Double-Blind Randomized Clinical Trial of Prazosin for Alcohol Use Disorder
Abstract
Objective:
Method:
Results:
Conclusions:
Method
Participants
Procedures
Study design.
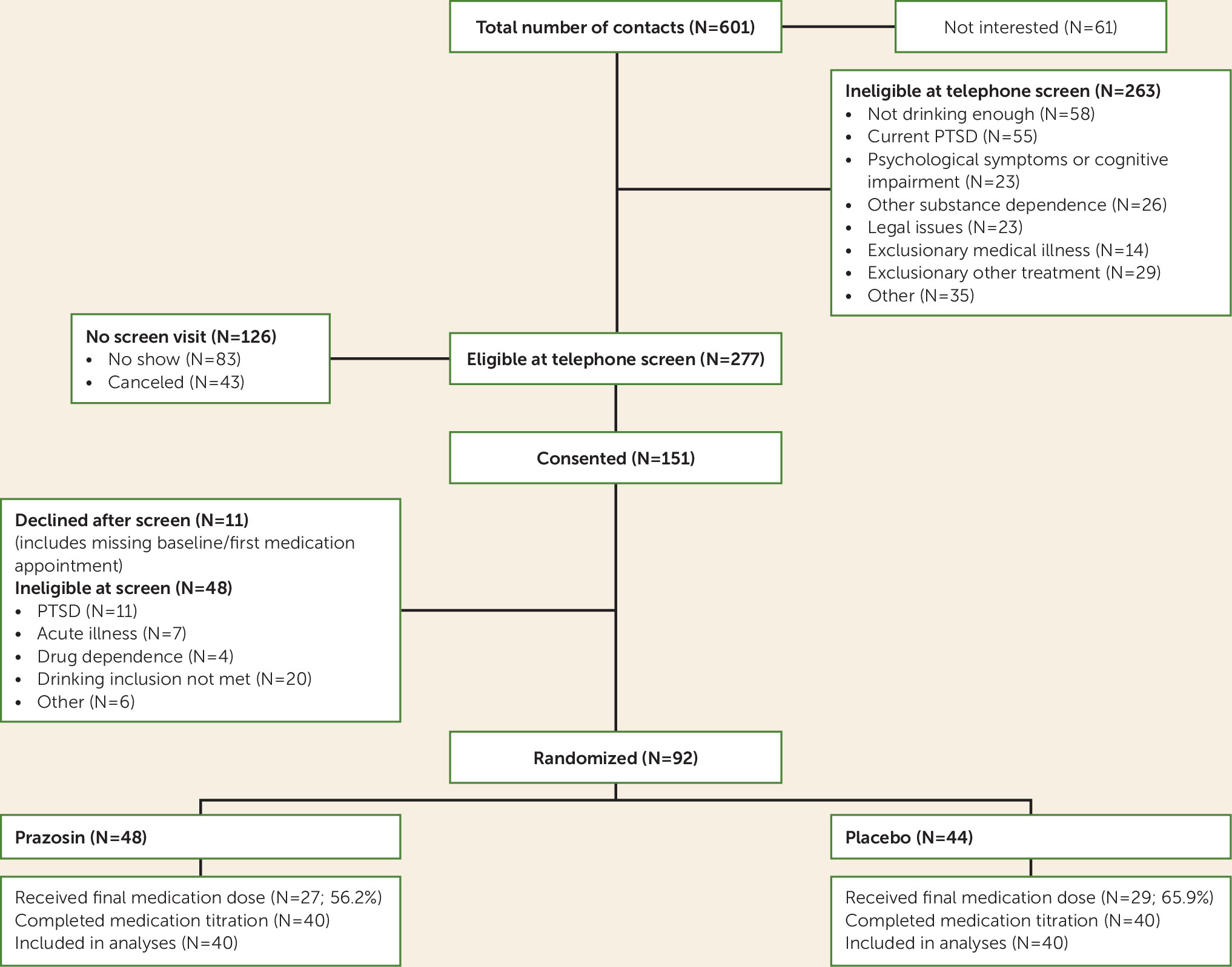
Recruitment and screening.
Randomization.
Study visits.
Measures
Mental health diagnoses and symptoms.
Substance use.
Interactive voice response daily monitoring.
Study Treatments
Medications.
Medical management.
Statistical Analysis
Daily interactive voice response data.
Sensitivity analyses.
Exploratory analyses.
Results
| Characteristic | Placebo Group (N=44) | Prazosin Group (N=48) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 49.1 | 9.5 | 47.3 | 9.8 |
| N | % | N | % | |
| Male | 36 | 81.8 | 37 | 77.1 |
| Ethnicity | ||||
| Non-Hispanic white | 23 | 53.5 | 29 | 59.6 |
| Black | 13 | 30.2 | 15 | 31.9 |
| Hispanic | 5 | 11.6 | 2 | 4.3 |
| Other | 3 | 4.7 | 2 | 4.3 |
| Veteran | 9 | 20.5 | 9 | 18.8 |
| Marital status | ||||
| Never married | 20 | 46.2 | 33 | 68.2 |
| Married | 8 | 19.2 | 4 | 9.1 |
| Separated or divorced | 14 | 30.8 | 9 | 18.2 |
| Widowed or other | 2 | 3.8 | 2 | 4.5 |
| Employed (part-time or full-time) | 39.5 | 44.4 | ||
| Mean | SD | Mean | SD | |
| Baseline drinking information for the preceding 90-day perioda | ||||
| Total standard drink units | 815 | 547 | 824 | 439 |
| Percent days drinking | 76.6 | 22.4 | 76.8 | 27.5 |
| Percent heavy drinking days | 66.5 | 26.0 | 71.8 | 29.1 |
| Average drinks per day | 9.1 | 6.1 | 9.2 | 4.9 |
| Average drinks per drinking day | 12.1 | 7.2 | 12.8 | 6.8 |
| Drinking across the last week of medication useb | ||||
| Percent days drinking | 35.5 | 39.7 | 43.0 | 44.0 |
| Percent days heavy drinking | 22.6 | 34.1 | 11.4 | 22.8 |
| Average drinks per day | 2.4 | 3.8 | 2.0 | 3.0 |
| Average drinks per drinking dayc | 6.3 | 5.7 | 4.6 | 4.0 |
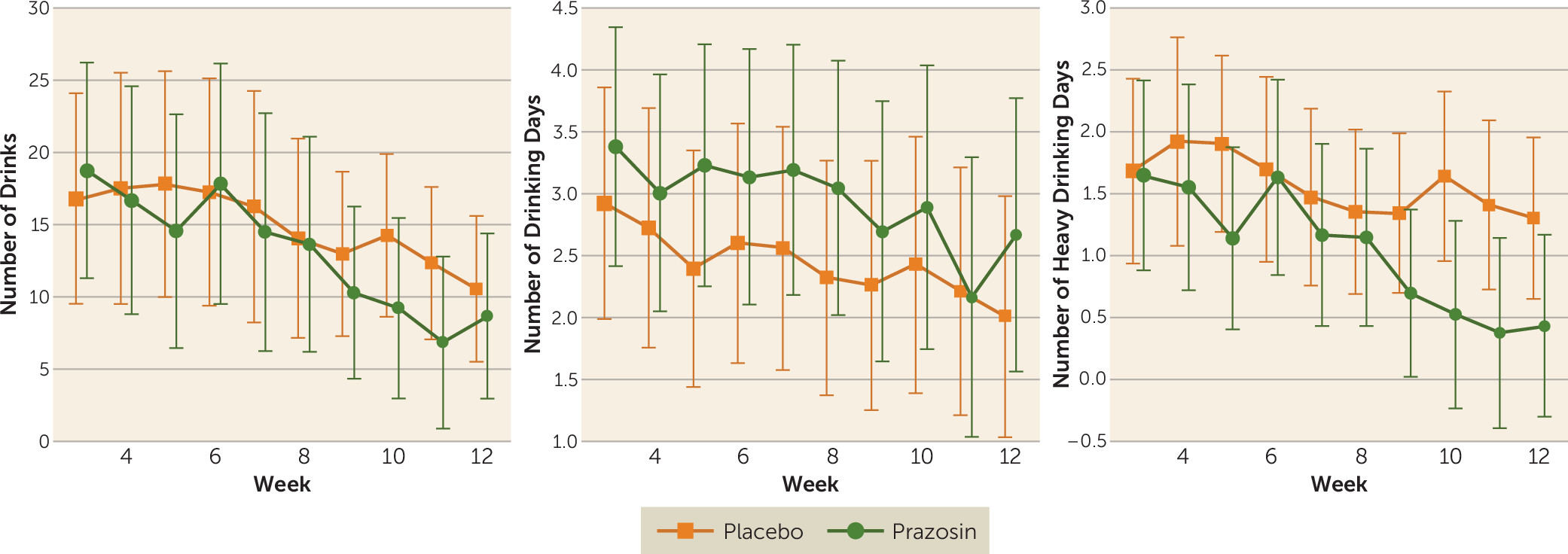
Primary Outcomes: Effect of Prazosin and Time on Daily Drinking Outcomes
| Prazosin Group (N=40) | Placebo Group (N=40) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week 3 | Week 12 | Changeb | Week 3 | Week 12 | Changeb | Difference in Changeb | ||||||
| Drinking Outcome | Mean | Mean | Mean | 95% CI | Mean | Mean | Mean | 95% CI | Mean | 95% CI | χ2 | p |
| Number of drinks per week | 21.3 | 13.3 | 8.0 | 1.8, 19.5 | 14.6 | 13.1 | 1.5 | –3.4, 6.8 | 6.5 | –2.4, 19.1 | 4.50 | 0.03 |
| Number of drinking days per week | 3.2 | 2.8 | 0.4 | 0.1, 0.8 | 2.8 | 2.3 | 0.5 | 0.1, 0.7 | 0.0 | –0.4, 0.5 | 0.006 | 0.94 |
| Number of heavy drinking days per week | 1.8 | 1.0 | 0.8 | 0.3, 1.0 | 1.5 | 1.2 | 0.3 | 0.0, 0.5 | 0.5 | 0.0, 0.8 | 6.55 | 0.01 |
Secondary Outcome, Sensitivity Analyses, and Exploratory Analyses
Adherence
| Prazosin Group (N=40) | Placebo Group (N=40) | |||
|---|---|---|---|---|
| Measure | Mean | SD | Mean | SD |
| Percent daily adherence to daily interactive voice response questions | 68.8 | 29.7 | 76.6 | 31.4 |
| Number of days in study | 71.6 | 20.6 | 73.6 | 21.7 |
| Percent days reported taking any study medicationa | 64.8 | 31.0 | 75.6 | 31.8 |
| Visits with positive riboflavin tracea | 64.1 | 26.0 | 71.3 | 28.6 |
Safety Findings
Adverse events.
Side effects.
| Prazosin Group (N=44) | Placebo Group (N=48) | ||||
|---|---|---|---|---|---|
| Event or Side Effect | Mean | SD | Mean | SD | p |
| Drowsiness | 28 | 58.3 | 15 | 34.1 | 0.020 |
| Edema | 9 | 18.8 | 2 | 4.6 | 0.036 |
| Dizziness | 20 | 41.7 | 14 | 31.8 | 0.328 |
| Light-headedness | 23 | 47.9 | 17 | 38.6 | 0.370 |
| Headache | 17 | 35.4 | 17 | 38.6 | 0.749 |
| Lacking energy | 23 | 47.9 | 16 | 36.4 | 0.263 |
| Weakness | 10 | 20.8 | 6 | 13.6 | 0.363 |
| Palpitations | 11 | 22.9 | 5 | 11.4 | 0.144 |
| Nausea | 18 | 37.5 | 11 | 25.0 | 0.197 |
| Change in urination | 9 | 18.8 | 5 | 11.4 | 0.324 |
Discussion
Patient Perspective
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 950.33 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).