Major hurdles confront attempts to create clinically useful imaging measures. In some ways, these hurdles are particularly high for studies in youths, given restrictions on research with vulnerable populations such as children and adolescents. However, research in youths is also particularly important, given the developmental nature of most mental disorders. In this issue of the
Journal, Green and colleagues (
1) report on new data from a functional MRI (fMRI) study in autism spectrum disorder (ASD), a prototypical neurodevelopmental disorder. Beyond generating important insights into ASD, the work is notable for the broad way that it informs clinical neuroscience research by highlighting pressing issues in the field. As such, taking stock of the work elucidates both short-term and longer-term goals for fMRI studies on pediatric mental illness, possibly illuminating a path toward increasing clinical relevance.
Sensory Hyperresponsivity
Green and colleagues examined 42 high-functioning youths with ASD and 27 age-matched, typically developing youths. They further divided patients with ASD according to their levels of problematic sensory overresponsivity, as rated on questionnaires completed by their parents. Clinicians seeing children with ASD frequently encounter this problem. For example, I vividly recall the happiness reported by parents of my patients when tagless T-shirts became ubiquitous—T-shirts in which the traditional sewn-in fabric label at the back of the neck has been replaced by printed labeling; this relieved the distress created by a “horribly annoying” tag-generated scratching on the back of my patients’ necks.
Sensory hypersensitivity was not codified in DSM until 2013, when changes in the fifth edition (DSM-5) reflected clinicians’ growing recognition of this problem’s impact. Unlike previous editions, DSM-5 includes the criterion of abnormal sensory responding in ASD as part of a broader domain pertaining to restrictive or repetitive behaviors. In this new study, Green and colleagues examined the pathophysiology of sensory hyperresponsivity; they exposed youths, during fMRI scanning, to auditory and tactile stimuli designed to provoke the types of sensory experiences rated by parents of youths with ASD as clinically problematic. As such, the study combines assessments in the clinical domain with fMRI assessments mapping correlates of real-time events corresponding to disturbing sensory experiences. Thus, the study applies an fMRI technique that weaves connections among symptoms, real-time experiences, and brain function.
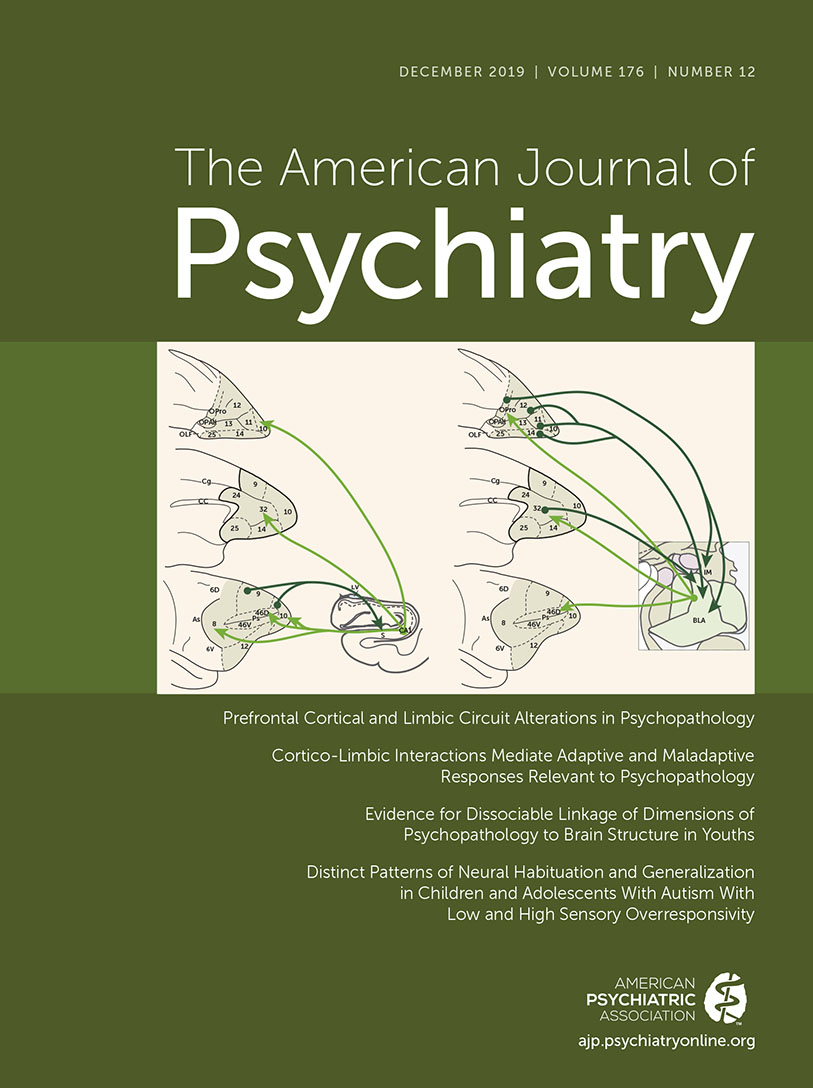
The study findings illustrate the complex nature of perturbed responding to stimuli that evoke sensory hyperresponsivity in patients with ASD. For example, problematic responding in these patients appears to involve disturbances in habituation, whereby responding in sensory cortices and fronto-amygdala brain regions fails to adjust with time to repeated stimulation in ways that manifest in the brains of other children. Moreover, this circuitry also displays attenuated reactivity to novelty in children who have both ASD and problematic overresponsivity, as compared with reactivity in other children. Finally, in children with both ASD and problematic overresponsivity, other brain regions manifest deficient filtering of background stimulation. These regions fail to express patterns suggesting inhibition, as occurs in the brains of other patients with ASD and of typically developing youths. The study thus maps the myriad ways in which brain function can differ among youths with both ASD and clinically problematic sensory overresponsivity, as compared with other youths.
Seeking Clinically Useful Tools
Clearly, scientific impact follows from Green and colleagues’ unique findings linking phenomena across clinical and neuroscience realms. However, the study is also notable for illustrating complex issues confronting clinically focused fMRI research on pediatric mental illnesses. These issues relate to practicality, statistics, the nature of mechanisms, and methods for demonstrating clinical utility. Delineating these issues brings into focus both short-term and long-term goals on a path that connects clinical and neuroscience-focused work.
From the perspective of practicality, Green and colleagues use a “passive-viewing” paradigm that relies only on fMRI data to characterize children’s responding. Moreover, the stimuli employed, while annoying, do not appear to produce behaviors in the MRI scanner resembling the clinical phenomena rated by parents on questionnaires. While this is a strength, as it increases tolerability and successful study completion, it is also a limitation, as this approach generates no direct evidence to confirm the existence of close relationships between the reactions to stimuli that children experience in the scanner and the reactions to stimuli that they find upsetting in their everyday lives. Other early-phase attempts to use novel stimuli in clinically relevant fMRI research with children have implemented similar approaches (
2). These approaches maximize practicality by deploying well-tolerated methods that place few demands on children.
To maximize clinical relevance, other studies have used alternative approaches. For example, some studies evoke more extreme aversive states in children, integrate additional behavioral or physiological data into the imaging paradigm, and then link these additional data to specific events experienced by children during scanning (
3). Such complex approaches precisely quantify phenomena in the MRI scanner rated on clinical measures. Differences between the Green et al. study and studies using these other methods reflect conflicts between practicality and clinical relevance. To remain feasible while maximizing clinical relevance, imaging studies of aversive states in children must “thread the needle.” Clinical relevance may be maximized by assessing on-line behaviors in pediatric patients experiencing distress that is clinically meaningful. However, these behaviors must be easy to assess, and the evoked distress must remain no more extreme than that children experience in their everyday lives. Thus, this new study illuminates questions about how to balance issues of feasibility and complexity to maximize clinical relevance.
The study also highlights important statistical issues. Green and colleagues preselected brain regions for analysis and conducted secondary whole-brain analyses using cluster correction. This region-of-interest approach is justifiable in early-phase research, particularly when prior studies inform such preselection, but the approach may contribute to failed replications. Accelerating the pace of discovery may require moving beyond region-based statistics. Some studies utilize a region-of-interest-based approach, to maximize power in research with relatively small sample sizes or fMRI paradigms with unclear test-retest reliability (
4). New methods would provide alternative means besides a region-of-interest-based approach to increase statistical power. For example, if refined techniques could address low reliability in fMRI, statistical power could be increased. These new methods then might be used in studies with many hundreds of subjects to support more conservative, whole-brain-corrected statistical approaches. Of note, this could lead fMRI research down a path followed in genetics, fortified by multisite investigations deploying identical imaging methods. Such work would accentuate the need to acceptably balance feasibility and complexity, an issue raised by Green et al. in the broader context of approaches in pediatric imaging. As such, this path holds unique obstacles for studies evoking aversive states and using complex procedures with children.
Studies like that of Green et al. inform a search for mechanisms connecting brain dysfunction to symptoms. Many scientists justifiably emphasize aspects of this search involving parallels between psychiatry and other branches of medicine. However, the brain’s complexity creates unique problems for psychiatry. These problems influence interpretations of mechanism-focused imaging findings and their extension through cross-species research. Considerable mechanistic research quantifies a series of observable components that can be directly measured. In cardiology this includes blood pressure or a patient’s ashen appearance. For Green et al., as in many psychiatric studies, it includes aspects of children’s behavior and their fMRI responses. However, studies on mechanisms in psychiatry also frequently draw inferences about components that are only indirectly observable. This often includes psychological processes, expressed as information-processing constructs rather than physical entities. These constructs cannot be directly observed but must be inferred by exposing a subject to a stimulus and measuring a change in behavior or brain function. For example, in the Green et al. study, such an information-processing mechanism must be invoked to explain how children with ASD experience distress when they encounter certain classes of stimuli.
Compared with studies of mechanisms in the physical sciences, less consensus exists on the best approach for mechanism-focused research on psychological processes, which are so important in psychiatry (
5). For example, some scientists suggest that the field should primarily focus on psychological processes like memory or attention. For these moderately complex constructs, considerable cross-species work exists that firmly links behaviors to brain functions through relatively well understood psychological processes. Other scientists, in contrast, suggest that this approach ignores some of the more important clinical constructs, such as patients’ experience of distress, including processes related to sensory hyperresponsivity. These highly complex constructs are difficult to study across species and therefore are understood in less depth than less complex psychological constructs. Failure to integrate these differing opinions in a consensus approach to mechanistic research slows progress. Reaching consensus on how best to advance mechanistic work in psychiatry provides an appropriate long-term goal for the field, since this problem affects many studies in clinical neuroscience.
Finally, Green and colleagues’ work generates important and achievable shorter-term goals for clinical imaging research on pediatric psychopathology. Perhaps the most tangible of these would involve extensions of the approach used in this study by applying imaging tools in prospective or therapeutic settings. From this perspective, imaging studies might provide a platform for prospective studies evaluating the ability of fMRI-based measures to predict outcomes, over and above clinical predictors of outcome. Similarly, therapeutic imaging research might use fMRI-based measures either to tailor currently available treatments to individual patients or to provide imaging-based targets for novel treatments. Success in meeting these short-term goals might follow when scientists reach consensus regarding approaches to address the other complex issues raised by the outstanding early-phase work reported by Green and colleagues.
In summary, Green and colleagues present important new findings on the biological correlates of sensory hyperresponsivity in ASD. The impact of these new results clearly arises through the eloquent way in which the study delineates relationships among specific clinical features, psychological processes engaged during imaging, and underlying neural circuitry function. However, an additional impact arises from extensions beyond the bounds of imaging research on ASD. This follows from the report’s ability to focus a lens on crucial issues in the clinical translation of brain imaging research with children and adolescents.