Among its many imperatives, the Decade of the Brain issues a call to psychiatrists to become brain smart at a level of sophistication beyond what contemporary psychiatric education provides.
1 Synaptic and intraneuronal physiology and molecular biology, particularly as they relate to neurotransmitter function, have been the mainstays of neurobiology curricula in psychiatry residency in the latter part of this century. These subjects have been emphasized primarily because the effectiveness of psychotropic medication created a need to know the scientific basis of psychopharmacology. In the past several years, however, regional brain findings of disturbed structure and function in major mental illness and the demonstration of focal brain effects of psychotropic drugs and psychotherapy
2 have established a mandate for renewed study by psychiatrists of neuroanatomy. We suggest that braincutting, tailored to psychiatrists-in-training, be the centerpiece of this educational endeavor.
To grasp fully the neuroscientific developments that increasingly inform clinical psychiatry practice, it is advantageous to be able to picture, in 3-D space, anatomical interrelationships within the brain. A positron emission study of obsessive-compulsive disorder (OCD) by Baxter et al.
3 provides a vivid example of how gross anatomic demonstration of these relationships can help students master conceptually complex neuroscientific material. Baxter et al. determined that pharmacological or psychotherapeutic interventions, when effective in OCD, had a normalizing effect on glucose metabolism in the right caudate nucleus. Furthermore, both types of therapy, when they had a salutory effect on symptoms, broke up an abnormal synchrony of metabolic rates between orbitofrontal cortex, caudate, and thalamus that the study had identified in patients with symptomatic OCD.
These results lend credence to the idea that patients with OCD are caught in a reverberating thought/behavior loop associated with a heightened interrelationship between brain regions that normally operate more independently. Brain dissection will reveal to the student the array in space of the orbitofrontal cortex, caudate nucleus, and thalamus, and their proximity to one another, and thereby help make sense of the interconnections between them. As well, such a demonstration can provide a tangible representation with which to engage the work of Alexander et al.
4 These researchers introduced an integrated conception of parallel cortical-striatal-thalamic-cortical circuits that provides some of the theoretical underpinnings of contemporary models of OCD
5 and that may also have relevance in schizophrenia.
6 Braincuttings will also enhance understanding of several other emerging brain findings, including those bearing on fear systems in humans
7 and other species,
8 mood disorders,
9 and addiction disorders.
10These regional brain scenarios relevant to psychiatric disorders, and the anatomical interrelationships of the regions involved, are not appreciated easily by students of psychiatry who are products of traditional medical training. The medical school neuroanatomy class usually does not emphasize behavioral neuroanatomy, nor is there often a venue for this in graduate medical training. Psychiatrists need to learn where behaviorally relevant brain regions are with respect to one another and to comprehend the hodological relationships between the regions. It is our belief that this material is best brought alive when psychiatry residents are confronted in clinical training with the disorders associated with brain dysfunction.
With that in mind, the Psychiatry, Psychology, and Neuropathology Departments and the Center for Cognitive Neuroscience at Dartmouth Medical School and Dartmouth College developed a brain anatomy curriculum that is built around a braincutting for psychiatry residents. Our intent in this article is to describe the curriculum in the hope of galvanizing similar developments at other training sites, and also to provide a template of the anatomical material to be mastered by psychiatrists who wish to train themselves in neuroanatomy.
We are not aware of any published reports of braincuttings tailored to the education of psychiatrists. Furthermore, having canvassed several other psychiatry departments at major university medical centers in the United States,
11 we believe that very few psychiatry residencies currently offer this exercise. Some residencies we polled offered braincuttings, but in each case they consisted of making available to psychiatry trainees attendance at traditional braincuttings sponsored by departments of neuropathology, neurology, or neurosurgery. These braincuttings are oriented toward neurological lesions. When normal neuroanatomy is reviewed, the focus is most often on features such as the neurocirculatory system and where cranial nerves exit the brain—anatomy that is usually more relevant to neurological than psychiatric conditions. Although the basics of neuroanatomy and lesion study are essential for all students of the brain, including psychiatrists, traditional braincuttings are not constructed with the education of psychiatrists specifically in mind. Braincutting has had a venerable and time-honored role in the training of neurologists, neurosurgeons, and neuropathologists. The Decade of the Brain invites this laboratory exercise, with an added emphasis on behavioral neuroanatomy, into psychiatric training.
The psychiatry residency behavioral neuroanatomy curriculum at Dartmouth Medical School consists of a seminar series followed by a braincutting. The braincutting will be reviewed first, since it is the principal emphasis in this communication.
THE BRAINCUTTING
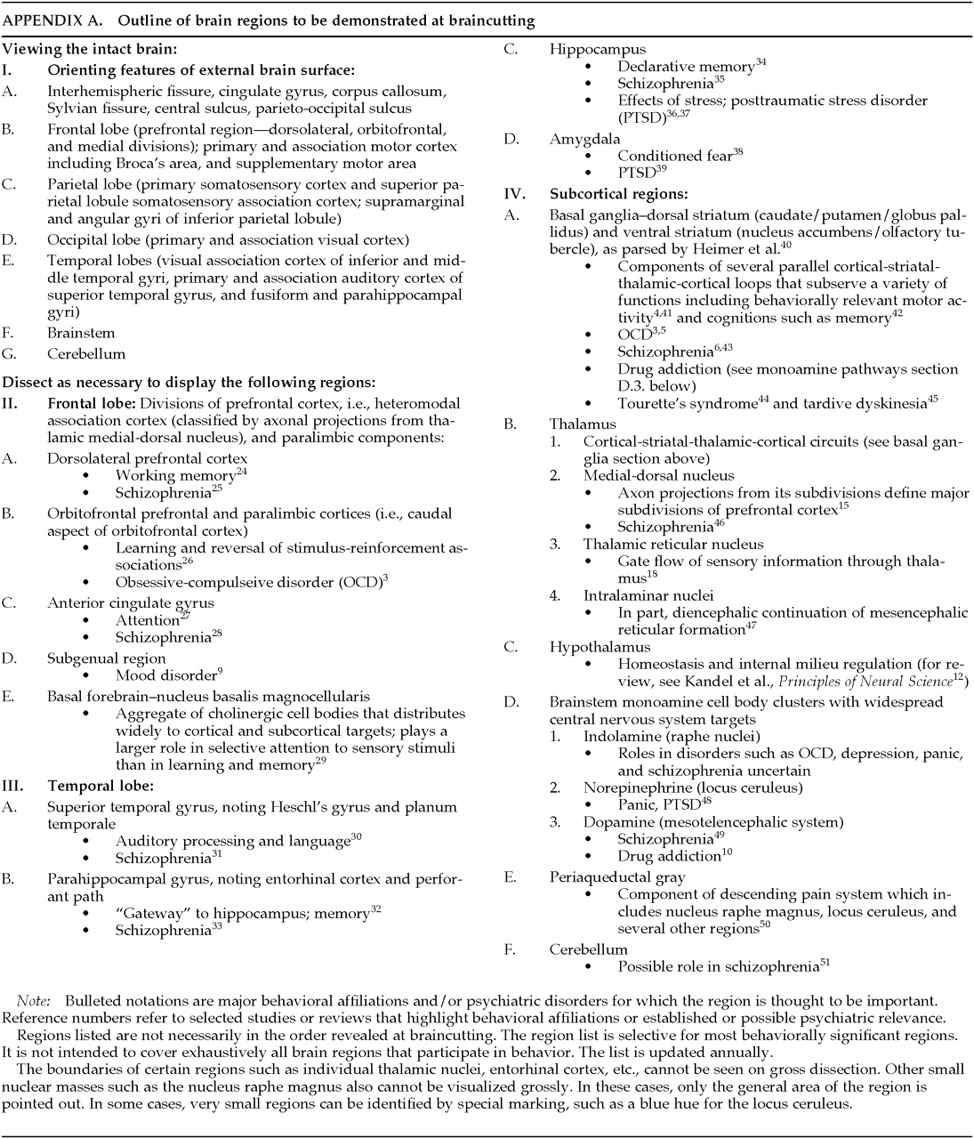
One of the authors (R.G.), provides the neuropathologist (W.H.) with a list of regions to be demonstrated. The regions selected are those with behavioral affiliations most pertinent to the study of psychiatric disorders. The regions that are included, their major behavioral affiliations, and their known or theoretical roles in major mental disorders are listed in
Appendix A. The teaching personnel include a neuropathologist (W.H.), a psychiatrist (R.G.), and a psychologist (A.C.). Although we have not yet included a neuroradiologist, doing so would provide valuable input. The students for each session are eight psychiatry residents. Materials on hand:
1.
A lightbox-displayed set of T1-weighted coronal magnetic resonance images (MRI; 3 mm thick, no gaps), through a normal whole brain, as well as midsagittal and selected axial images from the same brain.
2.
Two normal postmortem brains, one of which is intact and the other pre-dissected, with the regions listed in the
Appendix flagged.
3.
Color reprints of plates that show structural and functional imaging findings in studies reviewed during the seminar series preceding the braincutting.
4.
Microscopic slides of tissue from several regions listed in the
Appendix.The neuropathologist dissects the intact brain exposing and demonstrating the regions listed in the
Appendix, and, when helpful, cross-references the pre-dissected flagged regions and the MRIs. As each region is exposed, the neuropathologist reviews anatomical features of the region and the psychiatrist and psychologist provide brief descriptions of its anatomical and functional relationships with other regions, behavioral affiliations, and theoretical or known roles in one or more major mental illnesses. Color plates are displayed from studies showing recent psychiatrically relevant findings. It is emphasized that these regions are not “centers” for specific activities, but rather nodes in the complex circuitry that underlies behavior. The format is interactive with the resident participants, and an effort is made to be sure that all participants master the relationships between regions. Students are encouraged to handle and examine for themselves all dissected sections. The demonstration lasts three and a half hours, with two brief breaks.
THE SEMINAR THAT PRECEDES THE BRAINCUTTING
We have found from experience that a braincutting is best preceded by didactic seminars, since the nomenclature and neuroanatomy involved are sufficiently complex that they cannot be learned for the first time at a braincutting. The seminar series, 12 weekly 90-minute sessions, is a slide and plastic model–assisted behavioral neuroanatomy tour. The major source materials are selected chapters from Kandel and colleagues'
Principles of Neural Science;
12 Mesulam's
Principles of Behavioral Neurology;
13 Nieuwenhuys and colleagues'
The Human Central Nervous System: A Synopsis and Atlas;
14 a slide set of the coronal, midsagittal, and axial MRIs described in the Braincutting section; and an annually updated bibliography including selections from this article's reference list. Because the major emphasis of this paper is to highlight the role of braincutting, the seminar series will be summarized here rather than set forth in detail. The full course syllabus is available on request.
The behavioral brain tour uses as its basis and guide the routes by which information is processed by the brain. As each region is encountered, its interconnections and participation in behaviorally relevant circuitry are discussed.
The tour begins with an orientation to the gross features, as listed in the
Appendix, of the external surface of the brain, employing a plate from Mesulam
13 that displays a lateral view of the external surface of the left hemisphere. The plate color-codes primary, association, and paralimbic cortices.
In keeping with the strategy of basing the brain tour on the sequences in which the brain processes information, the regional tour begins with the thalamus. (Although sensory processing peripheral to the thalamus does bear on higher order processing and behavior, the course focuses attention primarily on the central nervous system.) In considering the thalamus, we review its relationship with other subcortical regions and its function as a major relay for sensory (including reticular formation) input to the cerebral cortex. We emphasize:
1.
Participation of thalamic nuclei in cortical-striatal-thalamic-cortical circuits that may have relevance in OCD
3,5 and schizophrenia.
62.
Axonal projections from the mediodorsal nucleus that define the major morphologic subdivisions of the prefrontal cortex.
153.
For historical reasons, the way-stations of the Papez circuit (which includes the anterior thalamic nuclei)
16 and the fact that Papez's belief that the circuit primarily processed emotion has proved incorrect.
174.
The gating functions of the thalamic reticular nucleus.
185.
Thalamic input to the amygdala.
196.
The absence of thalamic processing of olfactory information.
This outline of what the course covers with respect to the thalamus is meant to convey a sense of the type of information discussed for each of the other regions, which we do not have space to describe in this report. The following is a brief review of the sequence of the subsequent regions toured.
After considering the thalamus, we move to three thalamic cortical targets: the primary auditory, visual, and somatosensory cerebral cortices, and their respective unimodal association cortices. Although for the most part these regions have not emerged to date as associated significantly with major psychiatric disorders (an exception is the linkage of auditory association cortex and auditory hallucinations
20), they are nonetheless included in the brain tour, since sensory information processing provides an instructive model for how the brain manages information. This knowledge proves helpful in understanding how the brain governs more complex behavioral functions. We then consider the two major heteromodal association cortices, prefrontal and parietotemporal, and their morphologic/functional subdivisions in each hemisphere.
We next turn to medial paralimbic and corticoid regions: cingulate gyrus, parahippocampal gyrus, hippocampus, amygdala, and subcortical regions including the hypothalamus and dorsal and ventral striatum. Finally, we review the cerebellum and brainstem regions, including the periaqueductal gray, and the major aggregates of monoamine cell bodies along with their subcortical and cortical targets.
The tour is intended in part to prepare residents for the braincutting. Since one of the goals of this course is to impart a 3-D appreciation of psychiatrically relevant neuroanatomy, many aspects of the peripheral sensory and voluntary motor systems are not considered. Neither is an effort made to consider the anatomy involved in neurological syndromes such as stroke. However, the anatomy underlying focal neurological syndromes that present primarily with behavioral symptoms such as prosopagnosia are discussed, as are classic “neurology” cases that illustrate behaviorally relevant neuroanatomy, such as those of Phineas Gage
21,22 and H.M.
23At each session, the material covered in the preceding session is reviewed. We have found that inculcating this material requires repeating it over and over for even the brightest and most inquisitive students. The current configuration of the course is based on informal feedback from faculty and students about earlier iterations.
In summary, the brain tour and braincutting curriculum at Dartmouth Medical School should be feasible in any department of psychiatry that can affiliate with departments of neuropathology and neuroradiology and with neuroscience-oriented psychology departments. The course was designed to meet a contemporary need for psychiatrists to learn behaviorally relevant neuroanatomy. This familiarity will enhance understanding of emerging neuroscientific developments in psychiatry and will thereby bring important available knowledge into the practice of clinical psychiatry. As an example, appreciating behavioral neuroanatomy will enhance our ability to explain more clearly, with diagrams and illustrations, to increasingly informed patients, the nature of the illnesses that plague them and how the psychological and pharmacological interventions we propose are thought to work.
ACKNOWLEDGMENTS
This work was supported by the National Alliance for Research on Schizophrenia and Depression; Mr. William Martens, Jr.; Mr. and Mrs. Robert Boyajian; Mr. and Mrs. James Winston (R.G.); National Institutes of Health awards DA08574 (A.C.) and NS17778 (M.G., J.H.); and Office of Naval Research award N00014-89-J-3035 (M.G., J.H.).