Exposure to potentially traumatic events during childhood is pervasive, with two-thirds of children experiencing violence (physical abuse, sexual abuse, or witnessing community or domestic violence) by age 16 (
1). Early-life exposure to violence can markedly alter neurobiological, psychological, and social development (
2). These changes increase the risk for developing both first-onset and comorbid internalizing psychopathology (
3), which has especially high overlap in symptom expression in adolescent girls (
4). However, the neurodevelopmental mechanisms conferring resilience and susceptibility to psychiatric disorders following abuse remain unclear. Recent models suggest that early-life adversity may alter maturation patterns in emotion-processing circuits, but it remains unknown how neurodevelopmental maturity may influence the relationship between threat-related (compared with deprivation-related) stress and risk for internalizing psychopathology. Identification of neural maturational markers of resilience and susceptibility could have important implications for clinical monitoring and treatment for youths who are victims of abuse.
Evolutionary trade-offs between an individual’s survival and development (e.g., investment in growth) and reproductive success (e.g., investment in sexual maturity) likely underlie individual differences in child development after early-life adversity. Life history theory and the differential susceptibility model suggest that these trade-offs are likely constrained by the susceptibility of various developmental milestones to early experiences. The stress acceleration hypothesis extends these frameworks by integrating early-life adversity and child neurodevelopment (
5). According to the hypothesis, early-life adversity may promote early development of emotion circuits, particularly those underlying threat-safety processing, to meet potentially dangerous environmental demands. Indeed, stress-related changes in the recruitment of emotion circuits often show patterns suggesting advanced development. For example, early development of amygdala-medial prefrontal cortex (mPFC) functional connectivity has been observed in youths exposed to maternal deprivation stress (
6) and those residing in disadvantaged socioeconomic neighborhoods (
7), and it has been found to be longitudinally associated with the severity of early-life adversity generally (
8). However, a more thorough review of the related literature indicates mixed results overall, equally suggesting both delayed maturation and no maturational differences (
9). Importantly, the stress acceleration model of adversity and the development of emotion-related circuits may be dependent on the characteristics of adversity experienced; this has been suggested by recent work incorporating the dimensional model of adversity and psychopathology (
10), where advanced biological aging measured via telomere shortening, epigenetic age, and pubertal development were specific to threat-related adversity (e.g., abuse) compared with deprivation-related adversity (e.g., neglect) (
11).
The relationship between emotion circuit maturation after abuse and resilience or susceptibility to subsequent psychopathology is also unclear. Current evidence suggests that fast developmental strategies during childhood increase risk for psychopathology in adulthood (
12). Additionally, abused youths are at increased risk for internalizing psychopathology earlier, with greater severity, and with more comorbidities (
13,
14). The latent vulnerability model (
15) suggests that resilience and susceptibility to psychopathology after early-life adversity depends on the degree of neurodevelopmental flexibility in systems underlying salience detection, threat appraisal, and emotion regulation in adapting to future adversity. Earlier-developing circuits underlying salience detection and threat appraisal (e.g., the amygdala, insula, and mPFC) are likely recalibrated toward increased recruitment to threat-related stimuli, spurring development toward a more mature threat processing phenotype. We suspected that vulnerability to psychopathology may then fundamentally depend on how later-developing circuits, especially in the lateral PFC, are recalibrated in response. In contrast to earlier-developing structures, the lateral PFC does not reach developmental plateau until early adulthood, remaining highly plastic throughout adolescence by maintaining increased levels of synaptogenesis and experience-dependent pruning, myelination, and apoptosis (
16). Therefore, such systems likely show greater variability in their developmental trajectories after early-life adversity, leading to greater variability in executive control processes underlying resilience or susceptibility to psychopathology. We posit that adaptive flexibility in the maturation of the lateral PFC is a key predictor for the development of internalizing psychopathology after early-life adversity, although this is likely highly dependent on the timing of the adversity.
In this study, we examined whether abused girls show advanced structural maturation in emotion-related circuits compared with whole-brain and language-related circuitry. Language-related circuitry was used as a control circuit to evaluate emotion circuit specificity. We examined whether the degree of structural maturity depended on the absence (resilience) or presence (susceptibility) of internalizing disorders and whether these effects were specific to abuse (threat) compared with neglect (deprivation). The focus on internalizing disorders broadly was a result of high rates of comorbidity between anxiety, depression, and posttraumatic stress disorder (PTSD), which if segregated would have considerably limited sample sizes and statistical power for psychopathology-related comparisons. Finally, we examined whether particular brain regions contributed to overall circuit maturation differently in abused girls who are resilient to internalizing disorders compared with those who are susceptible to internalizing disorders. By using machine learning in a stacked generalization framework, we implemented a normative development model trained to predict chronological age from regional gray matter volume estimates in typically developing girls. We then used the normative model to calculate a brain age gap estimation (BrainAGE; predicted age minus chronological age), an index of relative circuit maturation. BrainAGE has been shown to represent a biologically meaningful index that is reliable (
17,
18), heritable (
18), and associated with developmental neurophenotypes underlying illness (
19,
20). This index is specific to an individual’s brain at the time the data were collected and should not be interpreted as reflecting a developmental trajectory that the brain will follow into the future. We hypothesized that abused girls, both resilient and susceptible to internalizing disorders, would show greater emotion circuit BrainAGE (indicating advanced maturation) relative to typically developing girls. We also hypothesized that abuse-related gray matter volume in early-developing regions underlying salience detection and threat appraisal (e.g., the amygdala and insula) would contribute to more positive (advanced) BrainAGE. Finally, we hypothesized that late-developing regions underlying attentional processes and executive control (e.g., the lateral PFC) would best differentiate circuit maturation in resilient compared with susceptible abused girls.
DISCUSSION
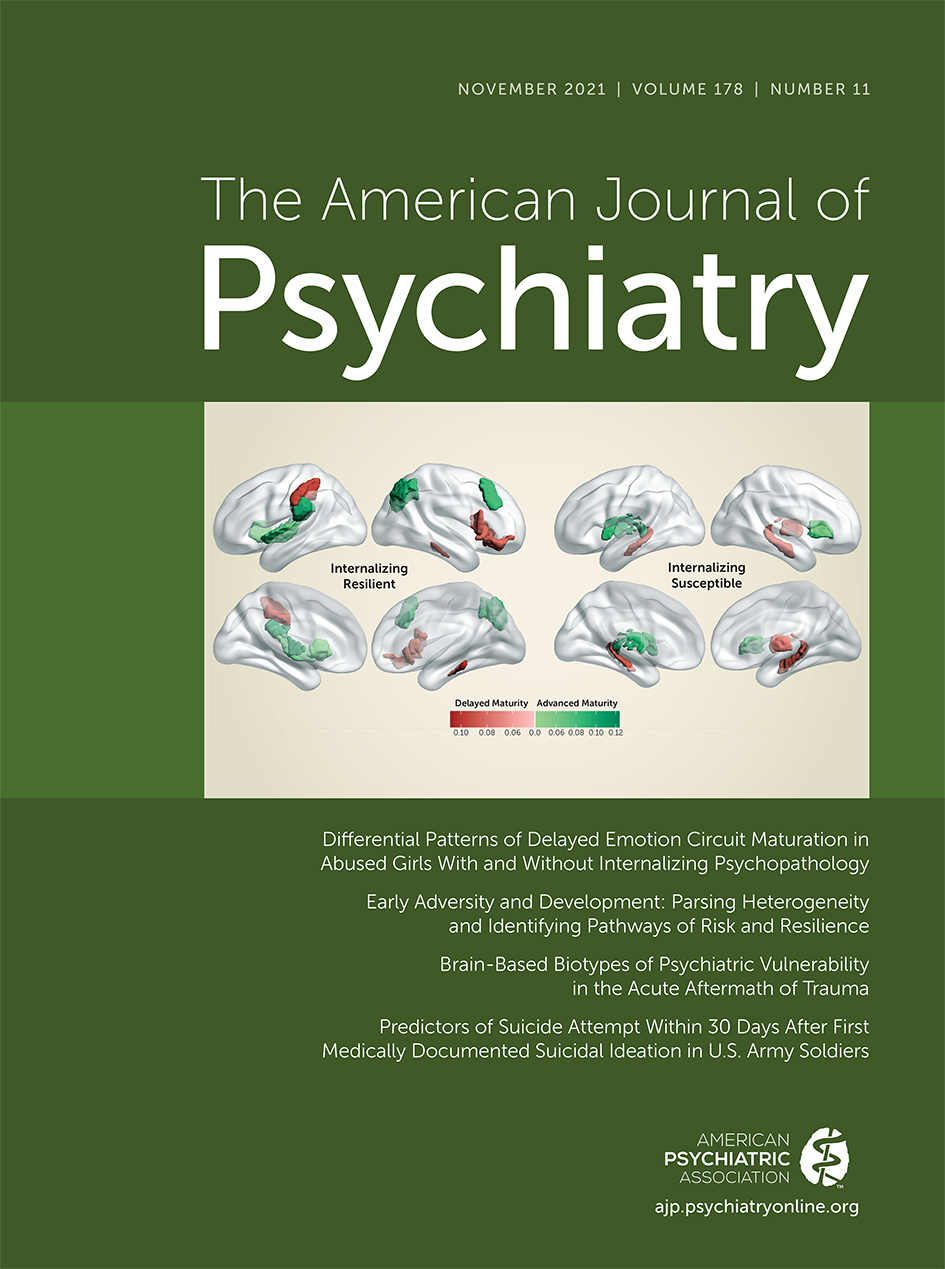
Abused girls, regardless of diagnostic status, showed delayed maturity in emotion circuitry (counter to our original hypothesis), which was further associated with increased hyperarousal symptoms. Advanced whole-brain BrainAGE was associated with increased physical neglect severity, suggesting differential effects of threat and deprivation stress on patterns of circuit-specific and whole-brain neurodevelopment. Additionally, we found unique regional contributors to emotion circuitry maturation in resilient and susceptible girls, most prominently in frontoparietal, hippocampal, and insular gray matter. Altogether, our findings provide new insights into brain maturational patterns related to threat- and deprivation-related adversity and internalizing psychopathology and point to potential systems-level mechanisms differentiating resilient and susceptible developmental trajectories.
Abuse exposure was associated with delayed emotion circuit maturity relative to typically developing girls, which was further related to increased hyperarousal symptoms (but only when controlling for group-level covariates and other PTSD-related symptoms). Although speculative, this suggests that delayed structural maturity in emotion circuits may underlie sensitive salience and threat detection systems in the brain, potentially leading to reduced threat-safety discrimination and states of generalized hypervigilance. Although enhanced threat bias in neurobiological reactivity is likely adaptive in abusive environments, this may lead to reliably misinterpreting safety cues as dangerous. Indeed, reduced threat-safety discrimination has previously been associated with younger developmental stage (children < adolescents < adults) (
26,
27), as well as with increased recruitment of threat processing circuits with maltreatment exposure and increased risk for psychopathology (
28,
29). For this reason, girls exposed to abuse may habitually recruit threat-related circuitry even in canonically safe contexts: this type of threat generalization, typically observed only in younger children, likely delays increases in synaptic pruning, circuit myelination, and other related processes that result in age-appropriate reductions in gray matter volume.
Physical neglect experiences, on the other hand, were positively associated with whole-brain maturity across typically developing and abused girls. Here, increased physical neglect corresponded to advanced whole-brain maturation. In contrast to the delayed emotion circuit maturation associated with abuse, this suggests that neglect and deprivation-related adversity may have global rather than circuit-specific effects on brain maturation. Indeed, the absence of expected age-typical cognitive and social inputs to the brain, as is often the case with physical neglect, likely affects the association cortex broadly, representing a global acceleration of neuronal and synapse elimination mechanisms typical of low-complexity environments (
10,
30). These mechanisms would translate to decreased gray matter volume in a deprivation context for equivalent chronological age, an advanced maturation phenotype. This may also explain the seeming discrepancy between previously reported findings of advanced emotion circuit development with adversity and the findings reported here, because the majority of these previous studies documented adversity more specific to deprivation (maternal separation [
6], disadvantaged socioeconomic neighborhoods [
7]) or a combination of threat and deprivation (abuse with physical or emotional neglect [
8)]). Thus, we suspect that the current formulation of the stress acceleration hypothesis, as it pertains to brain maturation, may more accurately account for broader whole-brain patterns specific to deprivation-related adversity. Additionally, because co-occurrence of deprivation- and threat-related adversity is common, global advanced maturation patterns specific to deprivation may mask threat-specific delayed maturation patterns only observed in emotion circuits when not examined separately, causing them to go unnoticed in earlier studies.
We observed unique gray matter volume phenotypes from abused girls contributing to significant shifts in BrainAGE distribution. Resilient, but not susceptible, abused girls showed dlPFC and lateral inferior parietal lobule gray matter volumes contributing to a positive (advanced) shift in emotion circuit maturation, supporting our original hypotheses. We previously reported that internalizing-susceptible youths show developmentally delayed gray matter volume reduction in the dlPFC (
31), and cortical expansion of the dlPFC differentiated which youths showed remission or persistence of PTSD symptoms at 1-year follow-up (
32). Although abnormal dlPFC structure has not been reliably associated with childhood abuse exposure (
9), changes in dlPFC structure and function have been broadly associated with reduced internalizing symptoms (
33,
34) and recovery from trauma (
35). For example, an inability to recruit the dlPFC during differentiation of threat from nonthreat mediates the relationship between anxiety disorders and generalized fear (
36). Additionally, repetitive transcranial magnetic stimulation of the dlPFC, altering functional connectivity with the amygdala (
37) and nucleus accumbens (
38), has been shown to reduce both anxiety and depression symptoms. Therefore, fronto-parietal structures contributing to advanced emotion circuit maturation in resilient girls may translate to a compensatory trajectory promoting more mature attentional and executive control processes, approaching adult patterns of function and decreasing psychiatric risk.
We also found that bilateral hippocampus gray matter volume contributed to negative (delayed) shifts in emotion circuit maturation in susceptible, but not resilient, abused girls. We previously reported age-related hippocampus gray matter abnormalities in traumatized youths with PTSD (
39), one of the most commonly reported neural correlates of early-life stress in youths and adults. Here, both childhood maltreatment and trauma exposure generally are associated with decreased hippocampal volume (
40–
42), likely driven by a combination of decreased neurogenesis/neural progenitor cells (
43), atrophy of dendrites and reduced postsynaptic dendritic spines (
44), and a reduced pool of stem cells into adulthood (
45). In alignment with our findings, decreased hippocampal volume appears to be more pronounced in maltreatment victims with PTSD and other internalizing disorders compared with those without (
42). Together, these results suggest that neurodevelopment underlying resilience to internalizing after abuse is critically dependent on regional patterns of maturation, where regions with a late (e.g., the dlPFC) compared with an early (e.g., the hippocampus) developmental plateau may have extended windows of change susceptibility in which to reorganize, a key factor in the development of pathology-inducing circuit phenotypes. The factors determining which children will undergo resilient circuit reorganization and which will not are unknown and warrant investigation.
The majority of differences in BrainAGE influential regions between resilient and susceptible girls were found in nodes of the cingulo-opercular network, including the insular cortex, opercular PFC, and lateral orbitofrontal cortex. Gray matter volume from susceptible and resilient girls contributed to more positive (advanced) and more negative (delayed) shifts in emotion circuit maturation, respectively. The cingulo-opercular network is a key substrate of threat-processing circuitry and is recruited by salient or unexpected stimuli to reorient attention circuitry toward relevant cues and inform subsequent responses (
46,
47). Abnormal development of the orbitofrontal cortex, cross-sectionally and longitudinally, has been reported in studies of abused youths (
31,
39). As the brain’s “engine of alertness,” abnormalities likely underlie symptoms of hyperarousal and hypervigilance commonly observed after abuse (
48,
49). In fact, meta-analyses across all DSM-IV axis I disorders suggest that gray matter volume in the insular cortex is the best differentiator of individuals with diagnosable psychopathology broadly and those without (
50,
51). We suspect that differences in the maturation of the cingulo-opercular network underlie important differences between resilient and susceptible girls after abuse, presumably through biasing attentional processes toward threat detection and the promotion of emotional reactivity.
Our study is not without limitations. First, as is the case for many pediatric neuroimaging studies, the sample size of typically developing and abused girls was modest. The small sample size for nonabused girls with internalizing diagnoses precluded us from an omnibus analysis interrogating maturation patterns specific to internalizing psychopathology. Second, given that many measures collected had substantial missing data (depression, anxiety symptoms, and pubertal milestones), and these were not missing-at-random data, associated null findings should be interpreted with caution. For example, in a full sample, we would expect that earlier pubertal milestones for the same chronological age would be associated with more positive BrainAGE and, accordingly, that abuse exposure would be associated with delayed pubertal milestones. This would represent an important step in evaluating the biological validity of BrainAGE and its ability to test hypotheses regarding maturation. Finally, our sample included only female youths. While relevant given the higher prevalence of internalizing disorders in girls, studies including boys could begin to disentangle which reported effects are sex specific. Future research would be strengthened by using both structural and functional MRI data for abused youths simultaneously, supporting the functional implications of structural maturity differences. Longitudinal studies are required to confirm maturational differences associated with abuse, as well as whether preadversity gray matter volume accounts for developmental delays and whether clinical interventions can bring emotion circuit maturity back into a healthy range.
Despite these limitations, our study has many strengths. First is our use of ensemble machine learning and feature influence analyses. To our knowledge, this is the first study to interrogate multivariate circuit-specific BrainAGEs, where constraining the neural feature set to specific domains of function allows a more precise indexing of maturation. This allows for the detection of altered circuit maturation, which may normally go undetected in whole-brain analyses. These methods also allowed us to explore how abuse-related gray matter volume phenotypes contributed to changes in BrainAGE, an important step in understanding the neurodevelopmental relationships learned by the normative model. Second, our study focused on disentangling the effects of threat-related adversity compared with deprivation-related adversity on circuit maturation, which are all too often aggregated into a single “adversity” cohort. Finally, this is one of only a handful of studies using BrainAGE to interrogate important questions in development, and more specifically, related to early-life adversity and psychopathology in youths. Normative neurodevelopment models and the BrainAGE maturity index have the potential to allow researchers to test treatment strategies targeting specific circuits and help clinicians monitor the neurodevelopmental trajectories of their patients, with the aim of helping guide them back into healthy ranges.