The rates of active-duty service members receiving psychiatric diagnoses increased over 60% during more than a decade of war in Iraq and Afghanistan (
1). Not surprisingly, rates of suicide ideation and attempts, as well as deaths by suicide, demonstrated comparable increases (
2,
3). Elevated suicide risk has been shown to endure well beyond military service, with veterans carrying a much greater risk for suicide than individuals in comparable civilian populations (
4).
Suicidal thoughts and previous suicide attempts are among the most significant risk factors for death by suicide in adults (
5). Given the variable nature of symptoms associated with suicide risk (e.g., depression, anxiety and hopelessness, substance abuse), arguably the most accurate and impactful marker of decreased risk after treatment is a reduction in the incidence of follow-up suicide attempts (
5). To date, however, only a handful of treatments have demonstrated efficacy for reducing posttreatment suicide attempt rates, with a number of comprehensive reviews available (
6,
7) indicating that cognitive-behavioral treatments, such as dialectical-behavior therapy (
8,
9) and cognitive therapy (
10), offer the most promise, particularly beyond 1 year of follow-up. Of these effective treatments, one common element is a focus on emotion-regulation skills training (
6). Although evidence-based interventions for treating suicidal behavior exist, these approaches have yet to be implemented and evaluated in active-duty military personnel (
11). Treatment in a military environment offers a number of unique challenges that differ from traditional clinical settings. In these circumstances, two primary issues are flexibility and brief duration, both of which are essential for successful implementation within the high-tempo, fluid, and unpredictable military system.
The present study is a randomized controlled trial examining the effectiveness of treatment as usual compared with treatment as usual supplemented with brief cognitive-behavioral therapy (CBT) (
11) for recent suicidal ideation and/or recent suicide attempt in active-duty military personnel. Brief CBT differs from treatment as usual because it 1) is purposefully brief to accommodate the time demands of a military setting, 2) incorporates the common elements of effective treatments, 3) is focused on skills development, 4) considers suicide risk as distinct from diagnosis and a function of a core skills deficit, and 5) emphasizes internal self-management (
11). The primary aim was to determine whether brief CBT significantly reduced posttreatment suicide attempt rates during the 24-month follow-up period. To this end, the first hypothesis was that the hazard ratio for a subsequent suicide attempt would be significantly lower in the brief CBT group compared with the treatment as usual group, and the second hypothesis was that the proportion of soldiers making a suicide attempt during follow-up would be significantly lower among those receiving brief CBT compared with those receiving treatment as usual.
Method
Participants and Procedures
Participants were 152 active-duty soldiers identified during weekly behavioral health treatment team meetings and daily emergency department reports at Fort Carson, Colo., and referred to research assistants for determination of eligibility. All soldiers admitted to inpatient psychiatric hospitalization for suicidal ideation with intent or for a suicide attempt from January 2011 to September 2012 were referred to research assistants upon discharge for determination of eligibility. Inclusion criteria were the presence of suicidal ideation with intent to die during the past week and/or a suicide attempt within the past month, active-duty military status, age ≥18 years, ability to speak English, and ability to understand and complete informed consent procedures. Soldiers were excluded if they had a medical or psychiatric condition that would preclude informed consent or participation in outpatient treatment, such as active psychosis or mania. The failure to register the trial before enrollment was due to an oversight of the principal investigator. The original grant proposal to demonstrate that the methods and procedures reported in this study are consistent with the original design and plan for the trial are available upon request from the authors.
A suicide attempt was defined as behavior that is self-directed and deliberately results in injury or the potential for injury to oneself for which there is evidence, whether implicit or explicit, of suicidal intent (
12). The Suicide Attempt Self-Injury Interview (
13) was used to determine the occurrence of suicide attempts, and the Beck Scale for Suicide Ideation (
14) was used to determine the presence of suicidal ideation within the past week. For those experiencing suicidal thoughts with intent to die, a total score ≥5 on the Beck Scale for Suicide Ideation was used as the cutoff score for study inclusion. Study procedures were explained to soldiers who met eligibility criteria, and written informed consent was obtained. The study’s procedures were reviewed and approved by the institutional review board of the Madigan Army Medical Center.
Randomization
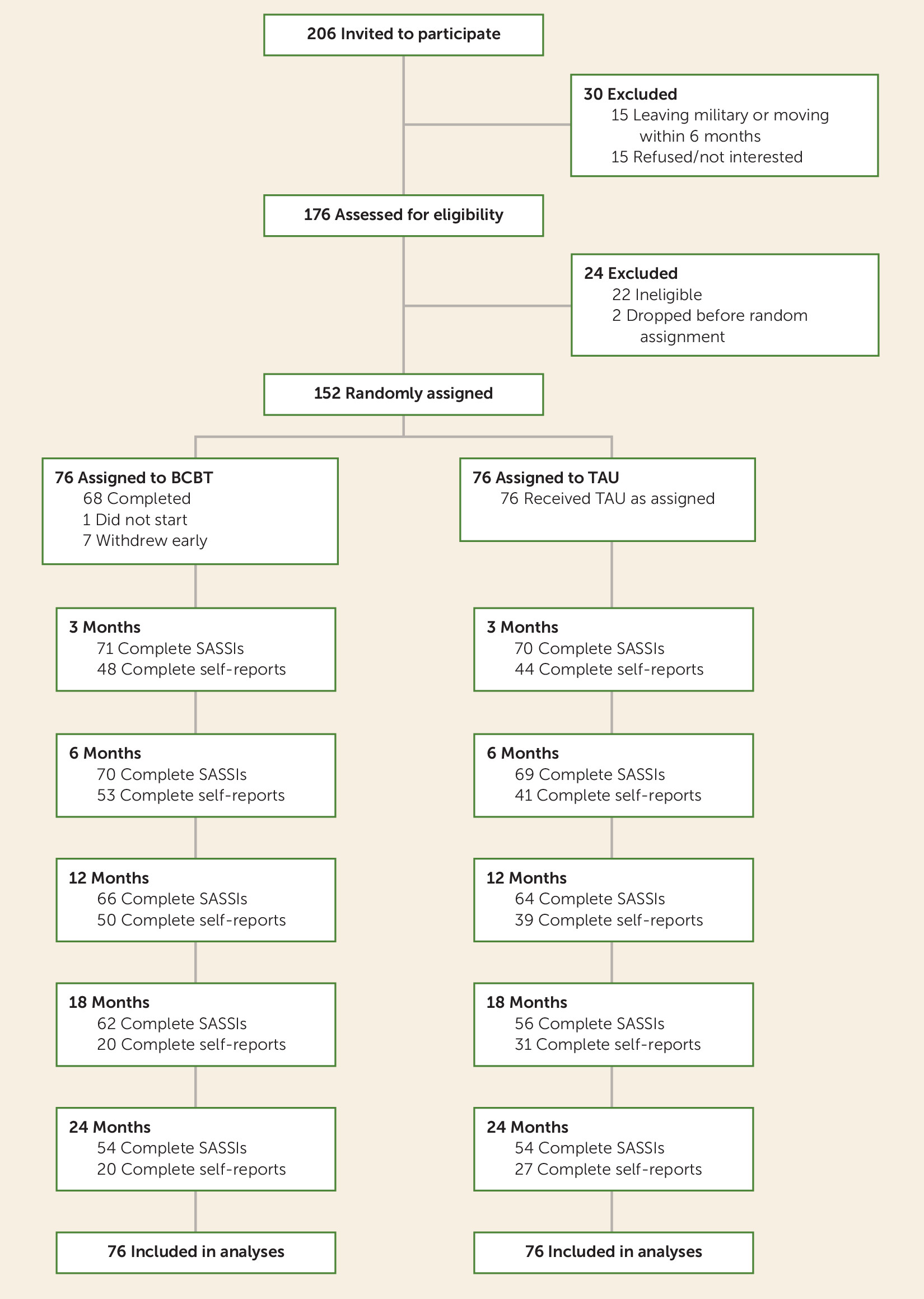
Participants were randomly assigned to either brief CBT (N=76) or treatment as usual (N=76) using a computerized randomization program created based on the RANUNI function available in the SAS software (SAS Institute, Cary, N.C.), constrained to produce equal numbers across groups. The flow chart of participants through the study is presented in
Figure 1. Participants were allowed to continue all other forms of mental health and substance abuse treatment while participating in this research study across both the brief CBT and treatment as usual arms.
Assessments
The baseline assessment, including clinician-administered interviews and self-report measures, was completed within 2 weeks of referral and prior to random assignment to treatment condition. Follow-up interviews to assess the incidence and date of subsequent suicide attempts and the incidence and severity of suicidal ideation were conducted by telephone or in person at 3, 6, 12, 18, and 24 months after baseline assessment by an independent, trained evaluator with a master’s degree, who was blind to treatment condition. The independent evaluator was trained on interview measures and then supervised and evaluated for reliability using video-recorded sessions reviewed by a lead investigator (C.J.B.). Agreement between the two raters was very good (κ=0.96). Participants completed follow-up self-report assessments of symptom severity in person at 3, 6, 12, 18, and 24 months.
Psychiatric diagnosis.
The Structured Clinical Interviews for Axis I and Axis II DSM-IV Disorders (
15) were used to determine the presence of current psychiatric diagnoses.
Outcome measures.
The primary outcome was the occurrence of suicide attempts during the follow-up period based on Suicide Attempt Self-Injury Interview scores. The Suicide Attempt Self-Injury Interview is a validated clinician-administered interview that assesses the characteristics of self-injurious behaviors, including suicide intent, desired and expected outcome, and medical severity of the suicide attempt. Consistent with this expectation, the Suicide Attempt Self-Injury Interview detected many more suicide attempts (N=26 out of 31 attempts) than were documented in the medical record (N=5 out of 31 attempts). The intensity of current (i.e., past week) and worst-point suicidal ideation since the previous assessment period was measured using the 19-item self-report Beck Scale for Suicide Ideation. Worst-point suicidal ideation was measured separately from current suicidal ideation based on previous research indicating that worst-point suicidal ideation is a stronger indicator of current and future risk for suicide attempts than current suicidal ideation (
16). Depression severity was assessed with the 21-item self-report Beck Depression Inventory-II (
17). Anxiety symptom severity was assessed with the 21-item Beck Anxiety Inventory (
18). Severity of hopelessness was assessed with the 20-item Beck Hopelessness Scale (
19). Posttraumatic stress symptom severity was assessed with the 17-item PTSD Checklist-Military version (
20).
Treatment Conditions
Treatment as usual.
Participants in both treatment conditions received usual care from military mental health clinicians as well as nonmilitary mental health clinicians in the local community. Treatment as usual included individual and group psychotherapy, psychiatric medication, substance abuse treatment, and/or support groups, as determined by participants’ primary mental health care providers, who were licensed military psychologists and psychiatrists. The specific types and amount of interventions received are described in the Results section. In order to facilitate follow-up research, staff obtained approval from participants to maintain detailed contact information (i.e., name, telephone number, e-mail address, mailing address) for at least two family members, friends, or peers who could be contacted in the event participants could not be reached or located. Research staff also used the military’s electronic medical record and coordinated with military providers and case managers to track participants over time and to assist with scheduling follow-up assessments. All additional mental health, substance abuse, and medical treatments were provided within the military health care system at no cost to participants.
CBT.
In addition to treatment as usual, participants in brief CBT were scheduled to receive 12 outpatient individual psychotherapy sessions on a weekly or biweekly basis, with the first session lasting 90 minutes and subsequent sessions lasting 60 minutes. Upon completion of brief CBT, participants were allowed to choose whether they wanted to continue individual psychotherapy with another mental health provider. Brief CBT was designed to be delivered in three phases. In phase I (five sessions), the therapist conducted a detailed assessment of the patient’s most recent suicidal episode or suicide attempt, identified patient-specific factors that contribute to and maintain suicidal behaviors, provided a cognitive-behavioral conceptualization, collaboratively developed a crisis response plan, and taught basic emotion-regulation skills such as relaxation and mindfulness. The crisis response plan was reviewed and updated in each session by adding new skills and/or removing skills determined to be ineffective, impractical, or too challenging. In phase II (five sessions), the therapist applied cognitive strategies to reduce beliefs and assumptions that serve as vulnerabilities to suicidal behavior (e.g., hopelessness, perceived burdensomeness, guilt and shame). In phase III (two sessions), a relapse prevention task was conducted, in which patients imagined the circumstances of a previous suicidal episode and the internal experiences associated with this event (i.e., thoughts, emotions, and physiological responses) and then imagined themselves using one or more skills learned in brief CBT to successfully resolve the crises. Therapists helped to increase the emotional salience and intensity of this task by verbalizing patients’ suicide-related thoughts, images, and emotions, which were previously discussed during treatment. Because progress through brief CBT is based on demonstrated competency and skill mastery, participants had to demonstrate the ability to successfully complete this task in order to terminate the treatment. Additional sessions were conducted until participants demonstrated the ability to successfully complete this task (
21).
During the first session of brief CBT, participants were provided with a small pocket-sized notebook (called a “smart book”) in which they were directed to record a “lesson learned” at the conclusion of each session. Lessons learned included new skills learned or knowledge gained by participants during each session. Smart books were reviewed during phase III, and participants were encouraged to use the smart book in the future as a memory aid for managing emotional distress and solving problems. The smart book contained participants’ relapse prevention plans. All brief CBT sessions were video recorded and observed by the investigators (C.J.B. and M.D.R.) using a fidelity checklist. Therapists participated in a 2-week training program with one of the treatment developers (C.J.B.) and were rated for competency using the Cognitive Therapy Rating Scale (
22). In order to maintain treatment fidelity, feedback was provided by the trainer to the research therapists at least twice per week during individual and group supervision to ensure that the therapists adhered to the brief CBT manual; both therapists achieved >90% fidelity ratings.
In order to maximize generalizability to the military setting, research therapists were credentialed as clinical providers in the military hospital and conducted all study procedures within the military medical system consistent with military and local requirements for patient care. Research therapy sessions were also documented in the military’s electronic medical record.
Statistical Analysis
All analyses were conducted with SAS 9.3 software (SAS Institute, Cary, N.C.) using an intent-to-treat approach, which included all participants randomly assigned to each treatment condition regardless of adherence, amount of treatment received, and/or attrition during follow-up assessments. To determine the effectiveness of brief CBT compared with treatment as usual, univariate and multivariate Cox proportional hazard regression models were used to analyze time to the first suicide attempt. Time to suicide attempt was measured by calculating the total number of days from enrollment to the first suicide attempt. For participants without a suicide attempt, the total number of days from enrollment to the last assessment was calculated. The Cox regression model was selected because it utilizes all available data from all participants regardless of the dropout rate or length of follow-up, which is consistent with the intent-to-treat principle. Estimates of the proportions of participants in each treatment group making at least one suicide attempt during the 24-month follow-up period were calculated using the Kaplan-Meier method, which similarly accounts for individuals who drop out and limited follow-up. To determine the effectiveness of brief CBT compared with treatment as usual for suicidal ideation, depression, anxiety, hopelessness, and posttraumatic stress symptoms, longitudinal mixed-effects models with random effects were used, which allows for the estimation of changes in repeated measures over time despite missing data. To compare group differences at each follow-up assessment, the longitudinal random-effects models included the main effects and interaction terms of treatment group and time, using data from all participants regardless of treatment adherence or early dropout. An autoregressive covariance structure was selected because of expected intercorrelations of measures at each follow-up assessment.
Power Analysis and Missing Data
Because participants were active-duty military personnel with high mobility related to reassignments, deployments, training, and medical separations, high attrition was expected. A priori power analyses were therefore conducted for the proposed survival analysis and mixed-effects longitudinal models to account for an assumed 4.5% attrition per month (i.e., 60% attrition overall at 24 months). Based on estimates from previous studies (
8–
10), we assumed that the suicide attempt rate in the brief CBT group (20%) would be one-half the suicide attempt rate in the treatment as usual group (40%) during follow-up. Power for a survival analysis predicting time to first suicide attempt was adequate (0.81) for a two-tailed alpha set at 0.05 with N=75 per treatment arm. Assuming no attrition, power was 0.94. For longitudinal mixed-effects models with an autoregressive covariance structure assuming r=0.50, N=75 per treatment arm yielded sufficient power (0.80) for a medium-sized two-tailed standardized mean difference (d=0.50) with an alpha set at 0.05. Assuming no attrition, power was 0.90.
To minimize the effect of attrition on the primary outcome variable (suicide attempts), follow-up assessment interviews were primarily conducted by telephone. A much larger number of participants were unable to complete self-reported symptom measures at the same time as the requested follow-up interviews (see
Figure 1). Because of the higher than planned attrition rate during later follow-up assessments, only self-reported data from baseline to the 18-month follow-up assessment were used. Results and conclusions were unchanged when analyzing only the self-reported data from baseline to the 12-month follow-up assessment, which indicate much fewer missing data; results up to the 18-month follow-up assessment are therefore presented. Analysis of missing data patterns indicated that self-reported data were missing completely at random for both treatment conditions (Little’s missing completely at random test: χ
2>12.57, df=10, p>0.25). Missingness was therefore handled with maximum likelihood estimation and multiple imputation of 10 data sets. There were no differences between analyses conducted with the original data set and the multiply imputed data set. Results based only on the original data set are therefore reported. Because the worst-point and current scores on the Beck Scale for Suicide Ideation had increasingly severe positive skew at each follow-up assessment, analyses for these two variables were repeated with 1) approximate bootstrapping with 1,000 resamples and 2) assuming zero-inflated distributions. Results did not differ from those obtained from the longitudinal random-effects models. To compare differences in treatment utilization, generalized mixed-effects models for count models were used.
Results
Sample Characteristics and Baseline Treatment Differences
The treatment groups did not significantly differ from each other at baseline on any of the demographic variables, military-specific characteristics, psychiatric diagnoses, history of previous suicide attempts, or medications. Demographic and clinical characteristics of participants are summarized in
Table 1.
Dropout Rates and Missing Data
The difference between the two treatment conditions in study dropout was not significant (χ2=1.85, df=1, p=0.17) (brief CBT group: N=5 [6.4%]; treatment as usual group: N=10 [13.2%]. Eight (11.1%) participants in brief CBT withdrew from treatment early (before the first session, N=1; before the relapse prevention task, N=7).
Suicide Attempts
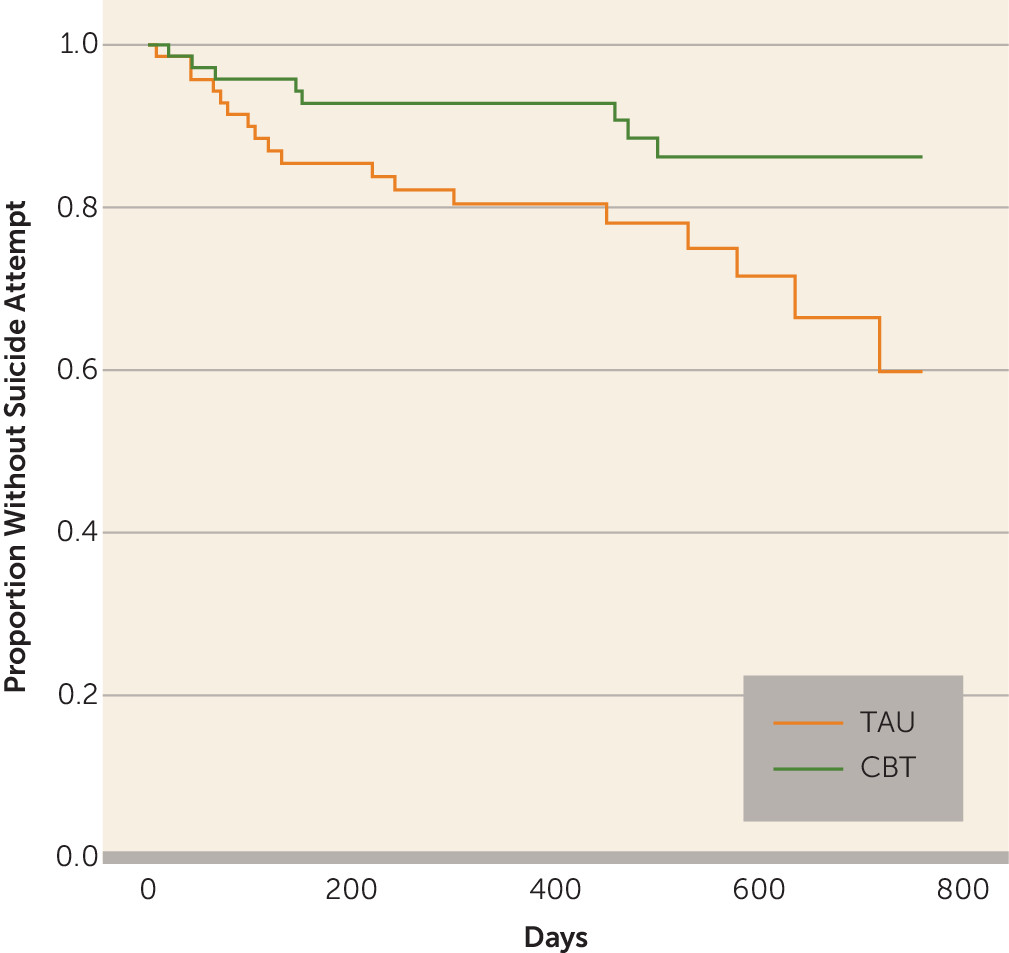
A total of 31 suicide attempts were made by 26 participants across both groups during the 2-year follow-up period, including two deaths by suicide (one in the brief CBT group and one in the treatment as usual group). Eight participants in brief CBT (estimated proportion: 13.8%) and 18 participants in treatment as usual (estimated proportion: 40.2%) made at least one suicide attempt during the 2-year follow-up period (Wald χ
2=5.28, df=1, p=0.02, hazard ratio=0.38, 95% confidence interval [CI]=0.16–0.87, number needed to treat=3.88), which suggests that soldiers in brief CBT were approximately 60% less likely to make a suicide attempt during the follow-up period than soldiers in treatment as usual. The Kaplan-Meier survival curves for both treatment groups are displayed in
Figure 2. Results indicated that participants in brief CBT were significantly less likely to make a suicide attempt during follow-up than participants in treatment as usual (log-rank χ
2=5.71, df=1, p=0.02). Results of the multivariate Cox regression revealed that treatment effects remained even when controlling for the effects of other risk factors (i.e., previous suicide attempts, depression, anxiety, posttraumatic stress, hopelessness, and suicidal ideation) at baseline (Wald χ
2=6.66, df=1, p=0.01, hazard ratio=0.31, 95% CI=0.13–0.75). The estimated proportions without a repeat suicide attempt in brief CBT and treatment as usual are presented in
Table 2. A significant difference between groups was observed as early as 6 months postbaseline and increased in magnitude over the 2-year follow-up period. The number needed to treat value of 3.88 indicated that approximately four soldiers had to be treated with brief CBT to have one fewer suicide attempt during follow-up compared with treatment as usual.
Analyses were repeated among participants with a history of suicide attempt at baseline (treatment as usual: N=57; brief CBT: N=59). Results indicated that participants in brief CBT (N=6, estimated proportion: 12.7%) were significantly less likely to make a follow-up suicide attempt than participants in treatment as usual (N=14, estimated proportion: 36.8%), even when controlling for other risk factors (Wald χ2=5.35, df=1, p=0.02, hazard ratio=0.30, 95% CI=0.11–0.83; log-rank χ2=4.95, df=1, p=0.03).
Secondary Outcome Measures
The effect of brief CBT compared with treatment as usual on suicidal ideation and symptoms of hopelessness, depression, anxiety, and posttraumatic stress was also examined from baseline to 18 months (see
Table 3). Results indicated no significant between-group differences over time in worst-point suicide ideation (F=1.66, df=1, 357, p=0.20), current suicide ideation (F=0.51, df=1, 357, p=0.48), hopelessness (F=0.59, df=1, 190, p=0.44), depression (F=0.33, df=1, 190, p=0.57), anxiety (F=0.01, df=1, 190, p=0.93), and posttraumatic stress (F=1.29, df=1, 190, p=0.26). The bias-corrected Hedge’s g statistic was also calculated at each time point for between-group effect-size estimation. Results indicated that worst-point suicidal ideation and current suicidal ideation declined across both treatments, with the magnitude of decline being larger among participants in brief CBT, who reported significantly less severe worst-point (F=4.96, df=1, 357, p=0.02) and current (F=3.86, df=1, 358, p=0.05) suicidal ideation at the 6-month follow-up assessment. In terms of depression, anxiety, and posttraumatic stress symptoms, the Hedge’s g values indicated larger declines among participants in brief CBT, although none of the between-group differences were statistically significant.
Treatment Utilization
On average, participants in brief CBT attended a mean of 11.75 (SD=4.01) sessions. Twenty-one (27.6%) participants attended nine or fewer brief CBT sessions; 12 (15.8%) attended nine to 11 sessions; eight (10.5%) attended 12 sessions; 14 (18.4%) attended 13–15 sessions; and 11 (14.4%) attended 16 or more sessions. A total of 59 (77.6%) participants in brief CBT received additional treatment of some kind during the follow-up period after completing brief CBT. In terms of overall treatment received (i.e., including both treatment as usual and brief CBT sessions), there were no differences in the overall amount of treatment received between groups during the first 3 months of the study (see
Table 4). There were also no differences between groups in terms of the total treatment received during the 2-year follow-up period, with the exception of hospitalization days, which were significantly fewer among participants in brief CBT (mean=3.14 [SD=7.83] days compared with mean=8.32 [SD=17.97] days; χ
2=7.55, df=1, p=0.006).
Military Career Outcomes
The Medical Evaluation Board is involved in the process designed to determine whether a service member’s medical condition enables him or her to continue to meet medical retention standards. Medical evaluation boards are typically initiated for service members with severe medical or psychiatric conditions that are chronic and/or believed to be persistent, and such conditions can result in medical retirement from the military. A decreased likelihood for medical retirement that fell short of statistical significance was observed among participants in brief CBT compared with participants in treatment as usual (26.8% compared with 41.8%; odds ratio=0.51, 95% CI=0.25–1.04, p=0.06).
Discussion
Consistent with our hypotheses, results of this randomized clinical trial demonstrated that brief CBT was effective in preventing suicide attempts among active-duty soldiers who were experiencing suicidal ideation with intent and/or had made a suicide attempt during the month immediately preceding treatment. More specifically, soldiers in brief CBT were approximately 60% less likely to make a suicide attempt during the 2-year follow-up period than soldiers in treatment as usual, which, to our knowledge, is the largest reduction in suicide attempt risk to date. Furthermore, soldiers in brief CBT were somewhat less likely to be medically retired from the military, although this finding fell short of the threshold for statistical significance. Additional research is needed to determine whether brief CBT may also have a positive effect on military readiness and social-occupational outcomes.
It is noteworthy that the observed reduction in suicide attempts occurred despite minimal differences in symptom severity between groups over time, a finding that mirrors previous outcomes from dialectical-behavior therapy (
8,
9) and cognitive therapy (
10). Given that the primary goal of brief CBT is emotion regulation and problem-solving skills development as opposed to symptom reduction, this finding is not surprising and supports the assertion that suicidal thoughts and behaviors should be targeted as a unique treatment goal separate from psychiatric diagnosis and symptom severity. In other words, effective treatment of risk for suicidal behavior does not require complete remission of a psychiatric diagnosis or symptom severity but rather the development of core skills in the areas of emotion regulation, interpersonal functioning, and cognitive restructuring. The present findings therefore extend previous findings from nonmilitary settings to military personnel and suggest that these skills can be taught to suicidal military personnel in a relatively brief period of time with reduced utilization of inpatient psychiatric care. This has significant implications for military health care costs. To this end, our findings suggest that targeted outpatient treatment can be effective for high-risk military personnel while maintaining sufficient safety, compared with treatment approaches that utilize inpatient hospitalization more frequently. Furthermore, these results suggest that a focus on psychiatric symptom severity as a primary clinical outcome for actively suicidal military personnel may be insufficient and may not be the most effective strategy for recovery.
This study is not without limitations. First, the sample was comprised of active-duty soldiers only, and therefore results may not generalize to military personnel in other branches of service or to veterans no longer in military service. Second, because the sample was predominantly male, conclusions about effectiveness with female soldiers should be made with caution. Additional studies targeting female soldiers are needed. Finally, although the follow-up rate for our primary outcome variable, suicide attempts, was very good, there was considerable attrition for follow-up self-reported measures because of the highly mobile nature of military personnel, which prohibited participants from following up in person (e.g., being deployed, reassigned to a different base, moving away after leaving military service). Conclusions specific to treatment effects on psychiatric symptom severity should therefore be made cautiously until additional studies can be conducted. Despite these limitations, our results suggest that a brief, time-limited outpatient treatment that specifically focuses on skills training can be effectively implemented in a military setting and can reduce suicide attempts among military personnel who have made a suicide attempt or are currently experiencing suicidal thoughts with intent to die.