The concept of recovery is increasingly prominent in mental health research and policy, and mental health services are encouraged to consider their role in supporting the recovery of individuals who experience mental illness (
1–
3). Recovery offers a transformational ideology for services and suggests reforms in how mental illness is understood and managed, as well as in how people living with mental illness are understood and helped (
4). This guiding philosophy challenges ideas and beliefs about the etiology and treatment of mental illness, including the way in which mental health practice is organized and implemented to ensure that people living with mental illness are allowed the opportunity to lead meaningful and productive lives (
5,
6). This vision values greater independence of people living with mental illness and adopts a shift from paternalistic mental health practices to practices that support autonomy (
7).
Although key building blocks for recovery-oriented practice have been proposed in international policy (
8–
10), research literature (
11,
12), and first-person narratives (
13,
14), it is a nebulous concept that is understood in a number of ways and is difficult to apply (
15). The term “recovery” is commonly used to refer to the process of how each individual comes to terms with and overcomes challenges associated with having a mental illness (
1,
5). On the other hand, mental health practitioners lean toward different meanings (
16) and often consider recovery in terms of symptomatology and view it primarily as improvement in mental health outcomes (
17). The subjective nature of recovery also means that individual practitioners emphasize different characteristics of recovery within their own practice, making routine operationalization (
18) and conceptualization of recovery a further challenge (
19,
20). The need for a consistent understanding and operationalization of recovery into mental health practice has been identified (
17,
18).
The aims of this study were to synthesize the characteristics of recovery-oriented practice guidance on the basis of international perspectives and to develop a useful overarching conceptual framework for translating recovery guidance into mental health practice. A conceptual framework provides an interpretive approach to the understanding of concepts and the relationships among them, which is developed through iterative qualitative analysis (
21).
Methods
Design
A literature search was conducted to identify recovery-oriented practice guidance. Each document was analyzed by using inductive thematic analysis, in which analytical concepts and perspectives are derived from the data in a deliberate and systematic way (
22). This approach allows exploration of the way that each document describes recovery-oriented practice, allows unexpected themes to emerge, and does not restrict the investigation to predetermined concepts or prejudge the significance of concepts.
Procedures
Guidance identification.
The literature search sought to identify guidance that explicitly describes or develops a conceptualization of recovery-oriented mental health practice. The term “guidance” is used to describe the range of documents included in the study, which was not limited to guidelines or practice standards. Guidance on recovery-oriented mental health practice was defined as recommendations developed as a guide to mental health services and mental health practitioners on supporting the recovery of people living with mental illness, guidance for users of mental health services to support self-advocacy of best practices and high-quality service delivery, an analysis of primary data, or a synthesis of secondary data. In addition, the guidance needed to be available in printed or downloadable form and written in English.
Three data sources were used to conduct the literature search. First, experts were asked to identify influential international policy and practice guidance. Second, an Internet search via Google Scholar using the key terms “recovery-oriented practice” AND “guidelines” OR “standards” OR “indicators” OR “competencies” was conducted. Third, manual search of reference lists of retrieved documents was undertaken. An electronic database search (for example, Medline) was not undertaken as policy and practice documents were sought rather than peer-reviewed articles in academic journals. The search was conducted in January 2010.
Analysis.
The characteristics of the eligible documents were identified in order to describe and define the guidance. The level of service user involvement in guidance development was rated by using three categories: control, collaboration, and consultation (
23). Control involves research in which service users take a lead, collaboration is defined as a shared partnership between service users and researchers in the research process, and consultation occurs when researchers consult service users about the research.
Inductive thematic analysis (
24) was used to systematically identify and synthesize the range and diversity of the key concepts of recovery-oriented practice identified in existing guidance. To meet aim 1, data extracts from each document were selected by two raters on the basis of the following criteria: described characteristics of recovery-oriented practice, provided definitions of recovery-oriented practice, or offered standards or indicators of recovery-oriented practice from which a succinct summary could be extracted. Initial semantic-level analysis was then undertaken by four analysts. Equal attention was paid to each data extract to identify initial codes, and individual extracts were coded under one or several themes to fully capture their meaning. An initial coding frame was developed; all extracts were double-coded by at least two raters, and a third rater resolved any differences.
To meet aim 2, interpretive analysis was undertaken to organize the themes into practice domains. Thematic maps were used to organize the themes by clustering all codes according to connections in the data and by considering the patterns and relationships between themes. Additional codes, refinements to the specifics of themes, and thematic patterns continued until theoretical saturation was achieved (
24).
Ethical approval
The study was conducted as part of a larger program of research, which has ethical approval obtained from the joint South London and Maudsley and the Institute of Psychiatry National Health Service research ethics committee.
Results
Guidance identification
Thirty documents were identified. [A list of the documents is available in an online supplement to this article at
ps.psychiatryonline.org.] Documents came from six countries—United States, England, Scotland, Republic of Ireland, Denmark, and New Zealand—and ranged in length from three to 149 pages. Their characteristics are shown in
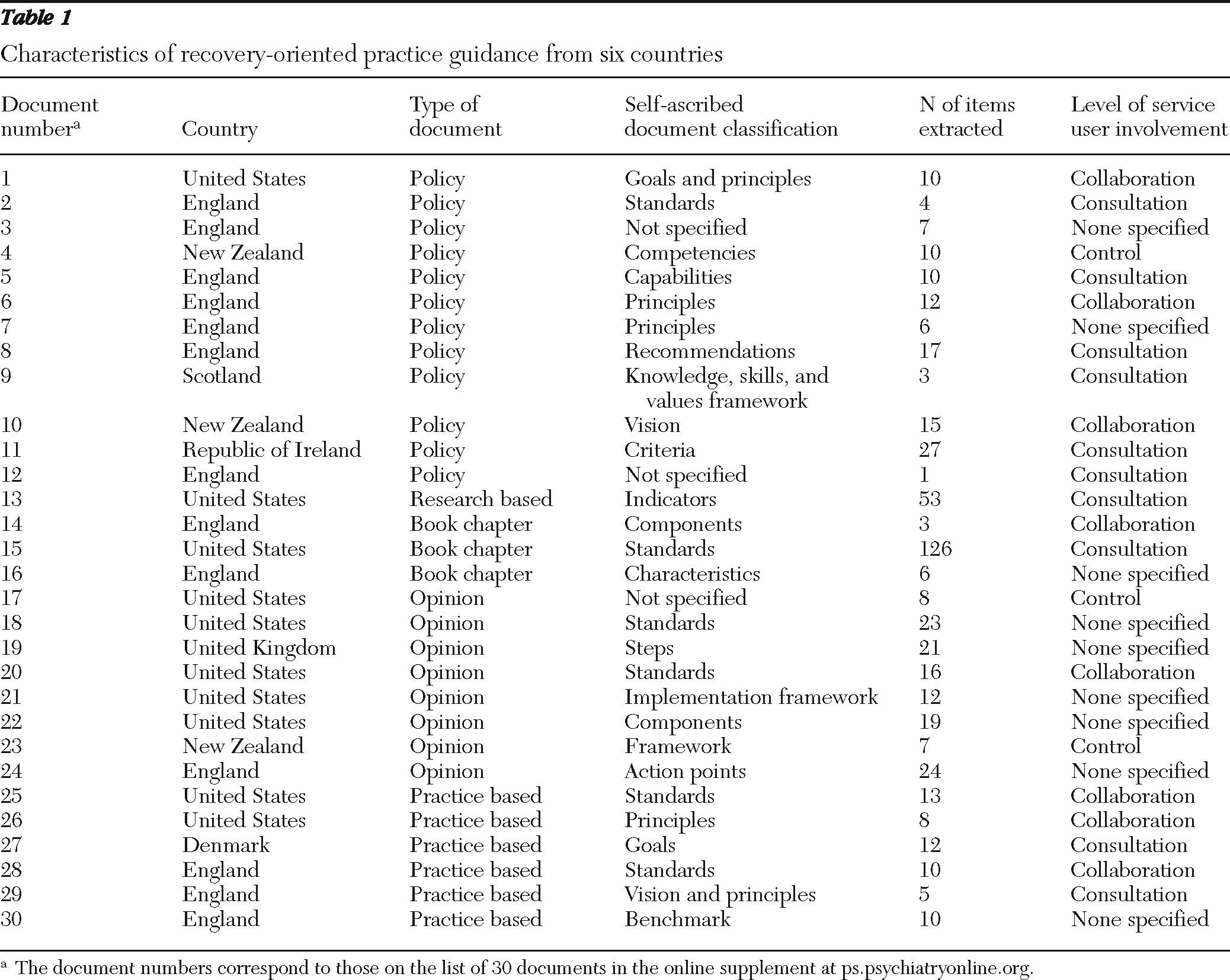
Table 1.
The nature of the guidance was diverse, with 15 self-ascribed categories of guidance. The level of service user involvement in the guideline development varied: user-controlled, N=3; collaboration, N=8; and consultation, N=10.
Aim 1: characteristics of practice guidance
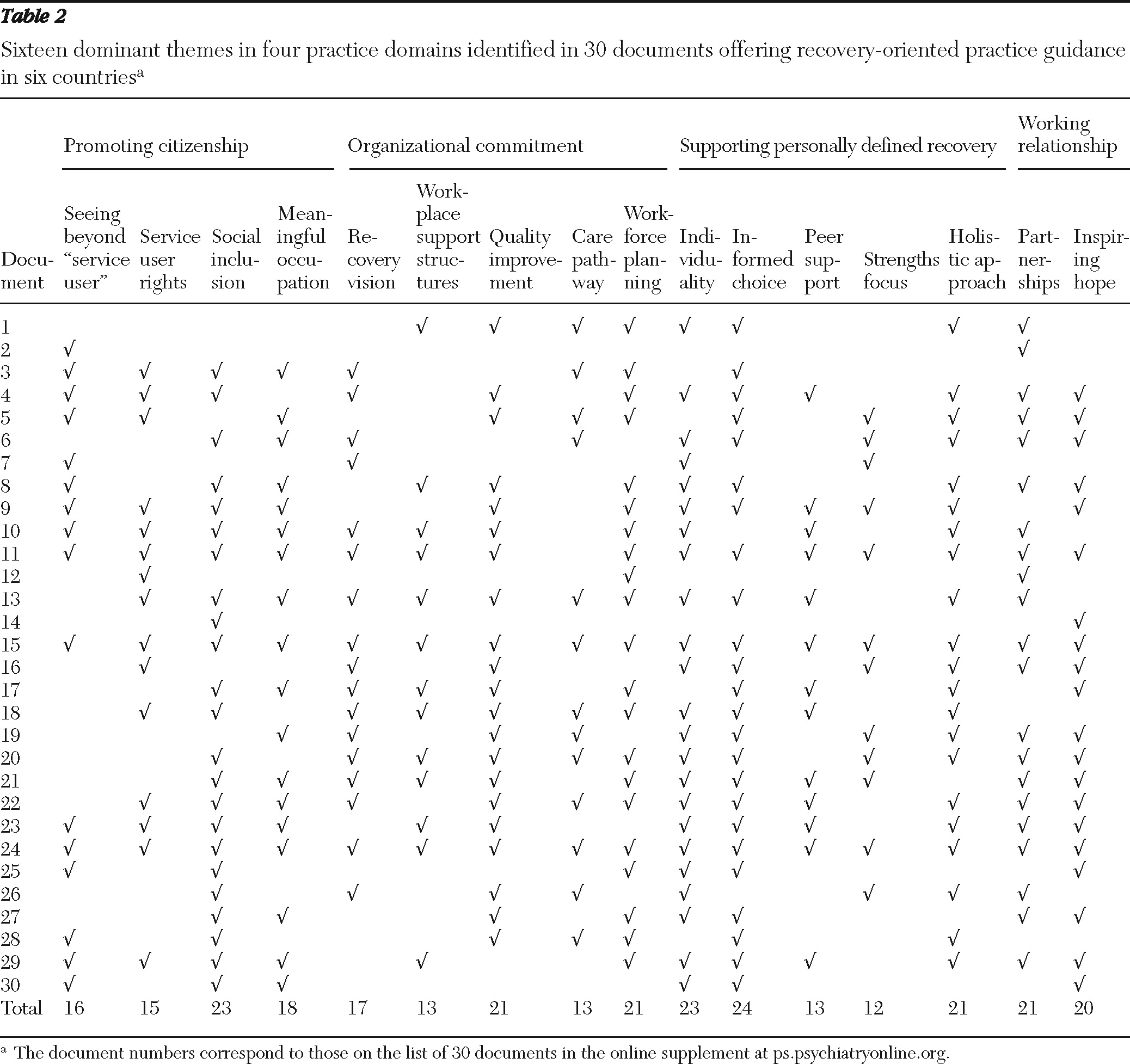
A total of 498 units of text were extracted from the 30 documents. Each unit of text varied in length from one sentence to one paragraph and described one or more components of recovery-oriented practice, resulting in 100 pages of coded data. Inductive semantic thematic analysis identified 16 dominant themes, which are shown in
Table 2 and discussed below. Because of space limitations, subthemes are not specified in this article. [The full conceptual framework is outlined in the online data supplement at
ps.psychiatryonline.org.]
Seeing beyond “service user.”
A shift in within-service attitude from “service user” to person is specified. Individuals who access mental health services are people first and are not defined by their service use or diagnosis. In addition to within-service attitude, societal stigma and discrimination are also challenged.
Service user rights.
The rights of individuals living with mental illness and of families and caregivers are respected. Practitioners have an awareness of human rights issues and are able to refer to or provide advocacy support. Guidance provided in New Zealand addresses this issue (
25). “A competent mental health worker understands and actively protects service users' rights. They demonstrate knowledge of human rights principles and issues … [T]hey demonstrate knowledge of service users' rights within mental health services and elsewhere. … [T]hey demonstrate the ability to promote and fulfil service users' rights.”
Social inclusion.
This theme addresses the improvement in the individual's quality of participation in community life. Practitioners work closely with mainstream organizations and personal social networks to promote opportunities for community integration outside the mental health service. As stated in the guidance from Devon, United Kingdom (
26), “All services demonstrate socially inclusive practice which is supportive of people living ordinary lives in ordinary settings and considers, in particular, peoples' needs for accommodation, occupation, education, personal relationships, money and participation in community life.”
Meaningful occupation.
Individuals are supported to participate in meaningful occupations and to identify a purposeful lifestyle within and beyond the limits of mental illness. Practitioners facilitate decision making about valued life roles and support individuals to create, develop, or maintain their chosen valued roles.
Recovery vision.
Recovery is viewed as the overarching vision of services, and mission and vision statements articulate an organizational commitment to recovery values and practices.
Workplace support structures.
Recovery principles are embedded in existing workplace support structures and give practitioners permission to support recovery values. This agreement is reflected in policies, as well as in contracting and commissioning arrangements that promote recovery philosophies. Guidance from the American Association of Community Psychiatrists (
11) states, “Recovery oriented service design will be reflected in policy and procedure documents, including financial structures that encourage such service development.”
Quality improvement.
Individuals living with mental illness, their families and caregivers, and practitioners are encouraged to make meaningful contributions to the design, delivery, and monitoring of mental health service provision. Central to this theme is the ability of mental health practitioners to support the involvement of service users in quality improvement and to actively encourage service user participation in service development and evaluation.
Care pathway.
Individuals are supported to gain access to and participate in services. Mental health services are encouraged to operate outside usual working hours to allow access by people who work and to support activity in the evenings and on weekends. Nonlinear continuums of care are accepted, and services are designed to allow people to move in and out of the system as required. Services do not exclude people from care on the basis of their symptoms, substance use, or unwillingness to participate in service provision options. Principles of the National Institute of Mental Health England (
27) state, “The user of services decides if and when to begin the recovery process and directs it; therefore, service user direction is essential throughout the process.”
Workforce planning.
Training and staff development is prioritized as an essential function to increase individual practitioners' competencies in recovery-oriented practice and to provide opportunities for staff growth, independence, and wellness. The workforce is representative of the community it serves, and recruitment is guided by recovery values. “Staff can support recovery by … recruiting people with recovery competencies, by interviewing with questions such as ‘Why do you suppose people with mental illness want to work?‘ to give a chance for applicants to demonstrate their values, assessing whether key knowledge, attitudes, and skills about recovery are present” (
28).
Individuality.
Service users' individuality is promoted, and autonomy is supported. Practitioners promote individual preference, self-determination over life, the dignity of risk, and the right to failure.
Informed choice.
Individuals have access to timely and accurate information that provides options and supports personal choice and decision making. Care planning is related to the attainment of personally defined goals and not solely to clinical outcomes. “The service focuses on people's right to make individual decisions or choices about all aspects of their own recovery process, including areas such as the desired goals and outcomes, preferred services used to achieve the outcomes, preferred moments to engage or disengage in services”(
29).
Peer support.
People in recovery are available to model empowerment and to share their own recovery stories to promote learning, self-management, and personal responsibility.
Strengths focus.
The strengths and natural supports of individuals who live with mental illness are acknowledged and encouraged. A strengths model and a discussion of strengths is the central focus of every assessment and care plan. “In addition to the assessment of individual capacities, it is beneficial to explore other areas not traditionally considered ‘strengths,’ e.g., the individual's most significant or most valued accomplishments, ways of relaxing and having fun, ways of calming down when upset, personal heroes, educational achievements, etc.” (
30).
Holistic approach.
A holistic approach is offered that includes a range of options to meet medical, physical, social, occupational, psychological, emotional, spiritual, and religious needs. Individuals are supported to develop a recovery plan that focuses on wellness, the treatments and supports that will facilitate recovery, and the resources that will support the recovery process.
Partnerships.
Individuals who live with mental illness are partners in all aspects of their care. Practitioners provide coaching support to promote autonomy over authority.
Inspiring hope.
Individuals who live with mental illness are valued as experts in their own experience. Practitioners value and believe in service users' abilities and foster hope and optimism in their work. “The system is grounded in a belief that recovery is possible and is expected outcome of treatment” (
31).
Aim 2: develop a conceptual framework
Interpretive analysis was undertaken to group the themes into practice domains by identifying connections and relationships between themes. Four overarching conceptual practice domains were identified: promoting citizenship, organizational commitment, supporting personally defined recovery, and working relationship. Each practice domain is as important as the next, and there is no hierarchical order. The grouping of themes and distribution of themes across documents is shown in
Table 2. Informed choice was the most prominent theme, appearing in the extracted data of 24 of the 30 documents. Representation of themes across documents is apparent; of potential interest is the recognition of an organizational perspective in data from the documents in which service users played a leading role.
The four practice domains are described below in further detail.
Promoting citizenship.
The core aim of services is to support people who live with mental illness to reintegrate into society and to live as equal citizens. Citizenship is central to supporting recovery, in which the right to a meaningful life for people living with severe and enduring mental illness is advocated. Seeing beyond “service user,” service user rights, social inclusion, and meaningful occupation are grouped in this practice domain.
Organizational commitment.
Organizations that support recovery orientation demonstrate a commitment to ensure that the work environment and service structure are conducive to promoting recovery-oriented practice. The organizational culture gives primacy to recovery and focuses on and adapts to the needs of people rather than those of services. Recovery vision, workplace support structures, quality improvement, care pathway, and workforce planning are included in this practice domain.
Supporting personally defined recovery.
Practitioners focus on supporting personally defined recovery and view recovery as being at the heart of practice and not as an additional task. Individuals are supported to define their own needs, goals, dreams, and plans for the future to shape the content of care. Individuality, informed choice, peer support, strengths focus, and holistic approach are contained in this practice domain.
Working relationship.
Practitioner interactions demonstrate a genuine desire to support individuals and their families to fulfill their potential and to shape their own future. A therapeutic relationship is essential to supporting recovery in which partnership working and hope is promoted.
Discussion
The goals of this study were to determine the characteristics of recovery-oriented practice guidance on the basis of current international perspectives and to develop an overarching conceptual framework that can be used to aid the translation of recovery guidance into clinical practice. A conceptual framework was developed by using inductive thematic analysis, which identified four practice domains: promoting citizenship, organizational commitment, supporting personally defined recovery, and working relationship.
Implications for policy and practice
The emerging conceptual framework is wide ranging, encompassing sociopolitical involvement and ethical responsibilities that may be outside the usual sphere of practice. Davidson (
7) argued for a conceptual framework that supports the fundamental role of independence and self-determination in enabling people who live with mental illness to exercise their rights of citizenship and to live meaningful lives. The view that promoting citizenship is the job of the mental health system may be challenging. It suggests that “becoming social activists who challenge stigma and discrimination, and promoting societal well-being may need to become the norm rather than the exception for mental health professionals in the 21st Century” (
32).
The involvement of organizations is also highlighted (
33), pointing to the need to develop a whole-systems approach. To operate within a recovery framework, services need to balance the tension between addressing both the priorities of service users and the wider expectations of the community (
18). Addressing organizational commitment may be difficult, because it challenges the view that the organization merely provides the infrastructure for service delivery and quality assurance. This raises questions about the purpose of mental health services and how their effectiveness should be evaluated (
34).
The process of supporting personally defined recovery reflects the complexity and dimensions of practice across both evidence-based practice and illness experience. This is enhanced by working relationships that recognize the value of therapeutic and real relationships (
6). Although the understanding of recovery-oriented practice is still developing, practices that are reflective of the four practice domains should be promoted (
7,
35).
There is an expectation that practitioners embed a recovery framework in their existing perspectives of disability and health (
3,
36). The conceptual framework can be used to address this need. One example is viewing recovery-oriented practice within an ecological perspective (
37), where the life context, the environment, and the relationship between individuals and their environment are considered (
14,
30). The conceptual framework promotes awareness of the impact of ecological factors, such as health care systems and societal and life context, on recovery (
38).
The conceptual framework can be used to aid the understanding and translation of recovery-oriented practice guidance into practice. Although the conceptual framework provides a conceptual overview built from robust analysis, it is not a definitive guide. The complexity of translating recovery into practice dictates the need for context-specific guidance. The synthesis of guidance provides a foundation for structuring local guidelines and future policy (
3), benchmarking recovery-oriented practice (for example, for developing an accreditation process for services (
39), and supporting staff development within existing practice competencies (
40).
Strengths and limitations
This study considered a broad range of documents to explore the breadth of recovery-oriented practice, and although the sample size was influenced by what was considered feasible for a qualitative analysis, it is substantially larger than is usual for a study of this type. Robust qualitative methodology was used to maximize the quality of the synthesis. The main limitation is the nonsystematic approach to identifying the guidance documents. The rationale for analyzing widely used documents is that recovery orientation is a developing area of research and practice, and its evolving meaning is both represented and influenced by prominent policy and practice documents. The literature search was a systematized review rather than a systematic review (
41); therefore, not all existing guidance documents were identified in the search, which resulted in reduced coverage of important guidance, for example, from Canada (
42) and Australia (
43). Informal analysis indicates that these documents are consistent with our findings, but the conceptual framework should be considered a heuristic to be further developed and refined.
Future research
The diversity of guidance highlights the complexity of translating recovery into practice. Future research to apply the conceptual framework in practice and to develop associated quality indicators would begin to bridge this gap (
44). A second strand of research will be empirical investigation of the relationship between practices and outcomes associated with personal recovery and clinical recovery (
39). A third strand will involve collation of more guidance developed by service users for comparative analysis to identify different emphases in user controlled guidance.
Despite the attention to practice guidelines and practitioner attitudes (
15) and research on recovery experiences of individuals receiving mental health services (
45), research on the implementation experiences of persons providing mental health services is a relatively unexplored area in need of further development (
46–
49). Although practice guidance exists, a translational gap between knowledge and routine implementation in mental health practice has been cited as a major challenge to innovation in mental health care (
50,
51). Recent advances in recovery research measure fidelity to a specific recovery intervention (
52–
54). A fourth strand will be research to address the translational gap in order to enhance implementation efforts (
2,
12).
Conclusions
A key challenge for mental health services is the lack of clarity about what constitutes recovery-oriented practice. This synthesis of guidance contributes to the understanding of recovery orientation, and the resulting conceptual framework can be used to aid the translation of recovery-oriented guidance into practice.
Acknowledgments and disclosures
This study was conducted within the larger REFOCUS study, which is funded by a five-year Programme Grant for Applied Research from the National Institute for Health Research (NIHR) (NIHR reference RP-PG-0707-10040) awarded to South London and Maudsley National Health Service (NHS) Foundation Trust, and in relation to the NIHR Specialist Mental Health Biomedical Research Centre at the Institute of Psychiatry, King's College London. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
The authors report no competing interests