What could reduced gray matter over most of the cerebral cortex have to do with strong physical and social fear? This is the question raised in a study by Kaczkurkin et al. in this issue of the
Journal (
1). The study uses the Philadelphia Neurodevelopmental Cohort, including over 1,600 participants in late childhood and early adolescence who have undergone structural brain scans and represent diverse mental health diagnoses, including attention deficit hyperactivity disorder, major depression, and anxiety disorders.
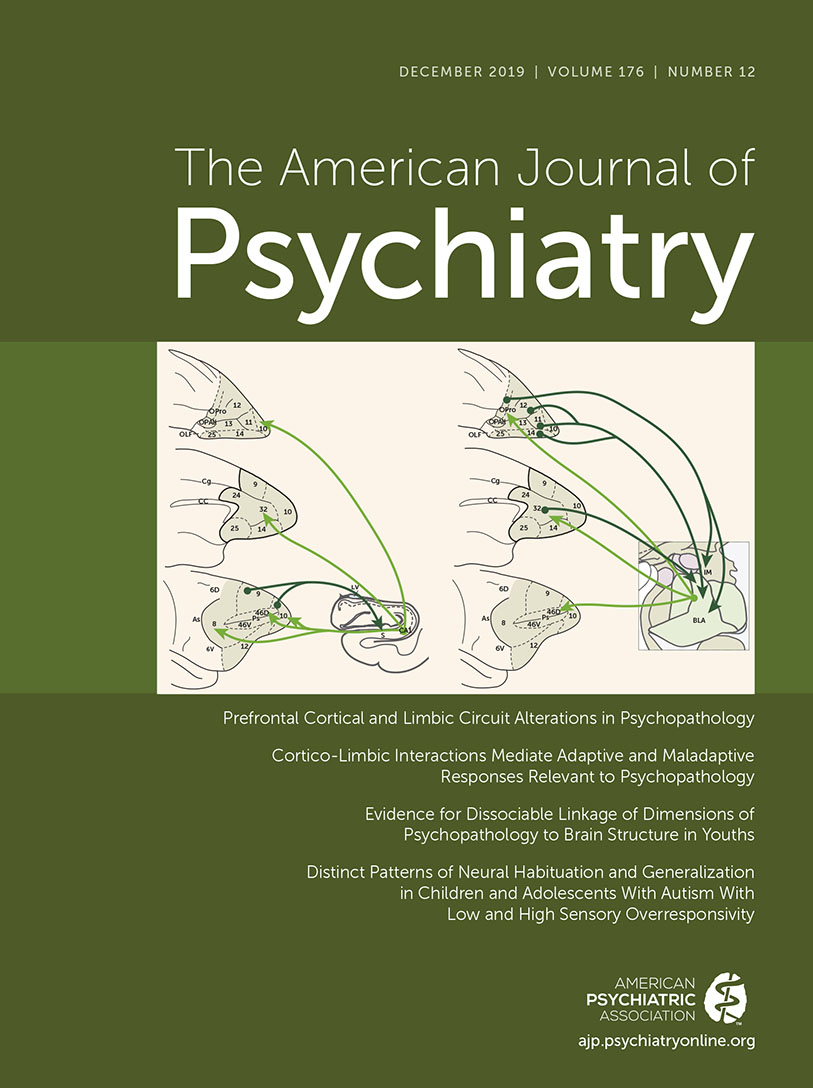
The methods are in line with current efforts to improve diagnosis of mental illness by finding the biological bases that cut across traditional mental health categories. Kaczkurkin et al. used bifactor modeling to reduce clinical symptoms to five orthogonal dimensions, which were labeled anxious-misery, psychosis, behavioral/externalizing, fear, and overall psychopathology. One of these dimensions, fear, is the main topic of the article. The authors used nonnegative matrix factorization to reduce their structural scans of the cortex to 18 networks and related fear to each of them. Thirteen of the 18 networks show significant negative correlations between cortical thickness and the fear dimension.
How could this be? A substantial amount of animal (
2) and human data show that brain structures related to fear include the amygdala and other subcortical brain areas.
Although the study focused on children and adolescents, cortical control of fear occurs from infancy to old age. Parents are very accurate in rating whether their infant or child is fearful in physical and social situations (
3). Fear is present over the lifespan, but its expression varies. Even in infancy, the expression of fear can be controlled from cortical areas. Four- and 6-month-old infants, when distressed from intense sound and light, show behavioral soothing when distracted by a novel object (
4). The brain network involved in orienting includes dorsal and ventral areas of the parietal and frontal lobes (
5). If orienting to the novel object ends, the infant returns to the same level of distress as before the distraction was introduced. While subcortical areas are critical for the emotion, its expression depends on the infant’s attention networks.
During childhood, a brain network including the anterior cingulate and insula develops, connecting to multiple brain areas (
5). This network exercises control over emotional expression and its subcortical sources. Imaging studies of adults find that negative words and pictures show activation of the amygdala, but when study participants are asked to avoid the emotion, activity is seen chiefly in midline frontal areas, including the ventral anterior cingulate cortex (ACC), and a reduction is seen in amygdala activity. Individuals with poor emotional control, such as patients with borderline personality disorder, show reduced activity in the ACC and higher than normal amygdala activity (
6). Presumably the number of neurons active within the ACC is reduced in individuals with poor emotional control. In the Kaczkurkin et al. study, thinner cortical areas were found for high levels of fear. This suggests that high levels of fear are associated with thinner cortex, and thus fewer neurons are present to become active in imaging studies.
In old age, emotional control is often diminished, which may be related to increased anxiety and fear. Past imaging research has shown that the ACC and adjacent midprefrontal cortex show a metabolic reduction that correlates with age-associated cognitive decline in healthy volunteers (
7).
There is also evidence that the specific pathways mediating control over fear and other emotions may change across development. In infancy, the network related to the ACC appears to be barely connected to brain areas leading to action (
8). In early childhood, the size of the ACC is most related to speed of response in resolving conflict (
9). However, as the cingulate becomes increasingly connected to brain areas generating behavior, it is the ACC’s connectivity that predicts reaction time in the conflict task. Most of such connections would have been made by the ages of the study subjects in the Kaczkurkin et al. study.
There is little reason to think that the stronger control by a network at one point in life eliminates control by other networks. The importance of orienting toward positive events and away from threatening ones is critical in infancy but persists at later ages (
3). Thus, one would expect to find that multiple brain areas involved in cortical control of fear have stronger overall correlations with individual differences in fear than other cortical areas. Table 1 in the
online supplement to the Kaczkurkin et al. article bears this out to some degree, but attention involved in the control of fear does not fully account for all brain areas found to correlate with the fear dimension. Although there may be more specificity in the control of fear by cortical networks, more targeted ages and more precise methods might help us learn what they are.
The Kaczkurkin et al. study suggests that control of fear may be a common deficit in many forms of pathology, at least in children and adolescents. Cortical control networks for emotion overlap substantially with the brain’s attention network. Randomized trials of meditation training have found that 2–4 weeks of training produces a change in connectivity surrounding the ACC as measured by diffusion tensor imaging compared with a relaxation training control group (
10). Based on the common finding that meditation produces a strong frontal theta rhythm (4–8 Hz) in scalp-recorded EEG, optogenetic studies have found that laser stimulation at low frequency near the theta rhythm in mice results in an increase in oligodendrocytes in white matter (
11). In these studies in both humans and mice, there is evidence of reduced fear and anxiety as a result of the training or stimulation.
So far, these stimulation methods have not been tried with pathological conditions of the type included in the Kaczkurkin et al. study. However, 2 weeks of meditation training in comparison with a relaxation training control group has been shown to normalize the reduced connectivity between the ACC and striatum found in smokers and to reduce smoking by over 60% (
12).
Despite the many as yet unsettled question raised by the Kaczkurkin et al. study, three important general issues are supported by the study findings and our extrapolation to attention networks.
The first is that many of the symptoms of pathology may be summarized along some of the same dimensions (e.g., fear) that are used to measure individual differences in temperament or personality in healthy individuals. The values observed in individuals with psychopathology may be more extreme, but they are not of a different kind.
The second is that the strength of cortical networks is related to individual differences in human behavior, including pathologies. Thus, not only are brain networks important determinants of behavior, a conclusion not likely to be disputed these days, but also differences in network strength, from whatever source, may help account for differences we find among people. Thus, emotion is an expression of underlying brain biology. This point supports the search for biological markers for mental disorders.
Third, we can learn about how to treat mental disorders by paying attention to their similarities, not only to their differences. Emphasizing differences between pathologies for differential diagnosis has led to neglect of commonalities that may turn out to be critical for both understanding the disorders and providing effective treatments for them.
The Kaczkurkin et al. study used a large online database and new methods for manipulating big data to examine critical issues in psychopathology. However, some of the studies cited in our comment show that small-scale studies of healthy people and animals remain a useful way for understanding the details of brain networks related to pathological symptoms.