respect to response and remission.
The rationale for requiring sufficient power for a difference of 15 CAPS points for efficacy and for declaring a difference of less than 12.5 CAPS points as not more than minimal inferiority is as follows. The CAPS manual suggests that a 15-point CAPS difference is clinically significant (
45). Regarding minimal inferiority, there is no consensus on the largest difference in efficacy (measured by the CAPS) that would render one treatment only minimally inferior to another. Any number lower than 15 is considered not clinically meaningful. We chose the 12.5 CAPS point boundary for minimal inferiority in communication with the NIMH reviewers of our application. We thus marked the interval between 10 (including) and 15 (not including) CAPS points difference as the range in which IPT would be considered inferior to prolonged exposure, but prolonged exposure not be considered superior to IPT, as the logic of noninferiority trials requires. We split this interval: a difference between 10 (including) and 12.5 (not including) CAPS points would make IPT inferior to prolonged exposure, but only minimally so. A difference of 12.5 (including) to 15 (not including) CAPS points would make it more than minimally inferior. NIMH grant reviewers judged this postulation of the primary hypothesis appropriate.
Results
Cohort
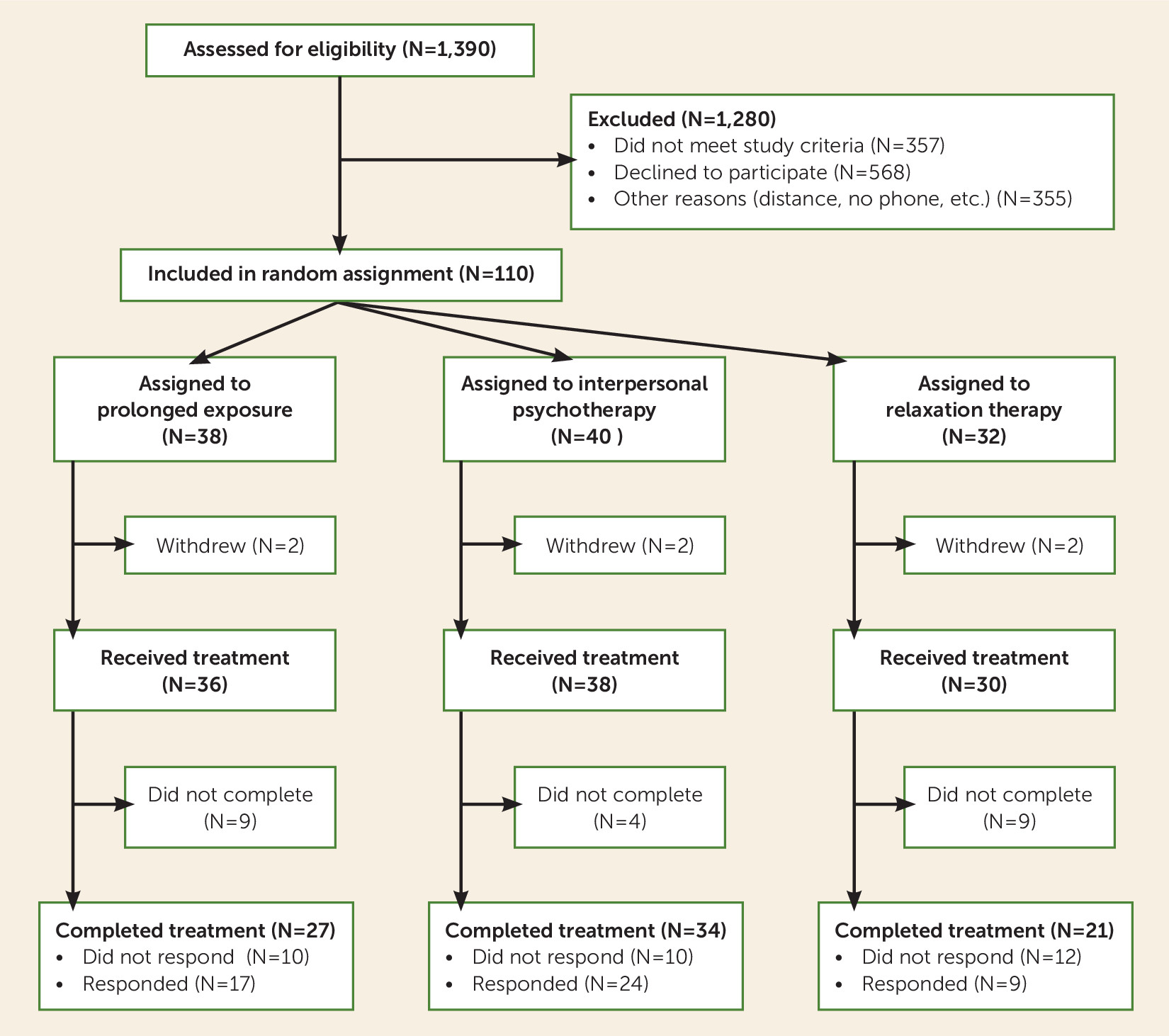
Overall, 110 unmedicated patients with chronic PTSD and a CAPS score >50 were recruited over the course of the 5-year trial (
Figure 1).
Tables 1 and
2 present baseline demographic and clinical characteristics, which indicate a highly traumatized, chronically ill sample. At a mean age of 40.1 years, only 15.5% of these patients were married or cohabitating; only 36.4% held full-time employment (11.8% were students). The sample was racially and ethnically diverse. Ninety-three percent reported interpersonal trauma. More than half (58.2%) reported chronic trauma (mean duration since primary trauma, 14.1 years [SD=14.4]), including sexual (35%) and physical (61.8%) abuse. Thirty-six percent reported trauma in childhood or adolescence. Three-quarters of participants had previously received psychotherapy and almost half had received pharmacotherapy for PTSD.
Table 2 summarizes the participants’ psychiatric debility: half had current comorbid major depression, and one-third had multiple depressive episodes. Nearly half met criteria for personality disorders, particularly paranoid, obsessive-compulsive, and avoidant.
Over the course of treatment, patients in the prolonged exposure group attended a mean of 8.3 sessions (SD=3.1) (a mean of 748 minutes [SD=277] overall), those in the IPT group attended a mean of 12.6 sessions (SD=3.4) (a mean of 630 minutes [SD=69] overall); and those in the relaxation therapy group attended a mean of 7.8 (SD=3.5) sessions (a mean of 667 minutes [SD=290] overall), or 83%, 90%, and 78% of prescribed sessions, respectively.
Outcome
CAPS scores showed substantial symptomatic improvement in each therapy over the 14-week course of treatment (
Table 3), with large within-group pretreatment-posttreatment effect sizes (Cohen’s d): for prolonged exposure, d=1.88; for IPT, d=1.69; and for relaxation therapy, d=1.32. The time-by-treatment interaction was not significant. Compared with relaxation therapy, prolonged exposure showed a significant advantage (p=0.010), and IPT showed an advantage that fell short of statistical significance (p=0.097). The difference between CAPS change scores in prolonged exposure and IPT was 5.5 points, less than the a priori 12.5-point minimal inferiority threshold. The null hypothesis of more than minimal inferiority of IPT was rejected (p=0.035).
Attrition was 15% in the IPT group, 29% in the prolonged exposure group, and 34% in the relaxation therapy group (n.s.). Two patients from each treatment condition withdrew after randomization but before beginning therapy. Rates of response (defined as an improvement >30% in CAPS score) were 63% for IPT, 47% for prolonged exposure, and 38% for relaxation therapy. IPT had a significantly higher response rate than relaxation therapy (χ2=4.45, p=0.03). Treatment remission rates did not differ significantly between groups (26% for prolonged exposure, 23% for IPT, and 22% for relaxation therapy).
On the Posttraumatic Stress Scale–Self Report, patients in the prolonged exposure and IPT groups showed statistically significantly greater improvement in PTSD symptoms compared with those in the relaxation therapy group (p<0.001 and p=0.008, respectively). Patients in the prolonged exposure group improved faster than those in the IPT group and showed an advantage over the IPT group at week 14, although the effect fell short of significance (p=0.053) (
Table 3). Prolonged exposure and IPT each yielded improvement that was statistically superior to relaxation therapy on the quality of life measure, the social functioning measure, and the interpersonal problems measure, and they did not differ significantly from each other.
Mediators and moderators of treatment effect will be addressed elsewhere. We examined two key variables, however. To ensure that IPT therapists were not conducting unintentional exposure therapy, mediation analyses assessed early change (between baseline and week 5) in “frequency of avoidance” of the three highest ranked trauma items on our Self-Initiated In Vivo Exposure Scale as a predictor of week 14 CAPS score. Early change in frequency of avoidance directly (and expectedly) predicted CAPS outcome in the prolonged exposure and relaxation therapy groups, but not in the IPT group (see Figure S1 in the data supplement that accompanies the online edition of this article). This finding supports prolonged exposure and IPT treatment theories.
Comorbid major depressive disorder, a diagnosis carried by half the sample, proved to be a striking moderator of treatment effects. The study was not powered to detect interaction terms, but to avoid omitting potentially important effects due to low power, interactions between treatment and major depressive disorder status with p values ≤0.15 were followed up with pairwise comparisons. The omnibus test assessing whether dropout depended on the interaction between depression status and treatment showed a p value of 0.15. Half of patients who had comorbid depression and were assigned to receive prolonged exposure dropped out: the odds ratio of prolonged exposure attrition with (50%) and without (5.6%) major depression was 17:1 (
Table 4). Dropout among depressed patients in the prolonged exposure group tended to be higher than among depressed patients in the IPT group (p=0.086) and higher than dropout among nondepressed patients in the prolonged exposure group (p=0.006). Dropout among nondepressed patients in the relaxation therapy group tended to be higher than dropout among nondepressed patients in either the IPT or the prolonged exposure group (p=0.068 and p=0.065, respectively). The effect of the interaction between major depression status and treatment response fell short of significance (p=0.058).
Response rates among patients without major depression were higher in the IPT (p=0.008) and prolonged exposure (p=0.032) groups than in the relaxation therapy group. Within the prolonged exposure group, response rates were higher among patients without depression than among those with depression. No evidence emerged for a moderating effect of depression status on treatment effects with respect to longitudinal PTSD severity (as indicated by CAPS score) or remission status.
Adverse Events
We withdrew five patients who, by therapist report and on independent evaluator assessment, developed worsening depression (two patients in the relaxation therapy group), manifested bipolar disorder (one patient in the IPT group), engaged in severe substance abuse (one patient in the IPT group), or violated protocol by obtaining outside treatment (one patient in the prolonged exposure group).
Discussion
Our primary goal in this study was to test whether IPT, a non-exposure-based treatment, was no more than minimally inferior to prolonged exposure for patients with severe, chronic PTSD. As IPT emerged no more than minimally inferior to prolonged exposure on the primary outcome measure, had a statistically nonsignificant but clinically meaningful higher response rate, and had a lower dropout rate among patients with comorbid major depression, the treatments appeared roughly equipotent. These findings contradict the widespread clinical belief in PTSD therapeutics that patients require cognitive-behavioral therapy or exposure to trauma reminders. This news may be a relief to many patients who refuse to face their trauma-related fears, cannot tolerate systematic exposure, or do not benefit from it.
Prolonged exposure did take effect more rapidly than IPT, and it showed a slight (nonsignificant) edge in CAPS score outcome and an advantage just short of significance on the self-report PTSD measure.
Many severely traumatized patients who had reported ineffective community treatment responded to each 14-week treatment modality. In a trial that achieved less than planned enrollment, relaxation therapy, an active control, statistically differed only marginally from IPT on CAPS score outcomes. A larger sample size might have yielded statistical significance. No ideal psychotherapy control exists comparable to pill placebo in pharmacotherapy trials. A study strength is that prolonged exposure and IPT, competing against a robust, active control condition, still showed differential benefits in symptoms and social functioning. This trial potentially adds a novel, very differently focused, non-cognitive-behavioral treatment to the PTSD armamentarium.
Two other critical findings arose. First, comorbid major depressive disorder strongly predicted dropout in the prolonged exposure group but not in the IPT or relaxation therapy groups. Prolonged exposure was developed to target anxiety; although it often reduces depressive symptoms (
14,
46), it may treat major depressive disorder less effectively. Alternatively, comorbid major depression may have rendered tolerating prolonged exposure more difficult. IPT was originally developed to treat major depression, however, and it did so in this study even while focusing on PTSD. The outcomes suggest differential therapeutics: IPT may have preferential advantages over prolonged exposure for patients with comorbid PTSD and major depression. (Alternatively, patients might benefit from concomitant antidepressant pharmacotherapy [
14].) Although few studies have even examined PTSD remission rates—and none, to our knowledge, have examined remission rates for comorbid PTSD and major depression—the extremely low remission rates we observed across treatments for patients with PTSD and comorbid major depression (10%−15%;
Table 4) suggest that this group might benefit from combined treatment with medication (
14). Prolonged exposure may produce greater CAPS score improvement in patients without major depression.
Second, a key mediator suggests that treatment mechanisms differed. Unsurprisingly given the focus on confronting traumatic reminders, patients in prolonged exposure who faced their traumas early had better PTSD outcomes, whereas patients whose avoidance increased early had worse final symptom scores than those whose avoidance did not increase early. Early avoidance had no predictive value in IPT, which deliberately ignores exposure to trauma reminders. IPT may work through alternative, attachment mechanisms involving emotional understanding, social support, and learning to cope with current life (
18,
24,
47) rather than confronting past traumas. Yet, in order to remit from PTSD, patients must eventually face their fears. As previously reported (
18), patients who improved in IPT seemed to gain confidence in daily social interactions, gathered social support, and then spontaneously—without therapist encouragement—exposed themselves to trauma reminders.
We found what many have suspected: exposure therapy is valuable, but not a sine qua non. IPT and cognitive-behavioral therapy both relieve major depression and bulimia. Psychotherapy and psychopharmacotherapy each ameliorate syndromes, presumably via different mechanisms. So why expect only one royal road (
48) to PTSD response?
Some study findings echo results from other trials. IPT, which initially focused on affective attunement and only later in treatment encouraged PTSD patients to change their interpersonal interactions in current relationships, yielded somewhat slower symptom improvement than prolonged exposure, but caught up over time. This pattern resembles some eating disorder comparative trials, in which IPT therapists, barred from discussing binge eating and body image in bulimia, focused on interpersonal relationships. In those studies, IPT yielded slower improvement than cognitive-behavioral therapy but eventually produced similar results (
19). The IPT approach to affective attunement also evokes Cloitre and colleagues’ PTSD treatment study (
49), in which initial affective attunement and social skills training (based on dialectal behavioral therapy principles rather than IPT) preceding exposure therapy benefited patients more than exposure therapy alone.
Researcher allegiance can influence study outcomes (
34,
50). This study’s principal investigator (J.C.M.) has IPT links; it is possible that some patients entered the study seeking IPT. This seems unlikely, however, given their evident lack of psychotherapeutic knowledge at study entry and our PTSD clinic’s historical specialization in prolonged exposure treatment (
14). The principal investigator encouraged friendly rivalry (
34) among the expert-supervised therapy teams. In a previous, prolonged exposure-allegiant PTSD trial (
14), the prolonged exposure therapists achieved comparable results: a 45% response rate, compared with 44%, using identical criteria (F.R. Schneier, personal communication, October 2013), and a 29% dropout rate, compared with 28%. Our study findings of prolonged exposure superiority over relaxation therapy confirm assay sensitivity.
Study strengths include matched rival teams of dedicated, allegiant psychotherapists. Few previous PTSD trials have defined response or remission a priori. The proscription of pharmacotherapy in the treatment sample eliminated the confounders of undocumented pharmacotherapy dosage changes and of potential psychotherapy-pharmacotherapy interactions. On the other hand, proscribing pharmacotherapy very likely contributed to the study limitation in sample size by excluding patients who were receiving psychopharmacotherapy. We felt it inappropriate to stop patients’ antidepressant medications, which, even if ineffective for PTSD, might benefit depressive or anxiety symptoms. A larger sample would have increased statistical power to test between-treatment differences. The unmedicated status of this patient sample may also limit the generalizability of our findings. A further limitation is our failure to complete two session adherence ratings on every treatment dyad, although all of those we rated were adherent.
The hypothesized a priori margin of 12.5 CAPS points to define “not more than minimal inferiority” between prolonged exposure and IPT was derived from a literature review (e.g.,
35) and statistical estimation based on our pilot data (
18). Our empirical CAPS data suggest a much narrower (5.5-point) clinical difference between the two treatments. The effect of the smaller than intended sample size on testing this hypothesis is that it increased the probability of type II error, that is, of not rejecting the null hypothesis when it is false. Here it means that there was a >20% chance of failing to reject the null hypothesis that IPT is more than minimally inferior to prolonged exposure when in fact IPT was not more than minimally inferior. The smaller sample size may also be responsible for our failing to find differences between IPT or prolonged exposure against relaxation therapy in some outcomes. Finally, although even the planned sample size did not allow sufficient power to detect clinically meaningful treatment effect moderators, the smaller than intended sample size further reduced power for moderation hypotheses.
The findings of this comparative trial require replication in combat veterans (only two of our 110 participants were veterans) and other PTSD populations, and at other treatment centers with differing treatment allegiances. Treatment mechanisms require further exploration. In any case, having another potentially efficacious treatment will benefit patients with PTSD.
Acknowledgments
The authors thank the many individuals who contributed to this project: therapists (Drs. L. Amsel, E. Graf, D. Gross, M. Kaplowitz, E. MacGregor, J. Page, H. Pessin, A. Rafaeli, E.J. Suh), evaluators (Drs. Elliot, Houston, Nasereddin, Surbaugh), research assistants, Ms. Helena Rosenfeld, volunteers, members of the data safety monitoring board (Drs. W. Bilker, J. Barber, M. Olfson), the personnel of the New York State Psychiatric Institute Anxiety Disorders Clinic, and the patients who participated in the trial.