Early intervention in psychosis now arguably represents the gold standard of care for people in their first episode of psychosis (
1). This care model incorporates pharmacological and psychological interventions, family and social support, supported employment, and physical health care checks delivered by a multidisciplinary team for up to 5 years. The rationale for early intervention derives from observations that reducing the duration of untreated psychosis may improve clinical, functional, and social outcomes in the short- to medium-term (
2–
8). This effect is most robust for schizophrenia spectrum disorders (
2–
4), with much less evidence in regard to affective psychoses (
9). Since early intervention psychosis service provision is founded on evidence-based health care (
10), this should include the provision of robust estimates of incidence of psychotic disorders to inform health care commissioners about local variation in service need. Unfortunately, psychosis epidemiology is predominantly informed by an older literature, conducted prior to the widespread introduction of these services (
11,
12), almost exclusively based in urban settings (
13). This research has revealed important heterogeneity in incidence by person (
14–
18) and place (
19,
20), generating new directions for etiological research (
21–
23). However, national implementation efforts being developed in countries such as Denmark (
24), Australia (
25), and Canada (
26), and currently undergoing revision in the United Kingdom (
27), require accurate, relevant estimates about the epidemiology of psychotic disorders in populations served by early intervention psychosis services. Such data will also be critical in countries such as the United States, where early intervention initiatives are gaining traction (
28–
31) but where little recent epidemiological data exist to inform service provision.
To address this gap, we established a naturalistic cohort study, known as the Social Epidemiology of Psychoses in East Anglia (SEPEA) study, in a diverse, mixed rural and urban setting in the East of England. We sought to precisely delineate the epidemiology of psychotic disorders since the introduction of early intervention psychosis services. Consistent with earlier epidemiology (
11,
13), we hypothesized that the incidence of psychotic disorders, including nonaffective psychoses, would decline with age and greater socioeconomic status and be higher among men, in black and minority ethnic groups, and in more deprived, urban neighborhoods. In line with previous findings (
13,
20), we also hypothesized that affective psychoses would show less variation across these domains.
Method
Design and Setting
We identified all persons aged 16–35 years old who presented to six early intervention psychosis services in a defined catchment area over 3.5 years from August 1, 2009. These services were implemented on the basis of a national implementation guide (
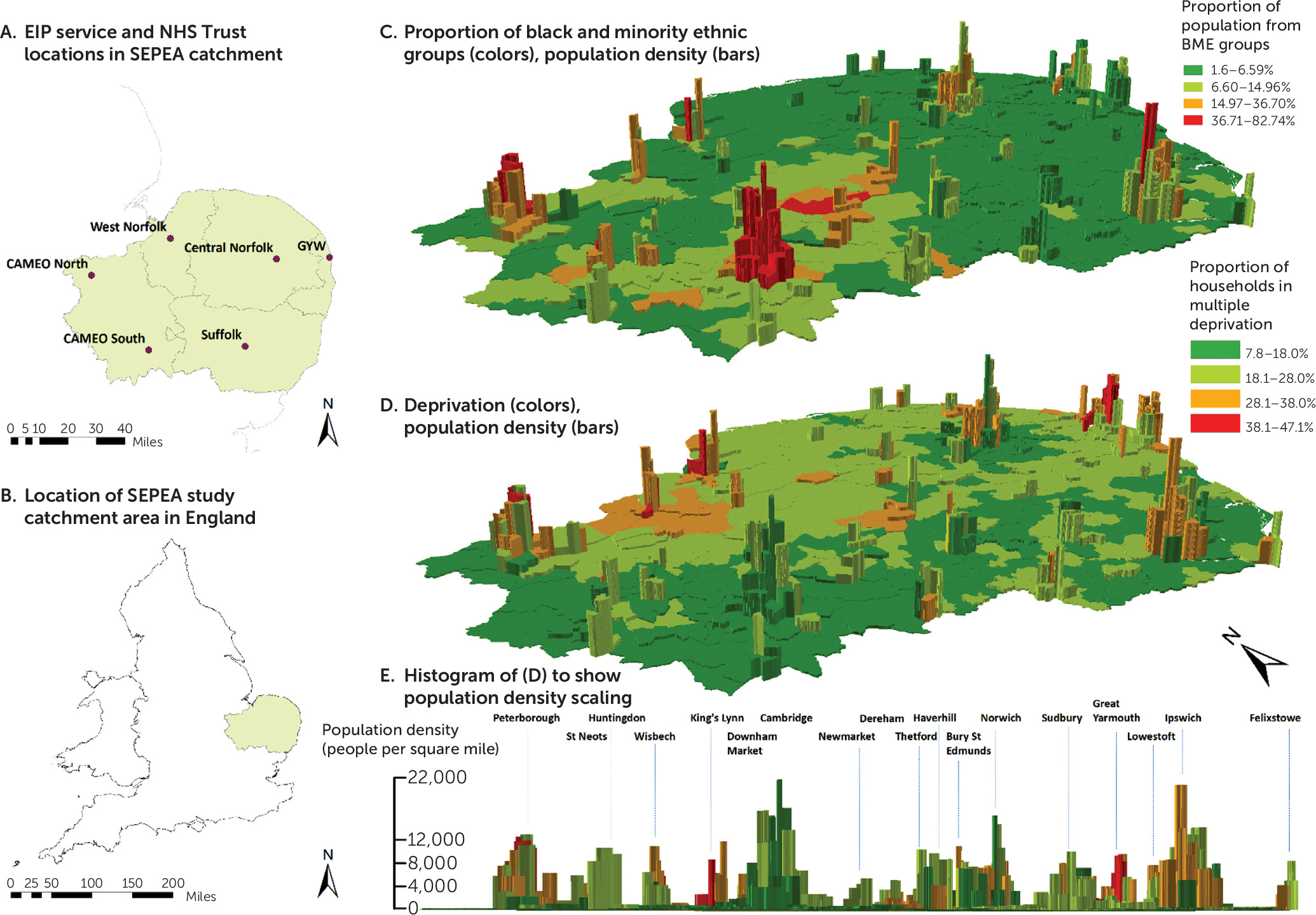
32) as the sole referral point for suspected psychosis for people up to 35 years old. Services accepted referrals from several sources, including self-referral, primary care, schools, universities, police and judicial services, and other mental health services. The catchment area was concomitant with the boundaries of the Cambridgeshire and Peterborough National Health Service (NHS) Foundation Trust and Norfolk and Suffolk NHS Foundation Trust (see
Figure 1). In 2011, the catchment area had an estimated population of 2.4 million people (4.5% of the English population) (
33), of whom 24.0% were 16–35 years old. The catchment area contained 530 administrative neighborhoods with a median population of 3,992 people (interquartile range: 2,426–5,935). The region is varied in terms of its sociodemographic characteristics and population density (see
Figure 1).
Inclusion Criteria
We applied the following inclusion criteria to all participants referred to early intervention psychosis services in our study:
1.
Acceptance into care because of suspected psychosis.
2.
16–35 years old (17–35 years old in “Cambridgeshire North” and “Cambridgeshire South” services).
3.
Resident in the catchment area, including those of no fixed abode.
4.
Absence of moderate or severe learning disability, or an organic basis to disorder.
5.
No previous contact with health services for psychotic disorder.
We collected baseline sociodemographic data on all participants who met these criteria (henceforth, the “incepted sample”), irrespective of later diagnosis. We followed incepted participants from referral until receipt of 3 years of care, or discharge from the service, if earlier.
Diagnostic Outcomes
We used a two-stage diagnostic procedure to confirm presence of an ICD-10 F10–F33 diagnosis. In the first stage, we asked the clinician responsible for care to provide a clinical diagnosis 6 months after acceptance into care and at service discharge (median follow-up: 2.3 years; interquartile range: 1.2–3.0). In the second stage, we obtained research-based diagnoses at these time points using OPCRIT [operational criteria for psychotic illness] (
34), a reliable diagnostic instrument (
34,
35) that produces ICD-10 diagnoses according to 90 standardized symptom items (
36). We trained a panel of clinicians (N=25) to rate OPCRIT items from available case note information. Excellent interrater reliability was achieved for any clinically relevant psychotic disorder (F10–F33: 92% agreement; interquartile range: 92–100) and specific diagnoses (85%; interquartile range: 81–90), based on completion of 20 case vignettes. Incepted participants were included in our incidence sample if they received an ICD-10 clinical diagnosis of psychotic disorder (F10–F33) at either time point, confirmed by OPCRIT assessment.
We classified participants according to their final OPCRIT diagnosis as follows: all clinically relevant psychotic disorders (F10–F33), nonaffective psychoses (F20–F29), schizophrenia (F20), other nonaffective psychoses (F21–F29), substance-induced psychoses (F10–F19), affective psychoses (F30–F33), bipolar disorder (F30–F31), and psychotic depression (F32–F33). Since OPCRIT does not distinguish substance-induced psychoses from other nonaffective psychoses, we relied on a clinical diagnosis of substance-induced psychosis at 6 months after acceptance (N=8), discharge (N=1), or both (N=21) for people who received an OPCRIT diagnosis of “ICD-10 other nonorganic psychoses” (i.e., F21–F29 and F1×0.5). Incepted participants without any OPCRIT-confirmed psychotic disorder were excluded from the incidence sample (
Figure 2).
Exposure and Confounder Variables
Sociodemographic information, including birthdate, sex, ethnicity, marital status, birth country, postcode, employment status, and main, current/last occupation, as well as parental occupations, was collected at first referral, using a standardized form. We classified age into seven categories (ages 16–17, 18–19, 20–22, 23–25, 26–28, 29–31, 32–35) to permit fine-grained estimation of incidence by age and sex. Marital status was classified as single, married/civil partnership, or widowed/divorced/dissolved. Ethnicity was self-ascribed to one of 18 categories from the 2011 Census of Great Britain. Here, we created a dichotomous ethnicity variable (black and minority ethnic groups compared with white British) to examine initial variation. We classified birth country as United Kingdom-born or foreign-born. We classified participant socioeconomic status according to current or, if unemployed for less than 2 years, main or last occupation, according to a standard methodology (
37,
38) as follows: professional and managerial occupations, intermediate occupations (including small employers and self-employed), routine and manual occupations, and those not employed (long-run unemployed, never worked, students, otherwise unclassifiable). We coded parental socioeconomic status similarly, taking the higher occupation of both parents, where available.
We geocoded participants to their neighborhood of residence at initial referral to obtain measures of their social environment. We defined multiple deprivation as the proportion of households in each neighborhood classified as deprived on at least two of four indicators from the 2011 census (employment, education, health, and living environment; also see Table S1 in the online data supplement). We categorized multiple deprivation on an equal-interval scale (7.7%−18%, 18.1%−28%, 28.1%−38%, 38.1%−47.1%). We estimated population density for each neighborhood based on the total 2011 census population divided by area, expressed as people per square mile. We categorized population density according to the proportion of neighborhoods 1) below the median (48–587 people per square mile), 2) in the 50th–75th percentile (588–4,653 people per square mile), 3) in the 76th–95th percentile (4,654–11,099 people per square mile), and in the 96th–100th percentile (11,100–21,970 people per square mile).
At-Risk Population
The usual resident population at risk, including students, was estimated from the 2011 census, conducted April 1, 2011, which coincided with the midpoint of case ascertainment. We multiplied population estimates by 3.5 to obtain person-years at risk over the study period and stratified the data by age group (16–24 years old, 25–29 years old, 30–35 years old), sex, ethnicity, and participant socioeconomic status.
Statistical Analyses
We first reported descriptive epidemiological characteristics of the sample, including crude incidence rates for each psychotic outcome and 95% confidence intervals. We used two-tailed chi-square, Mann-Whitney, and Kruskal-Wallis chi-square tests to analyze differences in sociodemographic characteristics between cases and the population at risk. For all psychotic disorders (F10–F33), nonaffective psychoses (F20–F29), and affective psychoses (F30–F33), we then fitted multivariable Poisson regression models to examine potential differences in incidence by age group (three-category), sex, ethnicity, participant socioeconomic status, and early intervention psychosis service setting, after mutual adjustment for all remaining variables. Forward-fitting modeling was used to determine the most parsimonious model, assessed via likelihood ratio test. Where variation in incidence between services was detected, we then examined whether this was attributable to multiple deprivation or population density, using multilevel Poisson models, fitted with neighborhood-level random intercepts. In these analyses, we excluded participants of no fixed abode (N=28). Incidence rates were presented per 100,000 person-years. Analyses were conducted using Stata version 13 (StataCorp, College Station, Tex.).
Ethics
Ethical approval was granted by the Cambridgeshire III Local Research Ethics Committee (09/H0309/39).
Results
Case Ascertainment and Crude Rates, by Contact Type
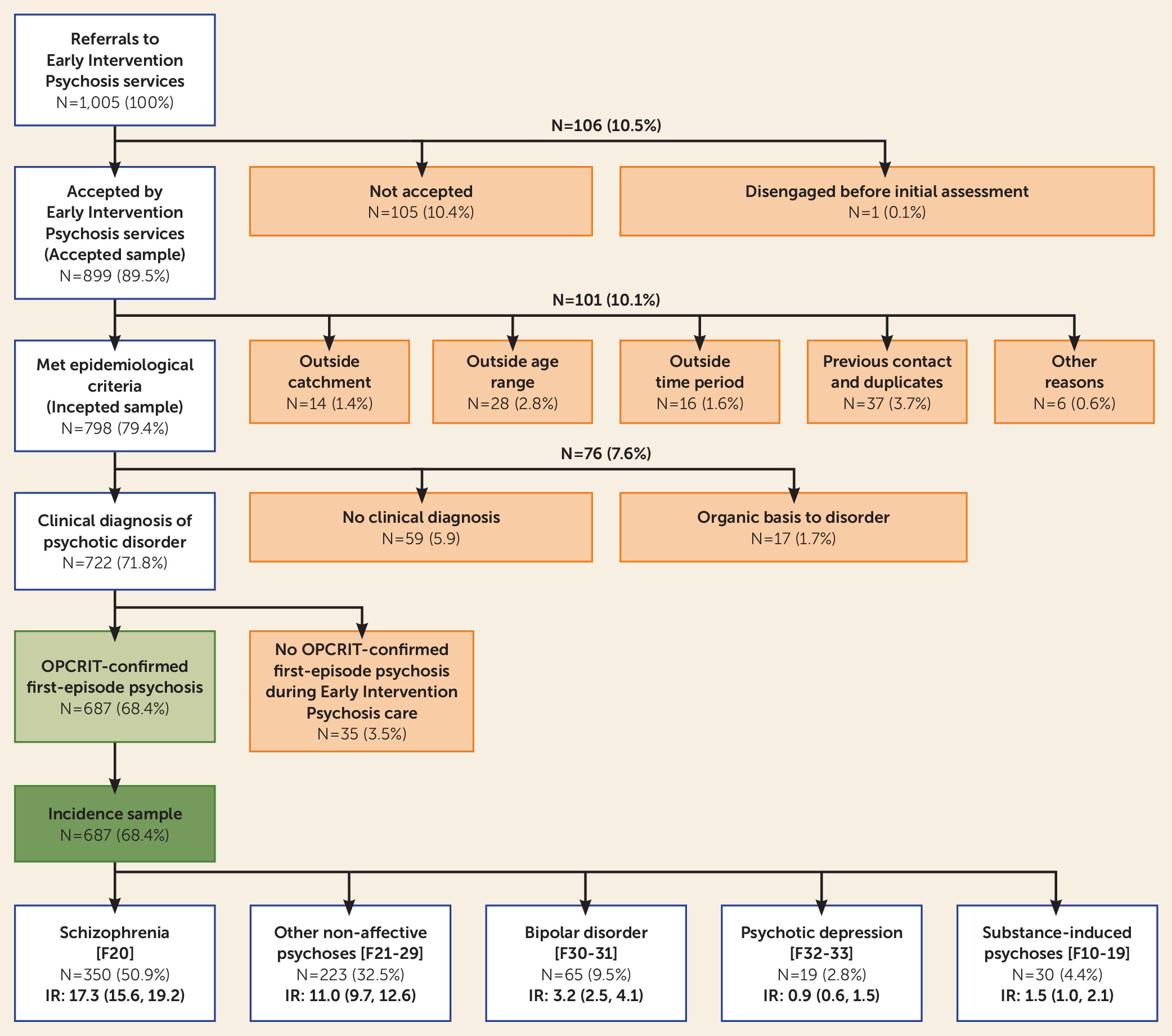
Over 1,000 people (N=1,005) were initially referred to six early intervention psychosis services with a suspected first episode of psychosis during 2.02 million person-years at risk, of whom 899 (89.5%) were accepted into care (
Figure 2). This corresponded to crude referral and acceptance rates of 49.7 (95% confidence interval [CI]=46.7–52.9) and 44.5 (95% CI=41.7–47.5) per 100,000 person-years, respectively (see Figure S1 in the
online data supplement). A total of 101 participants (10.0%) did not meet epidemiological criteria (
Figure 2), leaving 798 people in our incepted sample, of whom 687 (86.1%) were diagnosed with an OPCRIT-confirmed ICD-10 psychotic disorder (F10–F33). This corresponded to a crude incidence of 34.0 new cases per 100,000 person-years (95% CI=31.5–36.6). Most incidence cases received a diagnosis of schizophrenia (F20; 50.9%) or other nonaffective psychotic disorder (F21–F29; 32.5%), giving a crude incidence of 28.3 per 100,000 person-years (95% CI=26.1–30.8) for nonaffective psychotic disorders. The incidence of affective psychotic disorders (F30–F33) was lower (4.2 per 100,000 person-years; 95% CI=3.4–5.1); the majority of these cases (77.4%) were bipolar affective psychoses (
Figure 2). The incidence of probable substance-induced psychosis was low (1.5 per 100,000 person-years at risk; 95% CI=1.0–2.1).
Baseline Characteristics and Descriptive Epidemiology
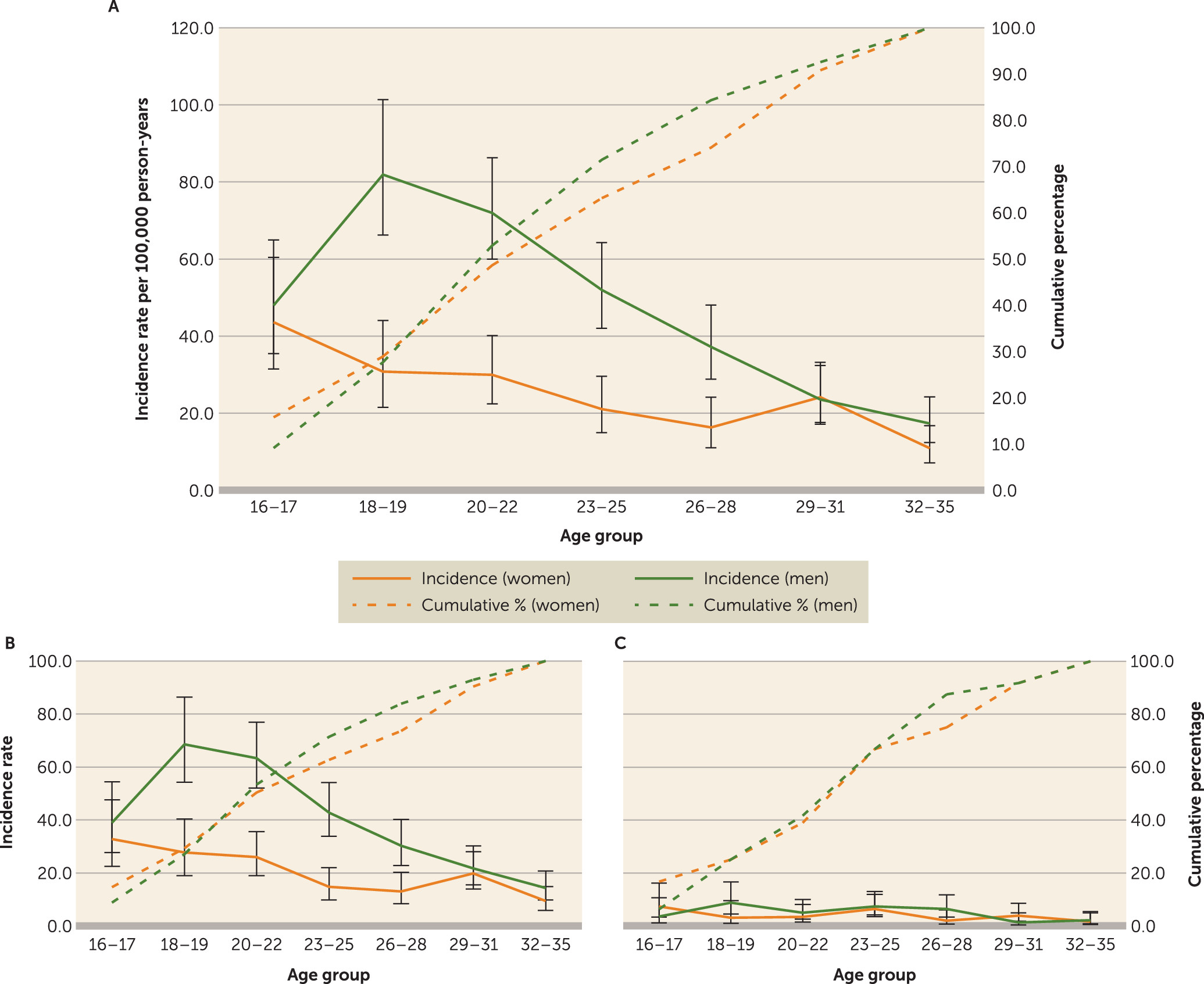
In our incidence sample, median age at referral did not differ between men (22.5 years; interquartile range: 19.5–26.7) and women (23.4 years; interquartile range: 19.5–29.1; Mann-Whitney U test: Z=1.0, p=0.27). We observed weak evidence (Kruskal-Wallis χ
2=5.0 on 2 degrees of freedom [df ], p=0.09) of differences in median age at referral between affective (23.6 years; interquartile range: 20.0–27.3), nonaffective (22.6 years; interquartile range: 19.6–27.4), and probable substance-induced (21.0 years; interquartile range: 17.7–24.7) psychoses. Two-thirds of cases (N=459 [66.8%]) were men (
Table 1), although there was weak evidence that this pattern differed between nonaffective (67.7% men), affective (57.1% men), and probable substance-induced (76.7% men) (χ
2 on 2 df=5.1, p=0.08) psychoses. Compared with the population at risk, cases were more likely to be men, to be younger, to be from an ethnic minority background, to be single, to be unemployed, to be of lower socioeconomic status, and to be from more deprived and densely populated neighborhoods (all p values <0.01), reflecting corresponding variation in crude incidence (
Table 1). Further examination of incidence by age revealed classic effect modification by sex (
Figure 3A; likelihood ratio test-χ
2 on 6 df=21.1, p<0.01), such that rates were higher for men than women until 29–31 years of age, with a decline in incidence for both sexes from initial peak rates at ages 18–19 in men and ages 16–17 in women. These patterns were similar for nonaffective psychoses (
Figure 3B; likelihood ratio test-χ
2 on 6 df=15.4, p=0.02) but differed for affective psychoses (likelihood ratio test-χ
2 on 6 df=9.5, p=0.15), which were similar for men and women at all ages (
Figure 3C).
Variation in the Incidence of All Clinically Relevant Psychotic Disorders
Incidence varied by age, sex, ethnicity, socioeconomic status, and setting, following mutual adjustment for each other (
Table 2, adjustment 1). For example, rates were 1.47 times higher in ethnic minority participants (95% CI=1.23–1.76) compared with the white British group, increased with lower socioeconomic status, and varied between early intervention psychosis services. Further multilevel modeling suggested that variation in incidence across the region was associated with both neighborhood-level population density and multiple deprivation, after adjustment for all other covariates (
Table 2, model 2). We observed evidence that this relationship was nonlinear, with excess rates restricted to the most densely populated (incidence rate ratio: 1.37; 95% CI=1.02–1.84) and deprived (incidence rate ratio: 2.11; 95% CI=1.34–3.32) neighborhoods in the study.
Variation in the Incidence of Nonaffective and Affective Psychotic Disorders
Incidence of nonaffective psychoses followed similar patterns as those described above with respect to individual-level risk factors (see Table S2 in the data supplement). However, only multiple deprivation (incidence rate ratio in most compared with least deprived neighborhoods: 2.74; 95% CI=1.71–4.39) remained consistently associated with neighborhood-level incidence (see Table S3 in the data supplement). There was some evidence that patterns of risk differed for affective psychoses, despite a smaller sample (N=84). Rates were more similar for men and women (incidence rate ratio for men: 1.27; 95% CI=0.82–1.96) and less strongly associated with socioeconomic status, after adjustment for other confounders (see Table S2 in the data supplement). While affective psychoses rates varied between services, this was not associated with either neighborhood-level variable (see Table S3 in the data supplement).
Discussion
In this, the largest epidemiological study—to our knowledge—of first-episode psychosis conducted since early intervention psychosis services were introduced in England, we have precisely delineated heterogeneity in incidence in a mixed rural and urban population. Our findings should provide timely evidence for mental health care policymakers in various settings about the current burden of psychotic disorders in young people. In particular, our findings 1) reveal substantial incidence rates of all clinically relevant psychotic disorders in young people, 2) demonstrate that median age at first referral is similar for young men and women before age 35, with 50% of cases presenting by 23 years old, and 3) extend previous knowledge to show that incidence in more rural populations in England, which have received less research, varies by classic individual- and neighborhood-level social and economic determinants of health, particularly for nonaffective disorders; affective psychoses showed less variation overall.
Methodological Considerations
Our study was based on referrals to early intervention psychosis services from multiple sources, including other mental health services within the NHS, and self-referrals. Our findings should therefore be interpreted based on administrative or first-contact incidence. We were unable to perform a leakage study to detect potentially missed cases, which could have led us to underestimate the true incidence in the catchment area. Nonetheless, early intervention psychosis services are the sole referral point for young people with suspected psychotic symptoms and actively engaged in outreach and promotion in the East of England. In England, there is very little private mental health care for psychosis, reducing risk of leakage. The epidemiological characteristics of our sample were consistent with those of other major first-episode psychosis studies (
39,
40), implying that our study design did not introduce substantial underascertainment overall, or differentially by sociodemographic subgroups. Although the excess incidence in black and minority ethnic groups was smaller than normally reported (
13), we do not believe this is due to any under-ascertainment bias. While ethnic minority groups are known to have differing pathways to care (
41–
43), there is no evidence that they are less likely to be referred to early intervention psychosis services. Furthermore, a forthcoming paper from our study (available upon request from Kirkbride et al.) demonstrates that rates for specific ethnic groups are in line with excesses more typically observed (
13). Our modest incidence rate ratios for black and ethnic minority groups, overall, are probably driven by the large proportion of non-British white migrants in this population (52.2%), whose overall psychosis risk is similar to that of the white British population (
40). We did not measure the duration of untreated psychosis in our sample, but this could only have affected the estimation of incidence rates if it had changed rapidly over the short follow-up period of our study (3.5 years); this is unlikely, particularly given that services were well established in our catchment area.
We cannot generalize our findings to people younger than 16 years old. This remains an important, underexplored epidemiological research issue, given that early intervention services and more general youth mental health services often accept cases at 14 years old or younger; limited evidence suggests incidence before 16 years old is very low (
44,
45). Our catchment area was considerably more rural than those previously studied in England. Generalizability to other settings will depend on the exact composition of their catchment areas, and we did not have data on very rural areas (i.e., less than 48 inhabitants per square mile). Nonetheless, variation in population density across our catchment area included the values for median population densities of 37 of 50 U.S. states (
46).
We obtained denominator data from the 2011 census. While the true population at risk is dynamic, any demographic changes in East Anglia over the 3.5-year period of our study would have been small and unlikely to have substantially biased our results given the absolute rarity of psychotic disorders. The 2011 census methodology minimized and adjusted estimates for nonresponse prior to publication (
47). We could not adjust or inspect variation by factors including family history of psychiatric disorders or substance use, which are not routinely collected for the denominator.
We used a two-stage diagnostic procedure to apply research-based criteria for psychotic disorder to our initial sample. OPCRIT diagnoses were assessed by trained clinicians, with good interrater reliability based on a small sample of 20 real-world case vignettes. The proportion of people who received a clinical diagnosis in the incepted sample, who also met OPCRIT criteria for psychotic disorder, was high (positive predictive value=687/722 [i.e., 95.2%]), demonstrating good concurrent validity in line with previous research (
36). We presented results for all clinically relevant disorders given current interest in this broad psychosis phenotype. Rates of affective psychotic disorders were lower than typically reported in adults (i.e., up to 64 years old) in England (
13), though consistent with observations elsewhere in Europe (
48). Given that the incidence rates of such disorders show less decline with age, and may even peak after 45 years old (
13,
49), lower rates reported in our young sample may be consistent with the underlying epidemiology.
Meaning of Findings: Implications for Mental Health Services Provision
Our findings highlight substantial demand for early intervention psychosis services in a large, diverse, mixed rural and urban population in the East of England. Referral rates to such services approached 50 people per 100,000 person-years, with services subsequently accepting nearly nine out of 10 referrals onto caseloads. We estimated that the true incidence of psychotic disorder seen through these services was closer to 34 new cases per 100,000 person-years. This difference highlights important challenges faced by policymakers, commissioners, and practitioners in developing, deploying, and delivering effective early intervention services.
Previous influential commissioning guidelines have used uniform estimates of narrowly defined schizophrenia incidence—closer to 15 per 100,000 person-years—based on an older epidemiology, as a basis for caseload and workforce calculations (
32). However, in practice, early intervention psychosis services may be mandated to intervene on a broader spectrum of psychoses, including other nonaffective and affective psychotic disorders, as well as other mental health disorders in which psychotic-like symptoms can present. In a U.S. context, where early intervention psychosis services are currently gaining momentum (
29,
30), service provision is primarily predicated on the treatment of nonaffective psychoses. If, however, earlier intervention in the critical period for psychosis generates greater diagnostic uncertainty (
50), this will inevitably result in a higher proportion of undifferentiated psychopathologies at first referral. Our data highlight some of the pragmatic realities in implementing early intervention psychosis services, which will accept a proportion of people who do not meet full research-based criteria for nonaffective psychotic disorder (29.1% of the incepted sample), in addition to 10.5% of people referred to but not accepted by services. Such groups would still require a degree of psychiatric triage and signposting, for which services need to be additionally resourced to effectively implement the fidelity criteria upon which they are predicated (
5). We have provided robust estimates of referral, acceptance, inception, and incidence rates in a diverse population, which can be used as part of a wider suite of evidence to inform service provision across the full spectrum of psychoses (
51), not limited to schizophrenia.
Meaning of Findings: Epidemiological Implications
Our findings extend previous epidemiological research to show that incidence of psychotic disorders varies by sociodemographic and environmental characteristics in more rural settings than typically studied (
11,
13). As expected, incidence rates were lower, overall, than reported in more urban populations in England. For example, recent rates for young people presenting to early intervention psychosis services in highly urban Southeast London (29,267 people per square mile) were 54.6 per 100,000 person-years (95% CI=49.5–60.2) (
52) higher than reported here. Nonetheless, crude rates of psychotic disorders in our most urban and deprived communities overlapped with such estimates, which persisted after adjustment for age, sex, ethnicity, and individual-level socioeconomic status. The nonlinear associations we observed between population density, deprivation, and psychosis incidence in our mixed rural and urban population imply that a threshold of exposure to environmental factors may be necessary to increase risk. These findings accord with limited previous research on this issue (
53). However, it remains unclear whether associations between environmental characteristics and psychosis risk reflect genuine etiological variance, or arise from selection factors, including familial aggregation of shared genetic or environmental experiences, which perpetuate downward social drift (
22). These processes may not be mutually exclusive but lead to the intergenerational accumulation of deleterious risk factors, which subsequently affect a number of adverse health and social outcomes, including schizophrenia and other psychoses. Further longitudinal studies are required to disentangle the potential role of social causation from drift or selection. Although we could not establish causation directly, our results demonstrate that our most deprived and urban communities shoulder a disproportionate burden of psychosis morbidity at the population-level. This should be used to inform the provision of effective early intervention services for psychosis.
Acknowledgments
The authors thank the Cambridgeshire & Peterborough (CPFT) and Norfolk & Suffolk Foundation Trusts (NSFT) for sponsoring this research. The authors also thank all service users and staff at the six EIP services where the SEPEA study took place: CAMEO North (Peterborough, CPFT), CAMEO South (Cambridge, CPFT), the West Norfolk Early Intervention Service (Kings Lynn, NSFT), the Central Norfolk Early Intervention Team (Norwich, NSFT), the Great Yarmouth & Waveney Early Intervention Service (Great Yarmouth, NSFT), and the former Suffolk Early Intervention Psychosis Service (Stowmarket, NSFT). The authors are grateful to staff at the NIHR Clinical Research Network: Eastern (formerly the Mental Health Research Network) for the invaluable support provided to the study, as well as for the dedicated help of all assistant psychologists and Clinical Studies Officers who contributed to data collection. In addition to assistance in OPCRIT assessment from several authors of this article, the authors are also grateful to Drs. Eva Aguilar (CPFT), Poornima Chandrappa (NSFT), Louise Colledge (CPFT), Ben Davies (CRN: Eastern), Jeanine Gambin (CPFT), Martina Gariga (CPFT), Maria Gonzalez (CPFT), Clare Knight (CPFT), Santvana Pandey (NSFT) and Swathi Theegala (CPFT), Rebecca Webster (CPFT), Lauren Wright (NSFT), Kayte Russell (NSFT), and Antonio Zambrana (CPFT) for their assistance with OPCRIT completion.