According to the National Sexually Transmitted Disease Surveillance System and the Sentinel Site Network of China (Chinese Centre for Disease Control and Prevention,
http://www.chinacdc.cn), there were 419,306 syphilis cases in 2011, an increase of 16.95% over the same period in 2010. Thirty percent of untreated syphilis patients develop neurosyphilis (NS).
1 Syphilitic infection of the central nervous system can occur early or late in the course of the disease.
2,3 NS mimics many other medical and neuropsychiatric disorders, including personality disorders, psychosis, and dementia.
4,5 Dementia is the most common presentation of NS in psychiatry.
4 Other presenting psychiatric symptoms have included personality disorders, cognitive impairment, dysphoria or elevated mood, hallucinations, mania, and delirium.
4–7 This variable, nonspecific presentation not only creates diagnostic problems but also leads to incorrect therapeutic decisions. Therefore, the diagnosis of NS with psychiatric manifestations is a challenging task. Thus far, only a few NS patient neuropsychiatric studies have been reported, primarily as single case studies.
1, 5, 8–12 Here, we retrospectively review the psychiatric manifestations, original diagnoses, laboratory findings, and brain MRI results among NS patients with psychiatric manifestations as the primary symptom in patients from the Zhongshan Hospital, Medical College of Xiamen from June 2005 to February 2012.
Discussion
We characterized 169 NS in-patients from the Zhongshan Hospital, Medical College of Xiamen University, who were admitted between June 2005 and February 2012. Fifty-two of the 169 NS patients presented with psychiatric manifestations as the primary symptom of NS, all of whom were patients with general paresis (88.1%, 52/59). Because 11 of these patients had a history of syphilis, there was no doubt that they had NS when they were hospitalized during the study period. The remaining 41 patients were treated for the first time in the hospital neurology department. None of the 41 patients had a history of psychiatric illness, but all patients showed psychiatric symptoms. None of the patients were suspected of having NS at the time of their initial diagnosis; they were diagnosed with NS during their follow-up treatments. This was an interesting fact, as it normally takes quite a while for an NS diagnosis. The main diseases originally diagnosed included dementia, delirium, epilepsy, hypertensive arteriosclerotic intracerebral ischemic stroke, Parkinsonism, Alzheimer’s disease, memory disorder, alcoholic encephalopathy, transient ischemic attack, viral encephalitis, subcortical arteriosclerotic encephalopathy, depression, and hyperlipidemia. Interestingly, in the cases studied, all of the patients’ demonstrated psychiatric manifestations, which led to their direct admission to the psychiatric unit rather than to a medical or neurology unit with a psychiatric consultation. Clinicians, including internists and neurologists, and especially psychiatrists, need to have an increased awareness of NS, which may present as a psychiatric illness. Without such an awareness on the part of clinicians, not only will a NS diagnosis be missed, but extensive and unnecessary laboratory investigations will follow.
8 Prompt, effective NS treatment is essential because most of its manifestations are potentially reversible.
9 In a previous paper, we reported that NS misdiagnosis is a common phenomenon. In that study, we analyzed 21 patients with ischemic stroke as the primary symptom among the same patients; except for four patients with NS who had histories of ischemic stroke, 17 of the 21 NS patients with ischemic stroke as their primary symptom were first-treatment cases in the hospital emergency department, and none of the cases were suspected of NS during the initial diagnosis. The proportion of misdiagnosis was as high as 80.95% (17/21).
17Psychiatric and neurological symptoms may present as a consequence of extensively damaged parenchyma in cortical regions of the brain; known as general paresis, this encephalitic form of NS typically presents as a progressive dementia 10 to 20 years after the original infection.
24 Here, of the 169 NS patients, 52 (30.77%) had psychiatric manifestations as primary symptom of NS, and all occurred in patients with general paresis. Generally, acute cerebral involvement (syphilitic meningitis or meningovasculitis) with symptoms such as headache, cranial nerve palsies, and/or stroke can occur in the early stages of syphilis, whereas late-stage NS typically presents with neuropsychiatric symptoms such as general paresis.
2 Marked neuropsychiatric deficits such as progressive dementia with signs of cerebral atrophy are classic characteristics of parenchymal involvement in late-stage NS patients, particularly in patients with general paresis.
Fifty-two NS patients had psychiatric manifestations as the primary symptom. The natural history of NS is mild, nonspecific amnesia and personality disorders, and delirium, progressing to dementia. Although it may present as virtually any psychiatric disorder, a significant number of patients with NS present with an insidious dementing process that leads to a progressive global deterioration in intellectual functioning. It is recognized that NS infection often manifests with psychiatric symptoms such as mania, hallucinations, mood disorders, delirium, and aggression. The clinical features of general paresis may include cognitive impairment, delusional or apathetic states, seizures, dysarthria, myoclonus, intention tremors, hyperreflexia, and Argyll Robertson pupil.
24,25 Argyll Robertson pupil is a classic clinical sign of NS. Among our subjects, only two presented with this classic NS characteristic. Argyll Robertson prevalence seemed abnormally low in our research. It may be that our hospital clinicians were inexperienced in this area. If these clinicians had an insufficient understanding of Argyll Robertson prevalence and therefore ignored the importance of these symptoms in a NS diagnosis, they did not record this sign during the course of disease diagnosis.
In addition to clinical findings and brain imaging, the diagnosis of NS was supported by serological testing. Generally, to reliably assess the clinical stage of NS, a combination of several CSF abnormalities, including pleocytosis, elevated protein, VDRL (or RPR), and TPPA, must be evaluated.
26,27 The diagnosis of NS can only be confirmed by the comprehensive consideration of clinical findings, serological testing, and treatment results. However, particularly during the later stages of disease and after antibiotic treatment, serological and CSF abnormalities may become ambiguous and therefore difficult to interpret.
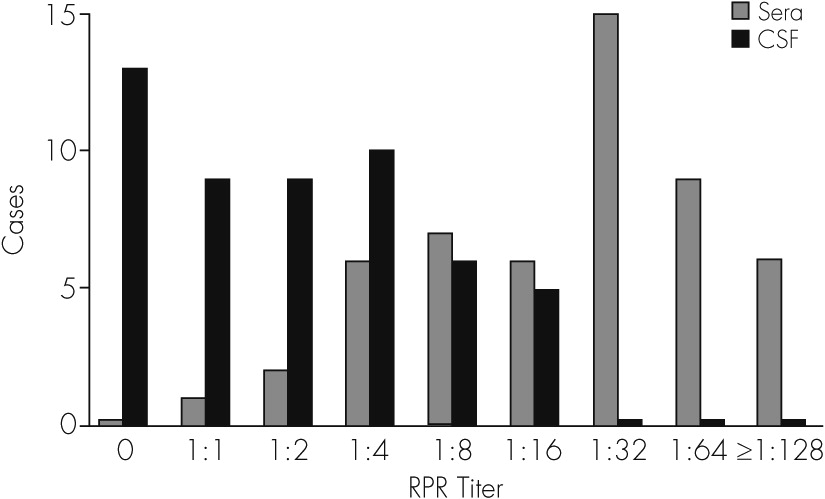
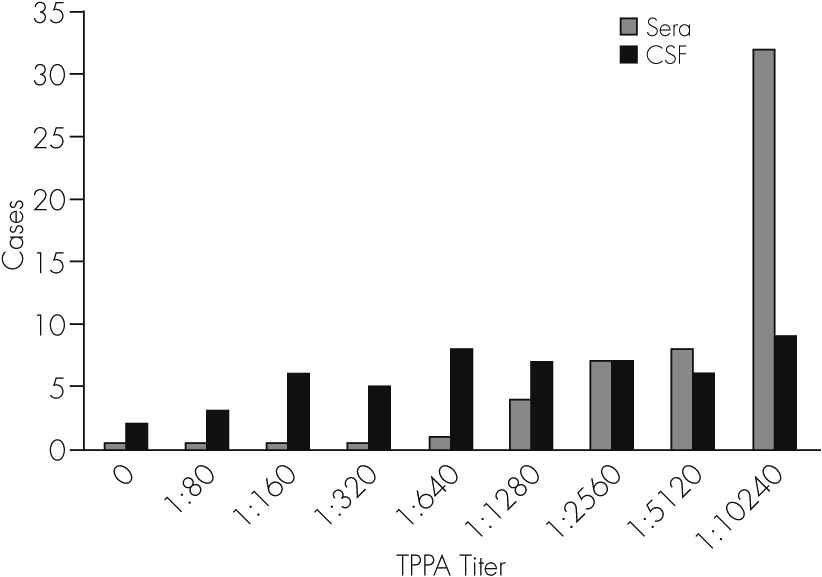
28 In our current study, among the 52 patients with general paresis and psychiatric manifestations, all tested positive during peripheral blood syphilitic serologic testing (RPR and TPPA). The positive rate of CSF-RPR was 75%, and that of CSF-TPPA was 96.2%. There were 23 (44.23%) patients with both CSF pleocytosis and elevated CSF protein.
Currently, the literature indicates that brain MRIs in most NS patients are normal or have nonspecific changes,
29,30 and there are no pathognomonic radiographic findings that suggest an NS diagnosis. Marano et al.
31 suggested that brain MRIs may not be helpful in the diagnosis of NS but are beneficial during follow-up treatments. In this study, 70% patients had an abnormal brain MRI. The MRI findings included cerebral atrophy, infarct ischemic stroke, demyelination, hydrocephalus, hippocampal sclerosis, and cerebral hemorrhage. Other reports suggest that brain MRI findings of cerebral atrophy
32,33 or vasculitis-related infarcts may support an NS diagnosis.
34 Recent studies using single photon emission computed tomography and positron emission tomography have shown brain dysfunction, with significant decreases in cerebral blood flow throughout the cerebrum in NS patients with psychiatric symptoms.
35Syphilis patients are often coinfected with HIV.
36,37 Among newly diagnosed syphilis patients coinfected with HIV, the incidence rate of NS is relatively high.
38,39 After comparing treatment responses between HIV-positive and HIV-negative syphilis patients, Ghanem et al.
40 found that the treatment failure rate in HIV-positive syphilis patients was higher, indicating that HIV negatively impacts syphilis treatment by inhibiting the host’s immune functions. During the last decades, some authors have reported changes in the clinical patterns of this disease,
41,42 which have generally been attributed to the expanded use of antibiotics as well as to the growing number of patients coinfected with HIV. However, the HIV positive rate in our local hospital was fairly low. Among the 297 NS patients, only two were coinfected with HIV. These limited data were not sufficient for subdivision; therefore, we excluded the HIV-positive patients from this research to reflect the population accurately.
The limitations of this retrospective chart review should be acknowledged. The major limitations of this study were its retrospective nature, and incomplete data for some of the patients. Two hundred ninety-seven patients were clinically diagnosed with NS in our hospital from June 2005 to February 2012; of these only 169 hospitalized patients were used in our study. Thus, selection bias is one concern because the exclusion of certain patients could affect the outcome. A well-designed study with long-term follow-up is necessary. There are diagnostic criteria for NS in clinical practice, and psychiatric diagnosis was performed according to the Diagnostic and Statistical Manual of Mental Disorders. At the time of hospitalization, NS was diagnosed according to the usual procedures; however, each patient’s symptoms and signs were not systematically or uniformly assessed. Some biases still exist, such as various descriptions from different clinicians. Finally, the association between MRI abnormalities and the various clinical findings should be interpreted with caution. NS diagnosis continues to be a challenge in a neuropsychiatric unit.
The importance of a rapid NS diagnosis is emphasized because early and effective treatment may not only prevent further disease progression but also allow for a complete recovery.
43 Therefore, NS should be considered as a differential diagnosis in patients who suffer from unclear mental abnormalities with acute or subacute onset, especially if focal neurological signs are missing. It is recommended that every patient with clinically evident neurological or psychiatric symptoms should receive a blood test for syphilis. When serology proves positive, all patients should undergo CSF examination. The existing law about the prevention and treatment of infectious diseases in China indicates that the HIV/syphilis/HBV/HCV tests are compulsively included in the detection process among blood donors and inpatients to prevent the spread of infectious diseases. This procedure can play an important role in finding patients infected with
T. pallidum. Psychiatrists are often the last line of defense against the progression of NS in infected patients.